J Pathol Transl Med.
2015 Jan;49(1):66-70. 10.4132/jptm.2014.10.14.
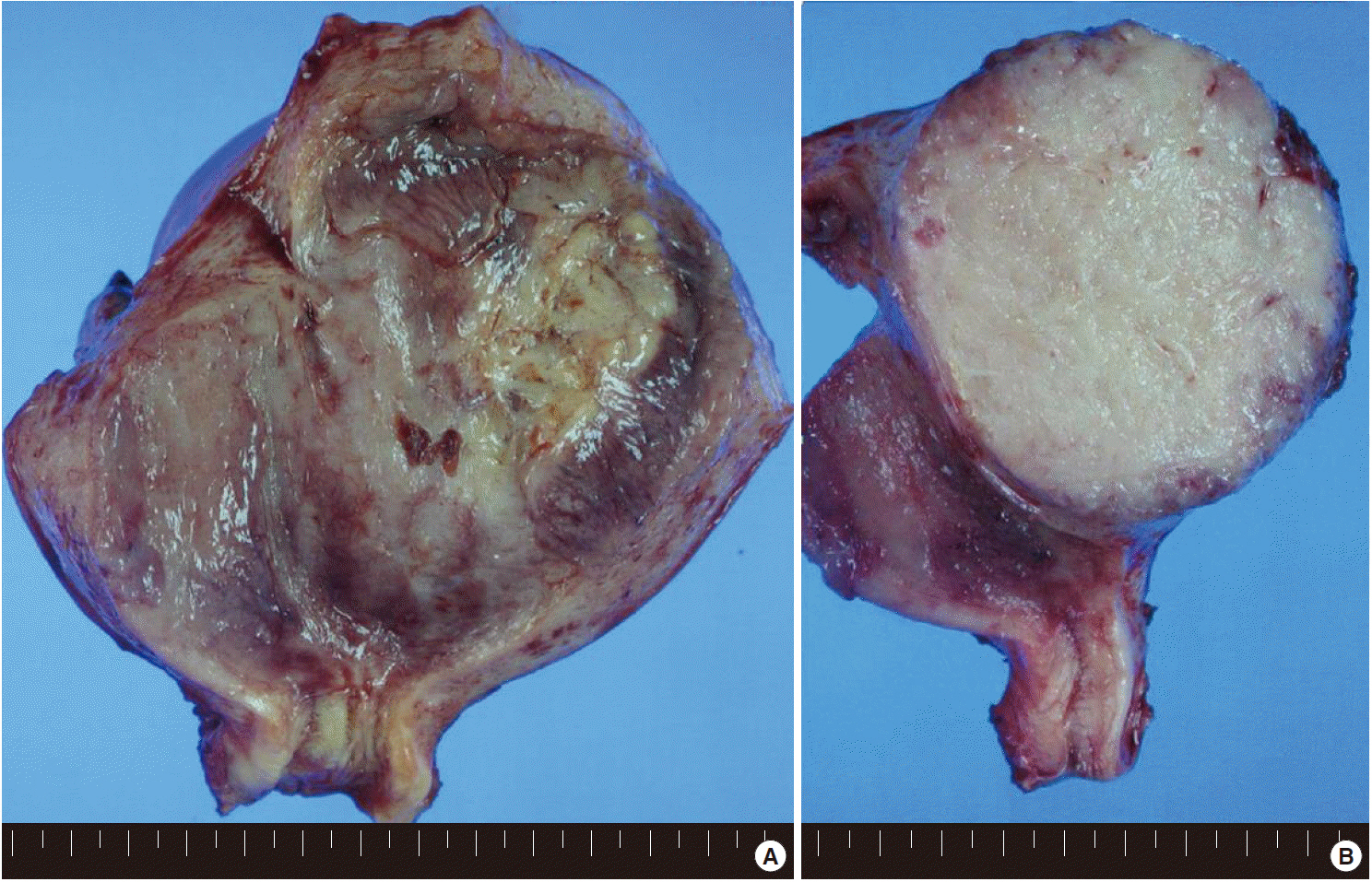
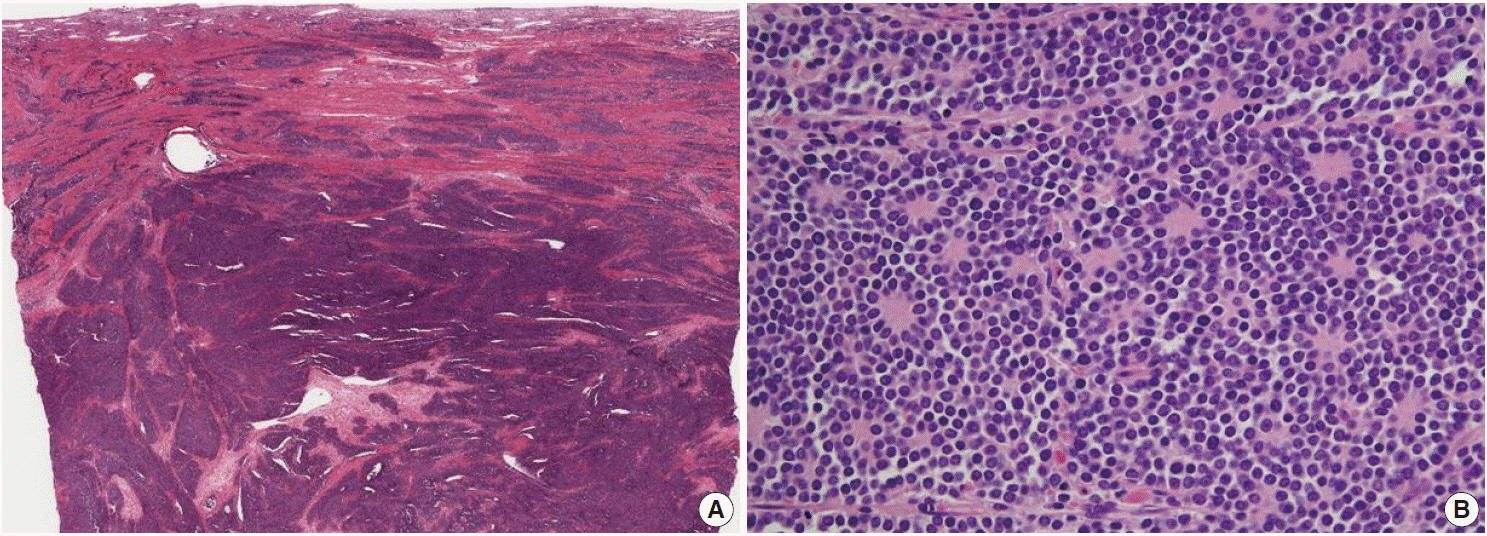
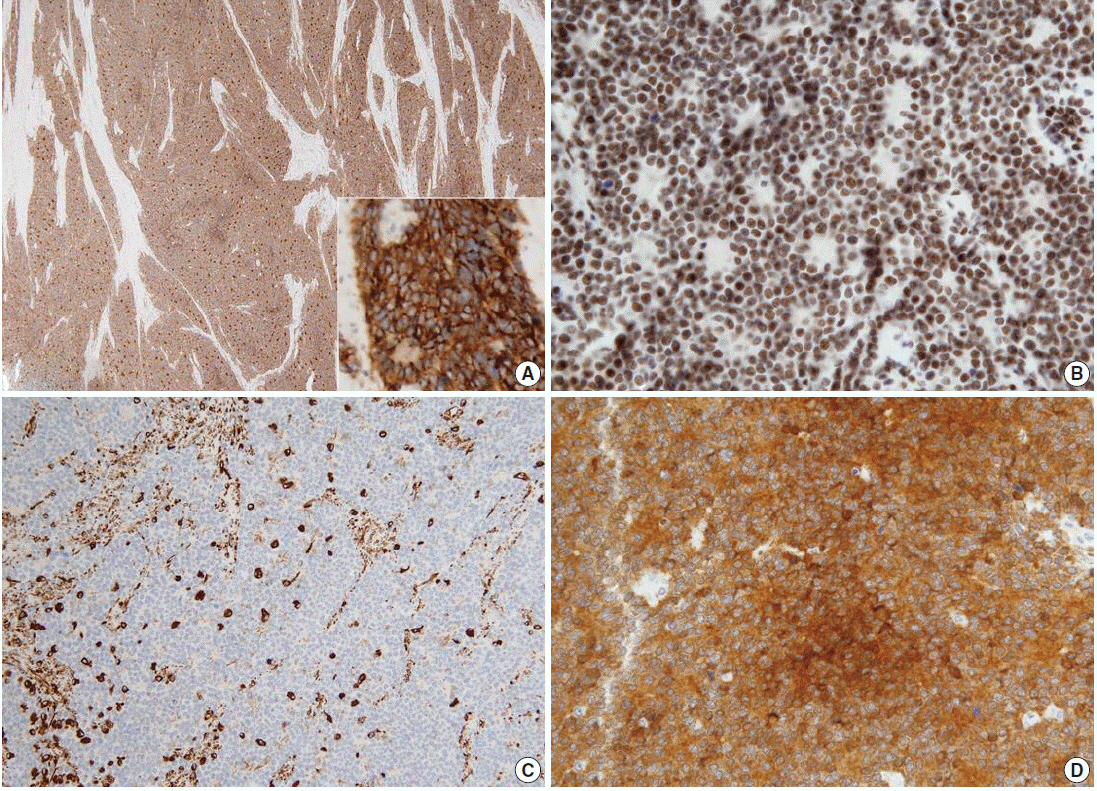
Ewing's Sarcoma/Primitive Neuroectodermal Tumor of the Uterine Corpus
- Affiliations
-
- 1Department of Pathology, Korea University Ansan Hospital, Ansan, Korea. a9604@chollian.net
- 2Department of Pathology, Korea University Anam Hospital, Seoul, Korea.
- KMID: 2381355
- DOI: http://doi.org/10.4132/jptm.2014.10.14
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Hart MN, Earle KM. Primitive neuroectodermal tumors of the brain in children. Cancer. 1973; 32:890–7.
Article2. Masoura S, Kourtis A, Kalogiannidis I, et al. Primary primitive neuroectodermal tumor of the cervix confirmed with molecular analysis in a 23-year-old woman: a case report. Pathol Res Pract. 2012; 208:245–9.
Article3. Truong AH, Ben-David Y. The role of Fli-1 in normal cell function and malignant transformation. Oncogene. 2000; 19:6482–9.
Article4. Kleinman GM, Young RH, Scully RE. Primary neuroectodermal tumors of the ovary: a report of 25 cases. Am J Surg Pathol. 1993; 17:764–78.5. Vang R, Taubenberger JK, Mannion CM, et al. Primary vulvar and vaginal extraosseous Ewing’s sarcoma/peripheral neuroectodermal tumor: diagnostic confirmation with CD99 immunostaining and reverse transcriptase-polymerase chain reaction. Int J Gynecol Pathol. 2000; 19:103–9.
Article6. Liao X, Xin X, Lü X. Primary Ewing’s sarcoma-primitive neuroectodermal tumor of the vagina. Gynecol Oncol. 2004; 92:684–8.
Article7. Tsao AS, Roth LM, Sandler A, Hurteau JA. Cervical primitive neuroectodermal tumor. Gynecol Oncol. 2001; 83:138–42.
Article8. Ren YL, Tang XY, Li T. Ewing sarcoma-primitive neuroectodermal tumor of the uterus: a clinicopathologic, immunohistochemical and ultrastructural study of one case. Arch Gynecol Obstet. 2011; 283:1139–43.
Article9. Mhawech-Fauceglia P, Herrmann F, Penetrante R, et al. Diagnostic utility of FLI-1 monoclonal antibody and dual-colour, break-apart probe fluorescence in situ (FISH) analysis in Ewing’s sarcoma/primitive neuroectodermal tumour (EWS/PNET): a comparative study with CD99 and FLI-1 polyclonal antibodies. Histopathology. 2006; 49:569–75.10. Sandberg AA, Bridge JA. Updates on the cytogenetics and molecular genetics of bone and soft tissue tumors: desmoplastic small roundcell tumors. Cancer Genet Cytogenet. 2002; 138:1–10.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ewing Sarcoma/Peripheral Primitive Neuroectodermal Tumor in an Adolscence, Manifested as Isolated Cervical Mass
- Double Primary Presentation of Liposarcoma and Ewing's Sarcoma: A Case Report
- A Case of a Primitive Neuroectodermal Tumor Detected from a Duodenal Metastasis
- Ewing's Sarcoma of the Lesser Sac Masquerading as a Pancreatic Tumor
- A case of extraosseous ewing's sarcoma/primitive neuroectodermal tumor of the ovary