J Korean Ophthalmol Soc.
2017 Jun;58(6):698-705. 10.3341/jkos.2017.58.6.698.
Range of Eye Movement in a Normal Population and Its Relationship to Age
- Affiliations
-
- 1Department of Ophthalmology, Hanyang University Seoul Hospital, Hanyang University College of Medicine, Seoul, Korea. limhw@nate.com
- KMID: 2382679
- DOI: http://doi.org/10.3341/jkos.2017.58.6.698
Abstract
- PURPOSE
The purpose of this study is to measure the range of normal eye movement and to evaluate the effect of age on the range of ocular movement in a normal population.
METHODS
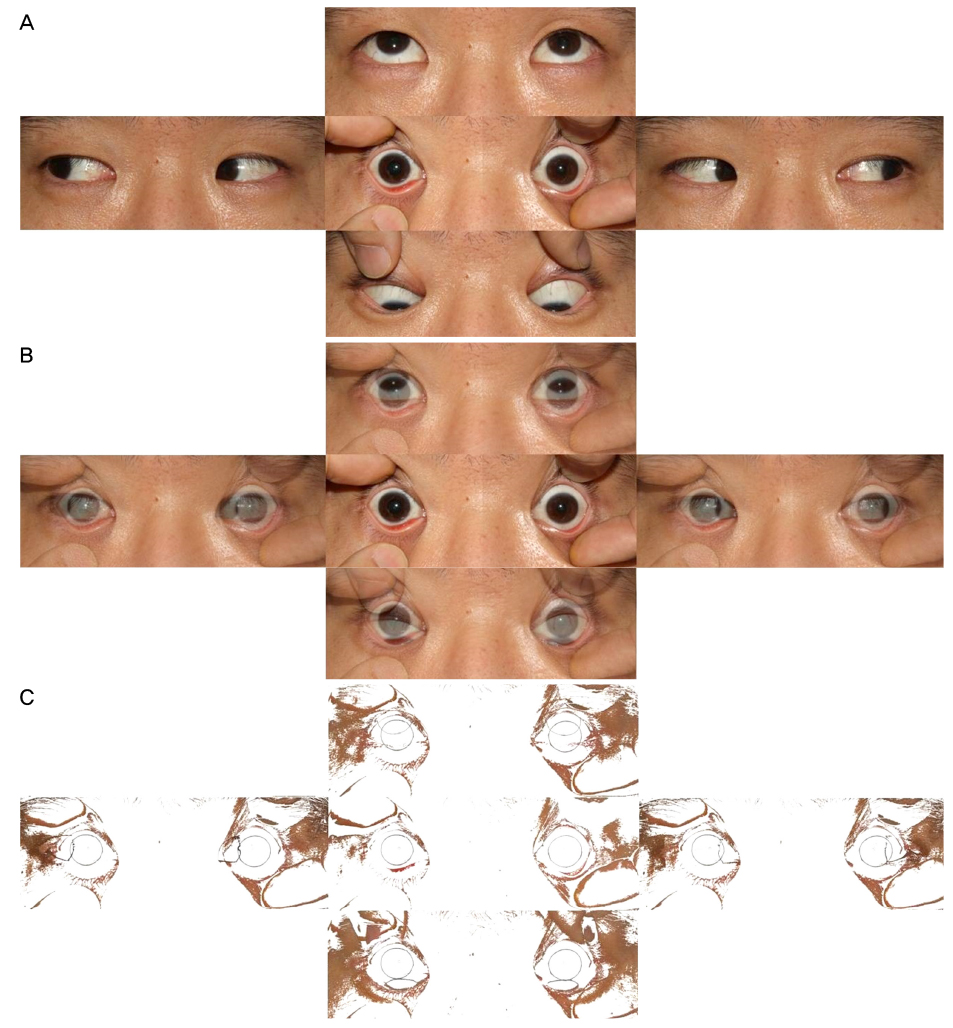
We conducted a prospective observational study of 85 subjects aged between 5 and 91 years. Photographs were taken of the cardinal position, and these images were analyzed using an image analysis software (Adobe Photoshop 6.0, Adobe, San Jose, CA, USA). To measure the range of eye movement, the preprocessed images were analyzed using the Image J program. The range of movement of the eyeball was quantitatively measured using corneal limbal analysis. Specifically, the ranges of ocular movement according to adduction, abduction, elevation, and depression were measured.
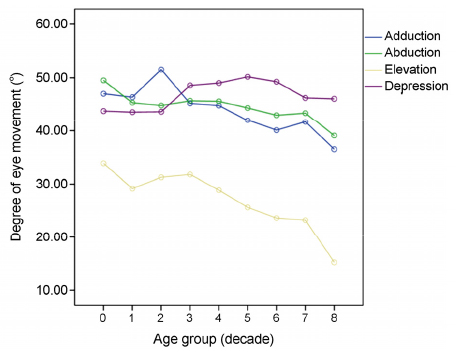
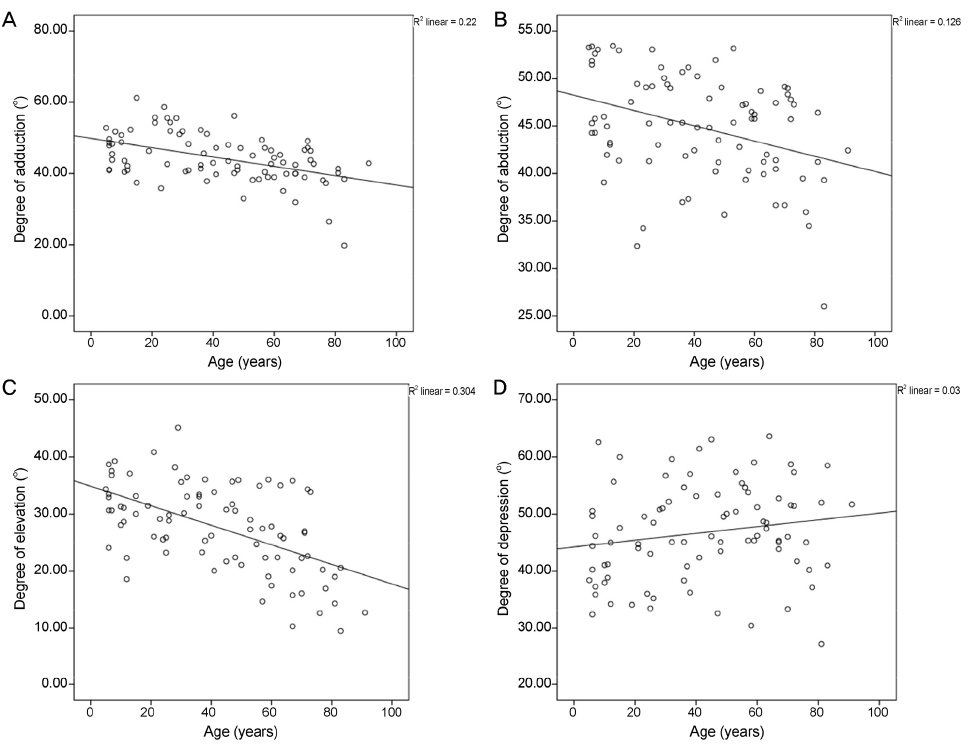
RESULTS
The normal movement ranges were 44.4 ± 6.9° in adduction, 44.8 ± 5.5° in abduction, 27.7 ± 7.6° in elevation, and 46.7 ± 8.4° in depression. Adduction, abduction, and elevation were negatively correlated with age (R² = 0.220, R² = 0.126, and R² = 0.304, respectively, all p < 0.001). However, there was no significant correlation between age and depression (R² = 0.030, p = 0.113).
CONCLUSIONS
For all ages, the range of normal ocular movement in the horizontal direction was symmetric, while the range of ocular movement in elevation was smaller than that of depression. As age increased, the range of ocular movement decreased in all directions except depression, but depression did not decrease with age. When assessing eye movement, it is necessary to consider the range of ocular movements relative to both the movement direction and changes in the ocular movement range according to age.
Keyword
Figure
Reference
-
1. Leigh RJ, Zee DS. The Neurology of Eye Movements. 4th ed. New York: Oxford University Press;2006.2. Jacobs RJ. Visual resolution and contour interaction in the fovea and periphery. Vision Res. 1979; 19:1187–1195.3. Ramat S, Leigh RJ, Zee DS, Optican LM. What clinical disorders tell us about the neural control of saccadic eye movements. Brain. 2007; 130(Pt 1):10–35.4. Clark RA, Isenberg SJ. The range of ocular movements decreases with aging. J AAPOS. 2001; 5:26–30.5. Mourits MP, Prummel MF, Wiersinga WM, Koorneef L. Measuring eye movements in Graves ophthalmopathy. Ophthalmology. 1994; 101:1341–1346.6. Gerling J, Lieb B, Kommerell G. Duction ranges in normal probands and patients with Graves’ ophthalmopathy, determined using the Goldmann perimeter. Int Ophthalmol. 1997-1998; 21:213–221.7. Chamberlain W. Restriction in upward gaze with advancing age. Am J Ophthalmol. 1971; 71(1 Pt 2):341–346.8. Haggerty H, Richardson S, Mitchell KW, Dickinson AJ. A modified method for measuring uniocular fields of fixation: reliability in healthy subjects and in patients with Graves orbitopathy. Arch Ophthalmol. 2005; 123:356–362.9. Dolman PJ, Cahill K, Czyz CN, et al. Reliability of estimating ductions in thyroid eye disease: an International Thyroid Eye Disease Society multicenter study. Ophthalmology. 2012; 119:382–389.10. Lim HW, Lee DE, Lee JW, et al. Clinical measurement of the angle of ocular movements in the nine cardinal positions of gaze. Ophthalmology. 2014; 121:870–876.11. Huaman AG, Sharpe JA. Vertical saccades in senescence. Invest Ophthalmol Vis Sci. 1993; 34:2588–2595.12. van der Geest JN, Frens MA. Recording eye movements with video-oculography and scleral search coils: a direct comparison of two methods. J Neurosci Methods. 2002; 114:185–195.13. Houben MM, Goumans J, van der Steen J. Recording three-dimensional eye movement: scleral search coils versus video oculography. Invest Ophthalmol Vis Sci. 2006; 47:179–187.14. Frens MA, van der. Scleral search coils influence saccade dynamics. J Neurophysiol. 2002; 88:692–698.15. Smeets JB, Hooge IT. Nature of variability in saccades. J Neurophysiol. 2003; 90:12–20.16. Lim HW, Lee JW, Hong E, et al. Quantitative assessment of inferior oblique muscle overaction using photographs of the cardinal positions of gaze. Am J Ophthalmol. 2014; 158:793–799.e2.17. Yang HK, Seo JM, Hwang JM, Kim KG. Automated analysis of binocular alignment using an infrared camera and selective wavelength filter. Invest Ophthalmol Vis Sci. 2013; 54:2733–2737.18. Yoon CK, Yang HK, Kim JS, Hwang JM. An objective photographic analysis of ocular oblique muscle dysfunction. Am J Ophthalmol. 2014; 158:924–931.19. Campbell WW, DeJong RN. DeJong's the neurologic examination. 6th ed. Philadelphia: Lippincott Williams & Wilkins;2006.20. Urist MJ. A lateral version light-reflex test. Am J Ophthalmol. 1967; 63:808–815.21. Bos JE, de Graaf B. Ocular torsion quantification with video images. IEEE Trans Biomed Eng. 1994; 41:351–357.22. Frohman TC, Galetta S, Fox R, et al. Pearls & Oy-sters: the medial longitudinal fasciculus in ocular motor physiology. Neurology. 2008; 70:e57–e67.23. Serra A, Liao K, Matta M, Leigh RH. Diagnosing disconjugate eye movements: phase-plane analysis of horizontal saccades. Neurology. 2008; 71:1167–1175.24. Oguro H, Okada K, Suyama N, et al. Decline of vertical gaze and convergence with aging. Gerontology. 2004; 50:177–181.25. Koornneef L. Eyelid and orbital fascial attachments and their clinical significance. Eye (Lond). 1988; 2(Pt 2):130–134.26. Miller JM. Functional anatomy of normal human rectus muscles. Vision Res. 1989; 29:223–240.27. Horn AK. The reticular formation. Prog Brain Res. 2006; 151:127–155.28. Hepp K, Henn V. Spatio-temporal recoding of rapid eye movement signals in the monkey paramedian pontine reticular formation (PPRF). Exp Brain Res. 1983; 52:105–120.29. Fukushima K. The interstitial nucleus of Cajal in the mid-brain reticular formation and vertical eye movement. Neurosci Res. 1991; 10:159–187.30. Brody H, Vijayashankar N. Anatomical changes in the nervous system. In : Finch CE, Hayflick L, editors. Handbook of the Biology of Aging. New York: Van Nostrand;1977. p. 241–261.31. Vijayashankar N, Brody H. Neuronal population of human abducens nucleus. Anat Record. 1971; 169:447.32. Clark RA, Demer JL. Effect of aging on human rectus extraocular muscle paths demonstrated by magnetic resonance imaging. Am J Ophthalmol. 2002; 134:872–878.