J Adv Prosthodont.
2017 Jun;9(3):176-181. 10.4047/jap.2017.9.3.176.
Evaluation of marginal and internal gaps of Ni-Cr and Co-Cr alloy copings manufactured by microstereolithography
- Affiliations
-
- 1Department of Dental Laboratory Science and Engineering, College of Health Science, Korea University, Seoul, Republic of Korea. kuc2842@korea.ac.kr
- 2Department of Dental Laboratory Science and Engineering, College of Health Science & Department of Public Health Sciences, Graduate School & BK21+ Program in Public Health Sciences, Korea University, Seoul, Republic of Korea.
- KMID: 2382603
- DOI: http://doi.org/10.4047/jap.2017.9.3.176
Abstract
- PURPOSE
The purpose of this study was to evaluate the marginal and internal gaps of Ni-Cr and Co-Cr copings, fabricated using the dental µ-SLA system.
MATERIALS AND METHODS
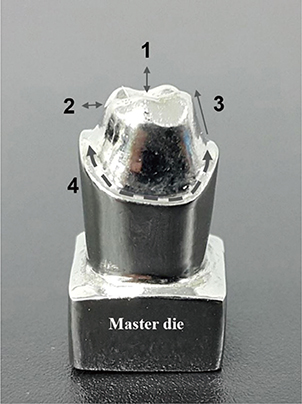
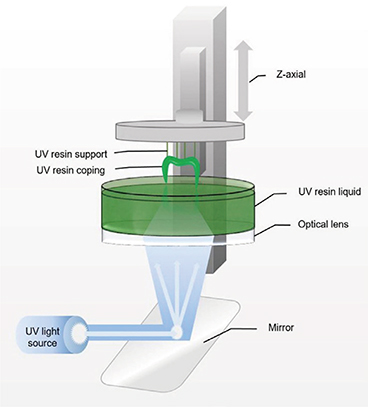
Ten study dies were made using a two-step silicone impression with a dental stone (type IV) from the master die of a tooth. Ni-Cr (NC group) and Co-Cr (CC group) alloy copings were designed using a dental scanner, CAD software, resin coping, and casting process. In addition, 10 Ni-Cr alloy copings were manufactured using the lost-wax technique (LW group). The marginal and internal gaps in the 3 groups were measured using a digital microscope (160 ×) with the silicone replica technique, and the obtained data were analyzed using the non-parametric Kruskal-Wallis H test. Post-hoc comparisons were performed using Bonferroni-corrected Mann-Whitney U tests (α=.05).
RESULTS
The mean (±standard deviation) values of the marginal, chamfer, axial wall, and occlusal gaps in the 3 groups were as follows: 81.5±73.8, 98.1±76.1, 87.1±44.8, and 146.8±78.7 µm in the LW group; 76.8±48.0, 141.7±57.1, 80.7±47.5, and 194.69±63.8 µm in the NC group; and 124.2±52.0, 199.5±71.0, 67.1±37.6, and 244.5±58.9 µm in the CC group.
CONCLUSION
The marginal gap in the LW and NC groups were clinically acceptable. Further improvement is needed for CC group to be used clinical practice.
Keyword
Figure
Reference
-
1. Konstantoulakis E, Nakajima H, Woody RD, Miller AW. Marginal fit and surface roughness of crowns made with an accelerated casting technique. J Prosthet Dent. 1998; 80:337–345.2. Tao J, Yoda M, Kimura K, Okuno O. Fit of metal ceramic crowns cast in Au-1.6 wt% Ti alloy for different abutment finish line curvature. Dent Mater. 2006; 22:397–404.3. Ucar Y, Akova T, Akyil MS, Brantley WA. Internal fit evaluation of crowns prepared using a new dental crown fabrication technique: laser-sintered Co-Cr crowns. J Prosthet Dent. 2009; 102:253–259.4. Duret F, Blouin JL, Duret B. CAD-CAM in dentistry. J Am Dent Assoc. 1988; 117:715–720.5. Miyazaki T, Hotta Y, Kunii J, Kuriyama S, Tamaki Y. A review of dental CAD/CAM: current status and future perspectives from 20 years of experience. Dent Mater J. 2009; 28:44–56.6. Davis DR. Limiting wax pattern distortion caused by setting expansion. J Prosthet Dent. 1987; 58:229–234.7. van Noort R. The future of dental devices is digital. Dent Mater. 2012; 28:3–12.8. Kim CM, Kim SR, Kim JH, Kim HY, Kim WC. Trueness of milled prostheses according to number of ball-end mill burs. J Prosthet Dent. 2016; 115:624–629.9. Örtorp A, Jönsson D, Mouhsen A, Vult von. The fit of cobalt-chromium three-unit fixed dental prostheses fabricated with four different techniques: a comparative in vitro study. Dent Mater. 2011; 27:356–363.10. Huang SH, Liu P, Mokasdar A, Hou L. Additive manufacturing and its societal impact: a literature review. Int J Adv Manuf Technol. 2013; 67:1191–1203.11. Park JY, Kim HY, Kim JH, Kim JH, Kim WC. Comparison of prosthetic models produced by traditional and additive manufacturing methods. J Adv Prosthodont. 2015; 7:294–302.12. Lee IH, Cho DW. Micro-stereolithography photopolymer solidification patterns for various laser beam exposure conditions. Int J Adv Manuf Technol. 2003; 22:410–416.13. Akova T, Ucar Y, Tukay A, Balkaya MC, Brantley WA. Comparison of the bond strength of laser-sintered and cast base metal dental alloys to porcelain. Dent Mater. 2008; 24:1400–1404.14. Kim KB, Kim WC, Kim HY, Kim JH. An evaluation of marginal fit of three-unit fixed dental prostheses fabricated by direct metal laser sintering system. Dent Mater. 2013; 29:e91–e96.15. Furst A, Radding SB. New developments in the study of metal carcinogenesis. J Environ Sci Health Part C. 1984; 2:103–133.16. Lu Y, Chen W, Ke W, Wu S. Nickel-based (Ni-Cr and Ni-Cr-Be) alloys used in dental restorations may be a potential cause for immune-mediated hypersensitivity. Med Hypotheses. 2009; 73:716–717.17. Reclaru L, Unger RE, Kirkpatrick CJ, Susz C, Eschler PY, Zuercher MH, Antoniac I, Lüthy H. Ni-Cr based dental alloys; Ni release, corrosion and biological evaluation. Mater Sci Eng C Mater Biol Appl. 2012; 32:1452–1460.18. Pradíes G, Zarauz C, Valverde A, Ferreiroa A, Martínez-Rus F. Clinical evaluation comparing the fit of all-ceramic crowns obtained from silicone and digital intraoral impressions based on wavefront sampling technology. J Dent. 2015; 43:201–208.19. Aktas G, Özcan N, Aydin DH, Şahin E, Akça K. Effect of digitizing techniques on the fit of implant-retained crowns with different antirotational abutment features. J Prosthet Dent. 2014; 111:367–372.20. Chazine M, Casucci A, Mazzoni A, Grandini S, Goracci C, Breschi L, Ferrari M. Interfacial nanoleakage and internal cement thickness of three esthetic crown systems. Dent Mater. 2012; 28:1105–1111.21. Beuer F, Aggstaller H, Edelhoff D, Gernet W, Sorensen J. Marginal and internal fits of fixed dental prostheses zirconia retainers. Dent Mater. 2009; 25:94–102.22. Karlsson S. The fit of Procera titanium crowns. An in vitro and clinical study. Acta Odontol Scand. 1993; 51:129–134.23. McLean JW, von Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971; 131:107–111.24. Fransson B, Oilo G, Gjeitanger R. The fit of metal-ceramic crowns, a clinical study. Dent Mater. 1985; 1:197–199.25. Syrek A, Reich G, Ranftl D, Klein C, Cerny B, Brodesser J. Clinical evaluation of all-ceramic crowns fabricated from intraoral digital impressions based on the principle of active wavefront sampling. J Dent. 2010; 38:553–559.26. Boening KW, Walter MH, Reppel PD. Non-cast titanium restorations in fixed prosthodontics. J Oral Rehabil. 1992; 19:281–287.27. Jacobs MS, Windeler AS. An investigation of dental luting cement solubility as a function of the marginal gap. J Prosthet Dent. 1991; 65:436–442.28. Kokubo Y, Tsumita M, Kano T, Sakurai S, Fukushima S. Clinical marginal and internal gaps of zirconia all-ceramic crowns. J Prosthodont Res. 2011; 55:40–43.29. Elshahawy W. Marginal accuracy in casting titanium fixed partial dentures. Tanta Dent J. 2015; 12:119–123.30. Singh V, Gupta S, Bhargava A, Kaul S. Marginal accuracy of metal copings produced with different ring casting techniques: An in vitro study. Eur J Prosthodont. 2015; 3:36–41.31. Molin M, Karlsson S. The fit of gold inlays and three ceramic inlay systems. A clinical and in vitro study. Acta Odontol Scand. 1993; 51:201–206.32. Grenade C, Mainjot A, Vanheusden A. Fit of single tooth zirconia copings: comparison between various manufacturing processes. J Prosthet Dent. 2011; 105:249–255.33. de Torres EM, Rodrigues RC, de Mattos Mda G, Ribeiro RF. The effect of commercially pure titanium and alternative dental alloys on the marginal fit of one-piece cast implant frameworks. J Dent. 2007; 35:800–805.34. Hutton JE, Marshall GW. The expansion of phosphate bonded investments: Part I-Setting expansion. J Prosthet Dent. 1993; 70:121–125.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The study of tension characteristics in orthodontic wires
- Evaluation and comparison of the marginal adaptation of two different substructure materials
- Study on the effect of soldering methods on the characteristics of the Ni-Cr alloy
- Influence of the accuracy of abutment tooth preparation on the marginal adaptation of Co-Cr alloy copings fabricated with a selective laser sintering technology
- SHEAR BOND STRENGTH OF RESIN ADHESIVE CEMENT TO ENAMEL AND Ni-Cr-Be ALLOY