Investig Clin Urol.
2017 Jun;58(Suppl 1):S46-S53. 10.4111/icu.2017.58.S1.S46.
Aggressive diagnosis and treatment for posterior urethral valve as an etiology for vesicoureteral reflux or urge incontinence in children
- Affiliations
-
- 1Department of Pediatric Urology, Jichi Medical University Children's Medical Center Tochigi, Shimotsuke, Japan. hnakai@jichi.ac.jp
- KMID: 2379895
- DOI: http://doi.org/10.4111/icu.2017.58.S1.S46
Abstract
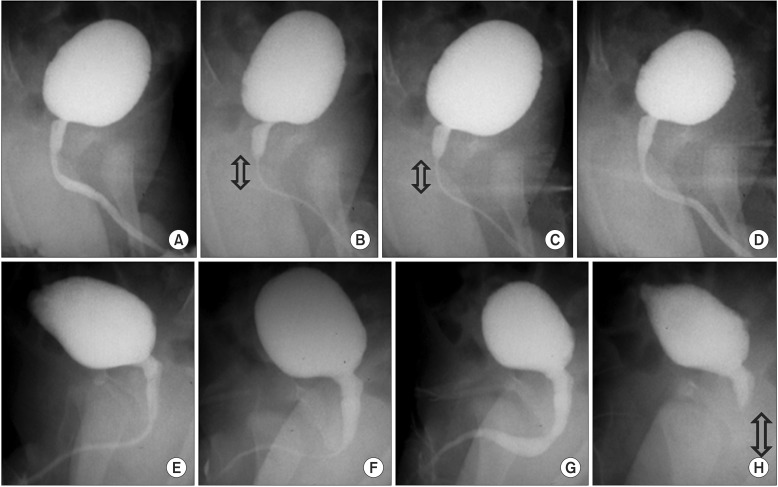
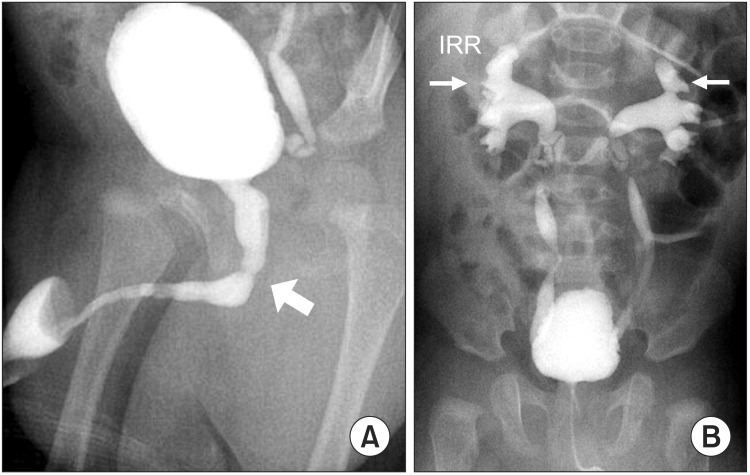
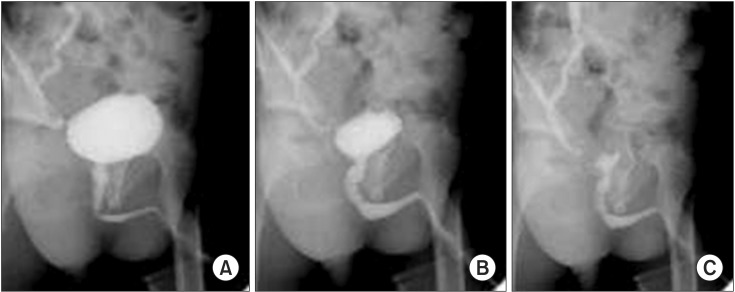
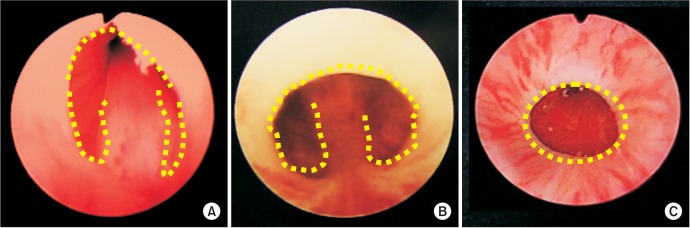
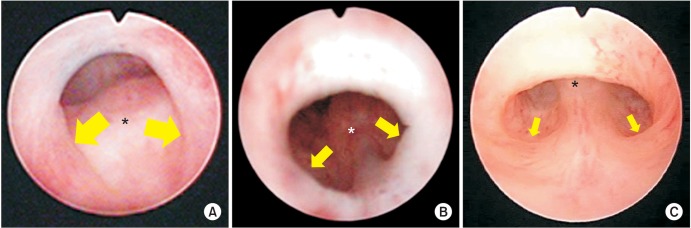
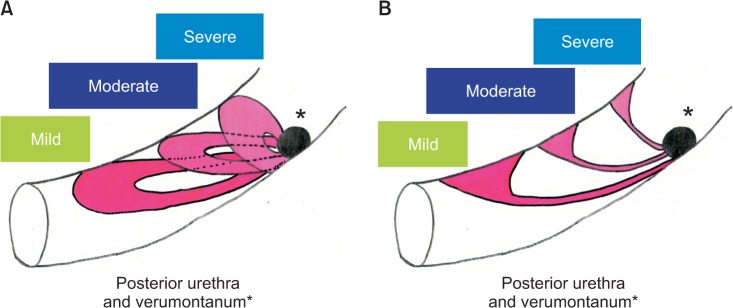
- Vesicoureteral reflux (VUR) is one of the most common diseases in pediatric urology and classified into primary and secondary VUR. Although posterior urethral valve (PUV) is well known as a cause of the secondary VUR, it is controversial that minor urethral deformity recognized in voiding cystourethrography represents mild end of PUV spectrum and contributes to the secondary VUR. We have been studying for these ten years congenital urethral obstructive lesions with special attention to its urethrographic and endoscopic morphology as well as therapeutic response with transurethral incision. Our conclusion to date is that congenital obstructive lesion in the postero-membranous urethra is exclusively PUV (types 1 and 3) and that severity of obstruction depends on broad spectrum of morphological features recognized in PUV. Endoscopic diagnostic criteria for PUV are being consolidated.
MeSH Terms
Figure
Cited by 1 articles
-
Pediatric vesicoureteral reflux: Slow but steady steps
Yong Seung Lee, Sang Won Han
Investig Clin Urol. 2017;58(Suppl 1):S1-S3. doi: 10.4111/icu.2017.58.S1.S1.
Reference
-
1. de Kort LM, Uiterwaal CS, Beek EJ, Jan Nievels RA, Klijn AJ, de Jong TP. Reliability of voiding cystourethrography to detect urethral obstruction in boys. Urology. 2004; 63:967–971. PMID: 15134990.
Article2. de Jong TP, Radmayr C, Dik P, Chrzan R, Klijn AJ, de Kort L, et al. Posterior urethral valves: search for a diagnostic reference standard. Urology. 2008; 72:1022–1025. PMID: 18585762.
Article3. Ichino M, Igawa Y, Seki S, Ishizuka O, Nishizawa O. Natural history and etiology of high pressure voiding in male infants. J Urol. 2007; 178:2561–2565. PMID: 17945306.
Article4. Dewan PA, Zappala SM, Ransley PG, Duffy PG. Endoscopic reappraisal of the morphology of congenital obstruction of the posterior urethra. Br J Urol. 1992; 70:439–444. PMID: 1450856.
Article5. Dewan PA, Keenan RJ, Morris LL, Le Quesne GW. Congenital urethral obstruction: Cobb's collar or prolapsed congenital obstructive posterior urethral membrane (COPUM). Br J Urol. 1994; 73:91–95. PMID: 8298906.
Article6. Farhat W, McLorie G, Capolicchio G, Khoury A, Bägli D, Merguerian PA. Outcomes of primary valve ablation versus urinary tract diversion in patients with posterior urethral valves. Urology. 2000; 56:653–657. PMID: 11018624.
Article7. Nakamura S, Kawai S, Kubo T, Kihara T, Mori K, Nakai H. Transurethral incision of congenital obstructive lesions in the posterior urethra in boys and its effect on urinary incontinence and urodynamic study. BJU Int. 2011; 107:1304–1311. PMID: 20804485.
Article8. Nakamura S, Hyuga T, Kawai S, Kubo T, Nakai H. The endoscopic morphological features of congenital posterior urethral obstructions in boys with refractory daytime urinary incontinence and nocturnal enuresis. Eur J Pediatr Surg. 2016; 26:368–375. PMID: 26378483.
Article9. Hyuga T, Nakamura S, Kawai S, Kubo T, Furukawa R, Aihara T, et al. The changes of urethral morphology recognized in voiding cystourethrography after endoscopic transurethral incision for posterior urethral valve in boys with intractable daytime urinary incontinence and nocturnal enuresis. World J Urol. 2017; 2. 28. [Epub]. DOI: 10.1007/s00345-017-2018-4.
Article