J Korean Ophthalmol Soc.
2017 Jun;58(6):731-735. 10.3341/jkos.2017.58.6.731.
One Step Operation of the Persistent Pupillary Membrane Removal and Cataract Operation: A Case Report
- Affiliations
-
- 1Department of Ophthalmology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. sonicnet@hanmail.net
- KMID: 2382684
- DOI: http://doi.org/10.3341/jkos.2017.58.6.731
Abstract
- PURPOSE
We report a case of one-step operation of persistent pupillary membrane removal, phacoemulsification, and posterior chamber lens implantation that was performed in a patient with persistent pupillary membrane and brunescent cataracts in both eyes.
CASE SUMMARY
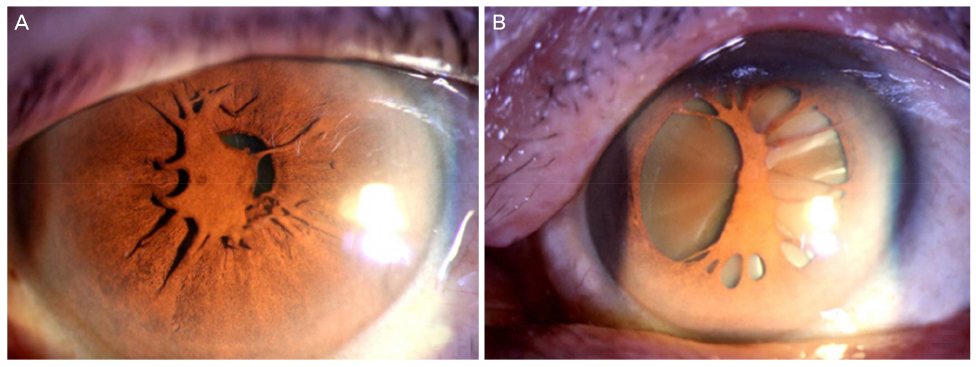
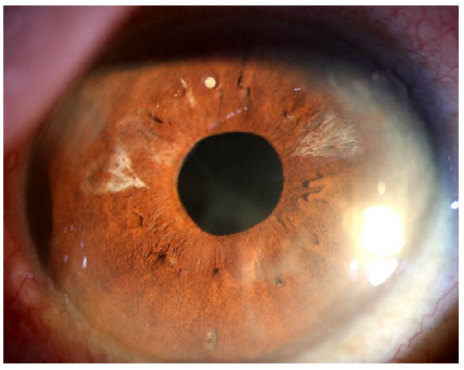
A 64-year-old male with no baseline disease visited our clinic with bilateral decreased visual acuity. His best corrected visual acuity at first visit was 0.1 in the right eye and 0.2 in the left eye. On anterior segment examination, both bilateral persistent pupillary membranes and brunescent cataracts were observed. First, we surgically removed the left pupillary membrane and performed phacoemulsification using posterior chamber lens implantation via one-stage operation. After one week, the same operation was performed for the right eye using the same method. At 6-months postoperative, his best corrected visual acuity was 0.2 in the right eye and 0.8 in the left eye. No complications such as anterior segment inflammation, uveitis, or intraocular pressure elevation were observed during the follow-up period.
CONCLUSIONS
We report a case of one-step operation of persistent pupillary membrane removal and cataract operation, which can improve visual acuity without any complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Kraus CL, Lueder GT. Clinical characteristics and surgical approach to visually significant persistent pupillary membranes. J AAPOS. 2014; 18:596–599.2. Lambert SR, Buckley EG, Lenhart PD, et al. Congenital fibrovascular pupillary membranes: clinical and histopathologic findings. Ophthalmology. 2012; 119:634–641.3. Ko J, Jung JW, Kim EK. Two-stage operation for the treatment of cataract associated with persistent pupillary membrane. J Cataract Refract Surg. 2013; 39:1615.4. Wang JK, Wu CY, Lai PC. Sequential argon-YAG laser membranectomy and phacoemulsification for treatment of persistent pupillary membrane and associated cataract. J Cataract Refract Surg. 2005; 31:1661–1663.5. Vega LF, Sabates R. Neodymium: YAG laser treatment of persistent pupillary membrane. Ophthalmic Surg. 1987; 18:452–454.6. Kumar H, Sakhuja N, Sachdev MS. Hyperplastic pupillary membrane and laser therapy. Ophthalmic Surg. 1994; 25:189–190.7. Mansour AM, Hamade I, Antonios RS. Sequential argon-YAG laser membranotomy of extensive persistent pupillary membrane with visual loss. BMJ Case Rep. 2015; 2015:pii: bcr2015210140.8. Kesarwani S, Murthy R, Vemuganti GK. Surgical technique for removing congenital fibrovascular pupillary membrane, with clinicopathological correlation. J AAPOS. 2009; 13:618–620.