Korean Circ J.
2017 Mar;47(2):254-262. 10.4070/kcj.2016.0226.
Short-Term Change of Exercise Capacity in Patients with Pulmonary Valve Replacement after Tetralogy of Fallot Repair
- Affiliations
-
- 1Department of Pediatrics, Sejong General Hospital, Bucheon, Korea. prelud15@korea.com
- KMID: 2377467
- DOI: http://doi.org/10.4070/kcj.2016.0226
Abstract
- BACKGROUND AND OBJECTIVES
The aim of this study was to investigate the effect of pulmonary valve replacement (PVR) on exercise capacity and determine cardiopulmonary exercise (CPEX) parameters associated with improvement in right ventricle (RV) function.
SUBJECTS AND METHODS
We retrospectively analyzed CPEX and magnetic resonance imaging parameters in a total of 245 patients who underwent PVR from January 1998 to October 2015. In addition, we analyzed the characteristics of the patients who showed improved exercise capacity after PVR.
RESULTS
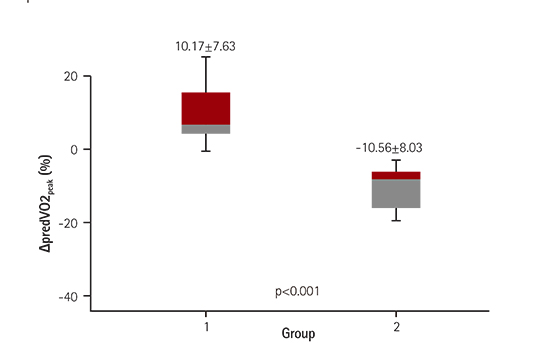
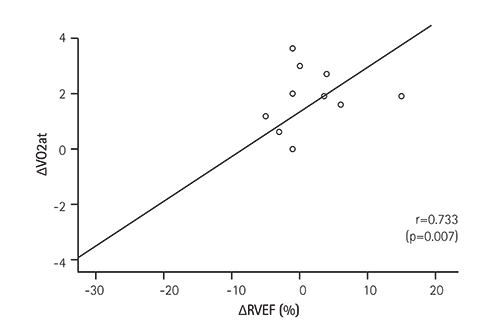
Twenty-eight patients met the inclusion criteria for the study. CPEX parameters after PVR showed no significant changes in all patients. However, baseline predicted peak oxygen uptake (VO2(peak)) (%) value was significantly lower in patients with significant improvement in exercise capacity after PVR, as compared to patients who showed decreased exercise capacity after PVR (60.83±10.28 vs. 75.81±13.83) (p=0.003). In addition, patients with improved exercise capacity showed a positive correlation between the change of right ventricular ejection fraction (RVEF) (%) and the change of anaerobic threshold (r=0.733, p=0.007); whereas, patients with decreased exercise capacity showed a negative correlation between the change of RVEF (%) and the change of predicted VO2(peak) (%) (r=−0.575, p=0.020).
CONCLUSION
The importance of predicted VO2(peak) (%) in evaluating exercise capacity differentiated from other CPEX variables. The change of anaerobic threshold and predicted VO2(peak) (%) might be a useful predictor of the change in RV function after PVR.
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of Predicted Exercise Capacity Equations in Adult Korean Subjects
Daehyun Jeong, Yeon-Mok Oh, Sei Won Lee, Sang-Do Lee, Jae Seung Lee
J Korean Med Sci. 2022;37(14):e113. doi: 10.3346/jkms.2022.37.e113.
Reference
-
1. Bove EL, Byrum CJ, Thomas FD, et al. The influence of pulmonary insufficiency on ventricular function following repair of tetralogy of Fallot. Evaluation using radionuclide ventriculography. J Thorac Cardiovasc Surg. 1983; 85:691–696.2. Katz NM, Blackstone EH, Kirklin JW, Pacifico AD, Bargeron LM Jr. Late survival and symptoms after repair of tetralogy of Fallot. Circulation. 1982; 65:403–410.3. Murphy JG, Gersh BJ, Mair DD, et al. Long-term outcome in patients undergoing surgical repair of tetralogy of Fallot. N Engl J Med. 1993; 329:593–599.4. Nollert G, Fischlein T, Bouterwek S, Bohmer C, Klinner W, Reichart B. Long-term survival in patients with repair of tetralogy of Fallot: 36-year follow-up of 490 survivors of the first year after surgical repair. J Am Coll Cardiol. 1997; 30:1374–1383.5. Ilbawi MN, Idriss FS, DeLeon SY, et al. Factors that exaggerate the deleterious effects of pulmonary insufficiency on the right ventricle after tetralogy repair. Surgical implications. J Thorac Cardiovasc Surg. 1987; 93:36–44.6. Bouzas B, Kilner PJ, Gatzoulis MA. Pulmonary regurgitation: not a benign lesion. Eur Heart J. 2005; 26:433–439.7. Gatzoulis MA, Balaji S, Webber SA, et al. Risk factors for arrhythmia and sudden cardiac death late after repair of tetralogy of Fallot: a multicentre study. Lancet. 2000; 356:975–981.8. Geva T, Sandweiss BM, Gauvreau K, Lock JE, Powell AJ. Factors associated with impaired clinical status in long-term survivors of tetralogy of Fallot repair evaluated by magnetic resonance imaging. J Am Coll Cardiol. 2004; 43:1068–1074.9. Therrien J, Marx GR, Gatzoulis MA. Late problems in tetralogy of Fallot-recognition, management, and prevention. Cardiol Clin. 2002; 20:395–404.10. Babu-Narayan SV, Diller GP, Gheta RR, et al. Clinical outcomes of surgical pulmonary valve replacement after repair of tetralogy of Fallot and potential prognostic value of preoperative cardiopulmonary exercise testing. Circulation. 2014; 129:18–27.11. Lee C, Kim YM, Lee CH, et al. Outcomes of pulmonary valve replacement in 170 patients with chronic pulmonary regurgitation after relief of right ventricular outflow tract obstruction: implications for optimal timing of pulmonary valve replacement. J Am Coll Cardiol. 2012; 60:1005–1014.12. Frigiola A, Tsang V, Bull C, et al. Biventricular response after pulmonary valve replacement for right ventricular outflow tract dysfunction: is age a predictor of outcome? Circulation. 2008; 118:14 Suppl. S182–S190.13. Lee JS, Jang SI, Kim SH, Lee SY, Baek JS, Shim WS. The results of cardiopulmonary exercise test in healthy Korean children and adolescents: single center study. Korean J Pediatr. 2013; 56:242–246.14. Guazzi M, Adams V, Conraads V, et al. EACPR/AHA Scientific Statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2012; 126:2261–2274.15. Matsumura N, Nishijima H, Kojima S, Hashimoto F, Minami M, Yasuda H. Determination of anaerobic threshold for assessment of functional state in patients with chronic heart failure. Circulation. 1983; 68:360–367.16. Buechel ER, Dave HH, Kellenberger CJ, et al. Remodelling of the right ventricle after early pulmonary valve replacement in children with repaired tetralogy of Fallot: assessment by cardiovascular magnetic resonance. Eur Heart J. 2005; 26:2721–2727.17. Oechslin EN, Harrison DA, Harris L, et al. Reoperation in adults with repair of tetralogy of fallot: indications and outcomes. J Thorac Cardiovasc Surg. 1999; 118:245–251.18. Lurz P, Giardini A, Taylor AM, et al. Effect of altering pathologic right ventricular loading conditions by percutaneous pulmonary valve implantation on exercise capacity. Am J Cardiol. 2010; 105:721–726.19. Batra AS, McElhinney DB, Wang W, et al. Cardiopulmonary exercise function among patients undergoing transcatheter pulmonary valve implantation in the US Melody valve investigational trial. Am Heart J. 2012; 163:280–287.20. Gengsakul A, Harris L, Bradley TJ, et al. The impact of pulmonary valve replacement after tetralogy of Fallot repair: a matched comparison. Eur J Cardiothorac Surg. 2007; 32:462–468.21. Ghez O, Tsang VT, Frigiola A, et al. Right ventricular outflow tract reconstruction for pulmonary regurgitation after repair of tetralogy of Fallot. Preliminary results. Eur J Cardiothorac Surg. 2007; 31:654–658.22. Sterrett LE, Ebenroth ES, Query C, et al. Why exercise capacity does not improve after pulmonary valve replacement. Pediatr Cardiol. 2014; 35:1395–1402.23. Oosterhof T, Mulder BJ, Vliegen HW, de Roos A. Cardiovascular magnetic resonance in the follow-up of patients with corrected tetralogy of Fallot: a review. Am Heart J. 2006; 151:265–272.24. Fredriksen PM, Therrien J, Veldtman G, et al. Aerobic capacity in adults with tetralogy of Fallot. Cardiol Young. 2002; 12:554–559.25. Wasserman K, Hansen JE, Sue DY, Whipp BJ. Principles of exercise testing and interpretation. 2nd ed. Malvern, Philadelphia: Lea & Febiger;1994. p. 64.26. LW S. Role of exercise testing in the evaluation of candidates for cardiac transplantation. In : Wasserman K, editor. Exercise gas exchange in heart disease. New York: Futura Publishing Company;1996. p. 271–286.27. Ivy JL, Withers RT, Van Handel PJ, Elger DH, Costill DL. Muscle respiratory capacity and fiber type as determinants of the lactate threshold. J Appl Physiol Respir Environ Exerc Physiol. 1980; 48:523–527.28. Sullivan MJ, Higginbotham MB, Cobb FR. Exercise training in patients with chronic heart failure delays ventilatory anaerobic threshold and improves submaximal exercise performance. Circulation. 1989; 79:324–329.29. Davis JA. Anaerobic threshold: review of the concept and directions for future research. Med Sci Sports Exerc. 1985; 17:6–21.30. Gaultier C, Boule M, Thibert M, Leca F. Resting lung function in children after repair of tetralogy of Fallot. Chest. 1986; 89:561–567.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary Valve Replacement after Repair of Tetralogy of Fallot
- Pulmonary Insufficiency after Repair of Tetralogy of Fallot: Prevention and Indications of Pulmonary Valve Replacement
- Tetralogy of Fallot: A Surgical Perspective
- Aortic Root and Ascending Aortic Aneurysm in an Adult with a Repaired Tetralogy of Fallot
- A Case of Severe Pulmonary Regurgitation Due to the Absence of Pulmonary Valve