J Pathol Transl Med.
2015 Sep;49(5):389-395. 10.4132/jptm.2015.08.10.
Parafibromin Staining Characteristics in Urothelial Carcinomas and Relationship with Prognostic Parameters
- Affiliations
-
- 1Department of Pathology, Sifa University Faculty of Medicine, Izmir, Turkey. serapkaraarslan@gmail.com
- 2Department of Pathology, Ege University Faculty of Medicine, Izmir, Turkey.
- 3Department of Urology, Sifa University Faculty of Medicine, Izmir, Turkey.
- KMID: 2381394
- DOI: http://doi.org/10.4132/jptm.2015.08.10
Abstract
- BACKGROUND
Parafibromin is a recently defined tumor suppressor gene. The aim of our study was to determine the relationships of parafibromin expression in urothelial carcinomas (UCs) with prognostic parameters and to evaluate the use of parafibromin as a potential marker of UC.
METHODS
Parafibromin expression was assessed in 49 UC specimens using immunohistochemistry. The correlations between parafibromin expression and clinical and pathologic parameters were investigated.
RESULTS
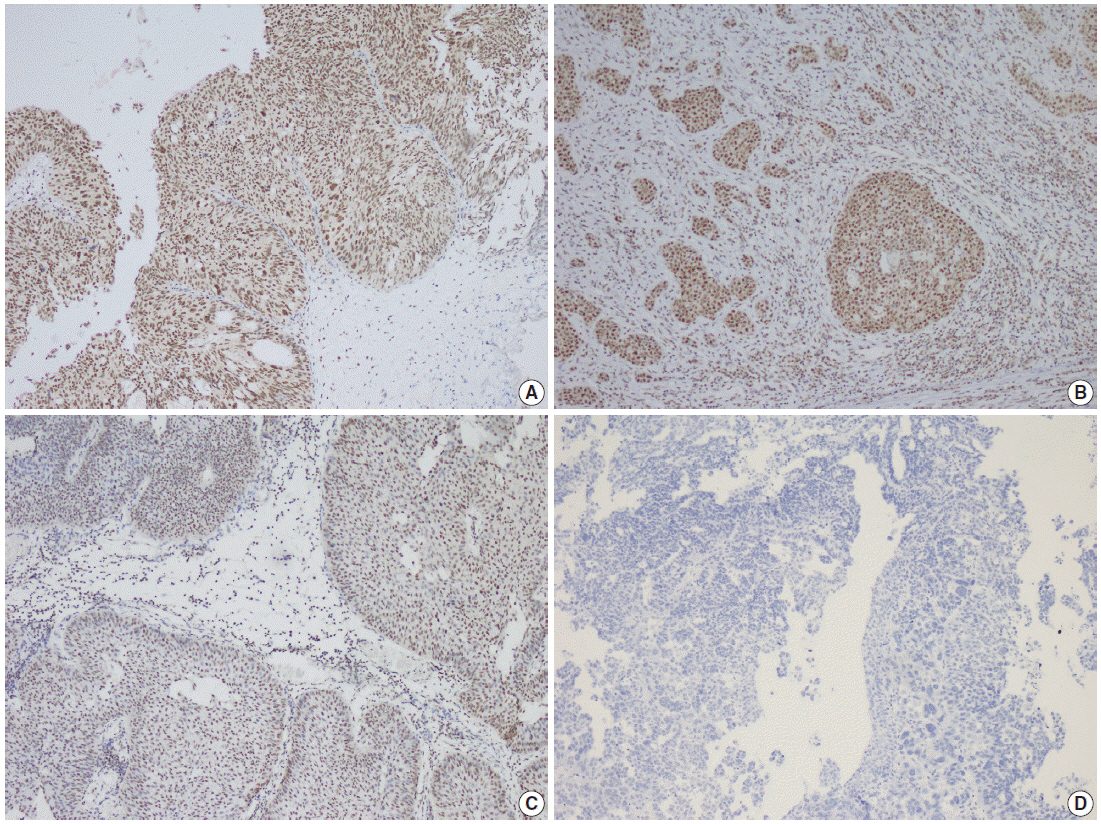
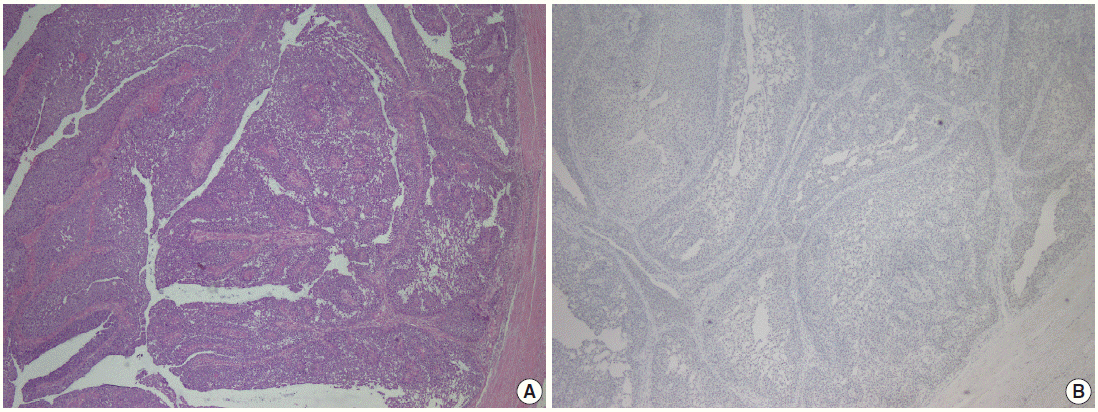
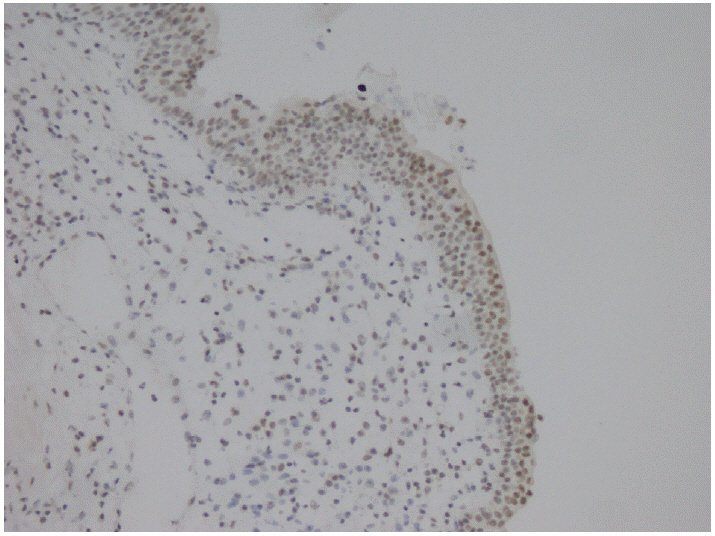
Of the patients, 42 (85.7%) were male, and the mean age was 69.6 +/- 8.2 years (range, 54 to 88 years). Morphologically, the UCs were divided into two groups: papillary (n = 27) and non-papillary (n = 22). There were seven low-grade (14.3%) and 42 high-grade (85.7%) tumors. Parafibromin was negative in 13 tumors (26.5%), partially positive in 19 tumors (38.8%), and positive in 17 tumors (34.7%). Parafibromin expression was more negative in UCs from upper urinary locations (n=17) and with muscularis propria invasion (n=28), which was statistically significant (p = .009 and p = .007, respectively). There was no statistically significant relationship between parafibromin expression and gender, age, tumor grade, survival, or disease-free survival.
CONCLUSIONS
We found that UC cases with parafibromin positivity had less of a tendency to show muscularis propria invasion and were more commonly located in the lower urinary system. These results need to be confirmed with studies based on larger case series.
Figure
Cited by 1 articles
-
Significance of Parafibromin Expression in Laryngeal Squamous Cell Carcinomas
Inju Cho, Mija Lee, Sharon Lim, Ran Hong
J Pathol Transl Med. 2016;50(4):264-269. doi: 10.4132/jptm.2016.04.24.
Reference
-
1. Ploeg M, Aben KK, Kiemeney LA. The present and future burden of urinary bladder cancer in the world. World J Urol. 2009; 27:289–93.
Article2. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009; 59:225–49.
Article3. Margulis V, Shariat SF, Matin SF, et al. Outcomes of radical nephroureterectomy: a series from the Upper Tract Urothelial Carcinoma Collaboration. Cancer. 2009; 115:1224–33.
Article4. Oldbring J, Glifberg I, Mikulowski P, Hellsten S. Carcinoma of the renal pelvis and ureter following bladder carcinoma: frequency, risk factors and clinicopathological findings. J Urol. 1989; 141:1311–3.
Article5. Babjuk M, Oosterlinck W, Sylvester R, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder. Eur Urol. 2008; 54:303–14.
Article6. Hall MC, Womack S, Sagalowsky AI, Carmody T, Erickstad MD, Roehrborn CG. Prognostic factors, recurrence, and survival in transitional cell carcinoma of the upper urinary tract: a 30-year experience in 252 patients. Urology. 1998; 52:594–601.
Article7. Olgac S, Mazumdar M, Dalbagni G, Reuter VE. Urothelial carcinoma of the renal pelvis: a clinicopathologic study of 130 cases. Am J Surg Pathol. 2004; 28:1545–52.8. Faraj SF, Chaux A, Gonzalez-Roibon N, et al. ARID1A immunohistochemistry improves outcome prediction in invasive urothelial carcinoma of urinary bladder. Hum Pathol. 2014; 45:2233–9.
Article9. Ramos Soler D, Ferrer Lozano J, Navarro Fos S, Llombart-Bosch A. Multiple analysis of morphologic factors with prognostic value in transitional cell papillary carcinoma of the bladder. Retrospective study of 571 cases. Actas Urol Esp. 1999; 23:119–26.10. Schapers RF, Pauwels RP, Wijnen JT, et al. A simplified grading method of transitional cell carcinoma of the urinary bladder: reproducibility, clinical significance and comparison with other prognostic parameters. Br J Urol. 1994; 73:625–31.
Article11. Aldred MJ, Talacko AA, Savarirayan R, et al. Dental findings in a family with hyperparathyroidism-jaw tumor syndrome and a novel HRPT2 gene mutation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:212–8.12. Pimenta FJ, Gontijo Silveira LF, Tavares GC, et al. HRPT2 gene alterations in ossifying fibroma of the jaws. Oral Oncol. 2006; 42:735–9.13. Shattuck TM, Välimäki S, Obara T, et al. Somatic and germ-line mutations of the HRPT2 gene in sporadic parathyroid carcinoma. N Engl J Med. 2003; 349:1722–9.14. Carpten JD, Robbins CM, Villablanca A, et al. HRPT2, encoding parafibromin, is mutated in hyperparathyroidism-jaw tumor syndrome. Nat Genet. 2002; 32:676–80.15. Wang PF, Tan MH, Zhang C, Morreau H, Teh BT. HRPT2, a tumor suppressor gene for hyperparathyroidism-jaw tumor syndrome. Horm Metab Res. 2005; 37:380–3.16. Cetani F, Ambrogini E, Viacava P, et al. Should parafibromin staining replace HRTP2 gene analysis as an additional tool for histologic diagnosis of parathyroid carcinoma? Eur J Endocrinol. 2007; 156:547–54.
Article17. Gill AJ, Clarkson A, Gimm O, et al. Loss of nuclear expression of parafibromin distinguishes parathyroid carcinomas and hyperparathyroidism-jaw tumor (HPT-JT) syndrome-related adenomas from sporadic parathyroid adenomas and hyperplasias. Am J Surg Pathol. 2006; 30:1140–9.
Article18. Selvarajan S, Sii LH, Lee A, et al. Parafibromin expression in breast cancer: a novel marker for prognostication? J Clin Pathol. 2008; 61:64–7.
Article19. Tan MH, Morrison C, Wang P, et al. Loss of parafibromin immunoreactivity is a distinguishing feature of parathyroid carcinoma. Clin Cancer Res. 2004; 10:6629–37.
Article20. Zheng HC, Wei ZL, Xu XY, et al. Parafibromin expression is an independent prognostic factor for colorectal carcinomas. Hum Pathol. 2011; 42:1089–102.
Article21. Zheng HC, Takahashi H, Li XH, et al. Downregulated parafibromin expression is a promising marker for pathogenesis, invasion, metastasis and prognosis of gastric carcinomas. Virchows Arch. 2008; 452:147–55.
Article22. Eble JN, Sauter G, Epstein JI, Sesterhenn IA. World Health Organization classification of tumours: pathology and genetics of tumours of the urinary system and male genital organs. Lyon: IARC Press;2004. p. 90.23. Quek ML, Stein JP, Clark PE, et al. Natural history of surgically treated bladder carcinoma with extravesical tumor extension. Cancer. 2003; 98:955–61.
Article24. Tilki D, Reich O, Svatek RS, et al. Characteristics and outcomes of patients with clinical carcinoma in situ only treated with radical cystectomy: an international study of 243 patients. J Urol. 2010; 183:1757–63.
Article25. Kim SH, Yang HK, Lee JH, Lee ES. A retrospective analysis of incidence and its associated risk factors of upper urinary tract recurrence following radical cystectomy for bladder cancer with transitional cell carcinoma: the significance of local pelvic recurrence and positive lymph node. PLoS One. 2014; 9:e96467.
Article26. Rausch S, Hofmann R, von Knobloch R. Nonbilharzial squamous cell carcinoma and transitional cell carcinoma with squamous differentiation of the lower and upper urinary tract. Urol Ann. 2012; 4:14–8.
Article27. Porzionato A, Macchi V, Barzon L, et al. Immunohistochemical assessment of parafibromin in mouse and human tissues. J Anat. 2006; 209:817–27.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Significance of Parafibromin Expression in Laryngeal Squamous Cell Carcinomas
- Expression of p16, Rb and FHIT Proteins in Urothelial Carcinoma of the Urinary Bladder
- Urinary Cytologic Findings of Urothelial Lesions
- Expression of Cyclooxygenase-2 in Urothelial Carcinoma of the Human Urinary Bladder
- A Study on the Relationship between CEA Immunohistochemical Findings and Expression Rate of PCNA and Clinicopathologic Factors of Colorectal Cancers