J Dent Rehabil Appl Sci.
2017 Mar;33(1):7-18. 10.14368/jdras.2017.33.1.7.
Effects of host modulation by nonsteroidal anti-inflammatory drugs on periodontal disease: a systematic review and meta-analysis
- Affiliations
-
- 1Department of Periodontology, College of Dentistry, Dankook University, Cheonan, Republic of Korea. jcp@dent.dku.edu
- 2Institute for Evidence-based Medicine, Department of Preventive Medicine, College of Medicine, Korea University, Seoul, Republic of Korea. jcp@dent.dku.edu
- KMID: 2377054
- DOI: http://doi.org/10.14368/jdras.2017.33.1.7
Abstract
- PURPOSE
Nonsteroidal anti-inflammatory drugs that prohibit biosynthesis of arachidonic acid metabolites have been considered potent host modulation agents. The aim of this review was to determine the effect of nonsteroidal anti-inflammatory drugs adjunctive with nonsurgical periodontal treatment in patients with periodontal disease.
MATERIALS AND METHODS
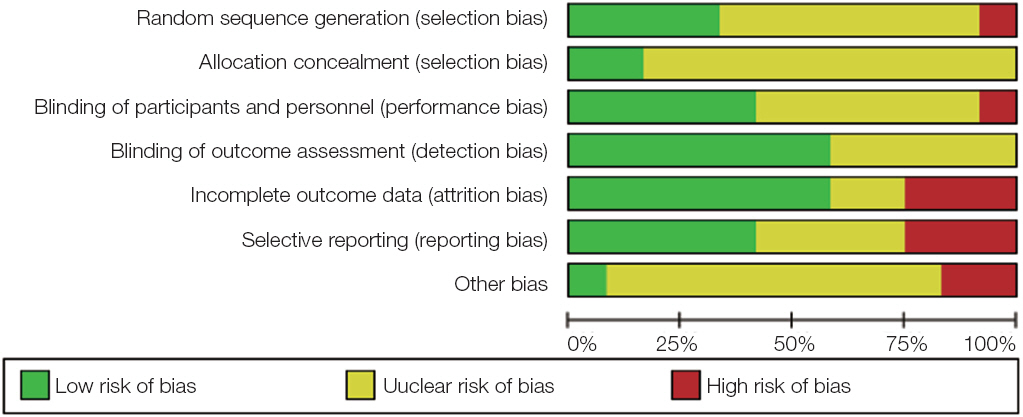
Three electronic databases were searched to identify relevant studies. The methodological quality and mean differences of the change in clinical attachment level and probing depth were analyzed according to Cochrane review methods.
RESULTS
Twelve studies were included in the methodological assessment and nine studies were suitable for inclusion in the meta-analysis. The mean difference in the clinical attachment level gain did not differ significantly between the nonsteroidal anti-inflammatory drugs and control groups at any observation time. The highest mean difference in clinical attachment level gain was 0.30 mm at 4 weeks (95% confidence interval = -0.37 to 0.97). There was a significant mean difference in the probing depth reduction, of 0.34 mm (95% confidence interval = 0.29 to 0.40) at 6 weeks.
CONCLUSION
Therefore, nonsteroidal anti-inflammatory drugs have additional therapeutic effect when administrated with nonsurgical periodontal treatment.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Consensus report. Periodontal diseases: pathogenesis and microbial factors. Ann Periodontol. 1996; 1:926–32. DOI: 10.1902/annals.1996.1.1.926. PMID: 9118284.2. Havemose-Poulsen A, Sørensen LK, Bendtzen K, Holmstrup P. Polymorphisms within the IL-1 gene cluster: effects on cytokine profiles in peripheral blood and whole blood cell cultures of patients with aggressive periodontitis, juvenile idiopathic arthritis, and rheumatoid arthritis. J Periodontol. 2007; 78:475–92. DOI: 10.1902/jop.2007.060135. PMID: 17335371.3. Löe H. Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care. 1993; 16:329–34. DOI: 10.2337/diacare.16.1.329.4. Tomar SL, Asma S. Smoking-attributable periodontitis in the United States: findings from NHANES III. National Health and Nutrition Examination Survey. J Periodontol. 2000; 71:743–51. DOI: 10.1902/jop.2000.71.5.743. PMID: 10872955.5. Cobb CM. Clinical significance of non-surgical periodontal therapy: an evidence-based perspective of scaling and root planing. J Clin Periodontol. 2002; 29(Suppl2):6–16. DOI: 10.1034/j.1600-051X.29.s2.4.x. PMID: 12010523.6. Haffajee AD, Socransky SS, Ebersole JL. Survival analysis of periodontal sites before and after peri-odontal therapy. J Clin Periodontol. 1985; 12:553–67. DOI: 10.1111/j.1600-051X.1985.tb01389.x. PMID: 3860518.7. Giannobile WV, Braun TM, Caplis AK, DoucetteStamm L, Duff GW, Kornman KS. Patient stratification for preventive care in dentistry. J Dent Res. 2013; 92:694–701. DOI: 10.1177/0022034513492336. PMID: 23752171. PMCID: PMC3711568.8. Kornman KS, Page RC, Tonetti MS. The host response to the microbial challenge in periodontitis: assembling the players. Periodontol 2000. 1997; 14:33–53. DOI: 10.1111/j.1600-0757.1997.tb00191.x. PMID: 9567965.9. Page RC. The role of inflammatory mediators in the pathogenesis of periodontal disease. J Periodontal Res. 1991; 26((3 Pt 2)):230–42. DOI: 10.1111/j.1600-0765.1991.tb01649.x. PMID: 1679130.10. Lane N, Armitage GC, Loomer P, Hsieh S, Majumdar S, Wang HY, Jeffcoat M, Munoz T. Bisphosphonate therapy improves the outcome of conventional periodontal treatment: results of a 12-month, randomized, placebo-controlled study. J Periodontol. 2005; 76:1113–22. DOI: 10.1902/jop.2005.76.7.1113. PMID: 16018754.11. Leitão RF, Ribeiro RA, Chaves HV, Rocha FA, Lima V, Brito GA. Nitric oxide synthase inhibition prevents alveolar bone resorption in experimental periodontitis in rats. J Periodontol. 2005; 76:956–63. DOI: 10.1902/jop.2005.76.6.956. PMID: 15948691.12. Martinez GL, Koury JC, Martins MA, Nogueira F, Fischer RG, Gustafsson A, Figueredo CM. Serum level changes of long chain-polyunsaturated fatty acids in patients undergoing periodontal therapy combined with one year of omega-3 supplementation: a pilot randomized clinical trial. J Periodontal Implant Sci. 2014; 44:169–77. DOI: 10.5051/jpis.2014.44.4.169. PMID: 25177518. PMCID: PMC4148629.13. Martuscelli G, Fiorellini JP, Crohin CC, Howell TH. The effect of interleukin-11 on the progression of ligature-induced periodontal disease in the beagle dog. J Periodontol. 2000; 71:573–8. DOI: 10.1902/jop.2000.71.4.573. PMID: 10807121.14. Offenbacher S, Odle BM, Van Dyke TE. The use of crevicular fluid prostaglandin E2 levels as a predictor of periodontal attachment loss. J Periodontal Res. 1986; 21:101–12. DOI: 10.1111/j.1600-0765.1986.tb01443.x. PMID: 2937899.15. Caton JG, Ciancio SG, Blieden TM, Bradshaw M, Crout RJ, Hefti AF, Massaro JM, Polson AM, Thomas J, Walker C. Treatment with subantimicrobial dose doxycycline improves the efficacy of scaling and root planing in patients with adult periodontitis. J Periodontol. 2000; 71:521–32. DOI: 10.1902/jop.2000.71.4.521. PMID: 10807113.16. Preshaw PM, Hefti AF, Novak MJ, Michalowicz BS, Pihlstrom BL, Schoor R, Trummel CL, Dean J, Van Dyke TE, Walker CB, Bradshaw MH. Subantimicrobial dose doxycycline enhances the efficacy of scaling and root planing in chronic periodontitis: a multicenter trial. J Periodontol. 2004; 75:1068–76. DOI: 10.1902/jop.2004.75.8.1068. PMID: 15455733.17. Reddy MS, Geurs NC, Gunsolley JC. Periodontal host modulation with antiproteinase, anti-inflammatory, and bone-sparing agents. A systematic review. Ann Periodontol. 2003; 8:12–37. DOI: 10.1902/annals.2003.8.1.12. PMID: 14971246.18. Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. 5:Wiley Online Library;2008. DOI: 10.1002/9780470712184.19. Opengrey. System for information on grey literature in Europe. Vandoeuvre-lès-Nancy: Institut de l’Information Scientifique et Technique. 2011. Available from: http://www.opengrey.eu/. (updated 2015 Mar 11).20. Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999; 4:1–6. DOI: 10.1902/annals.1999.4.1.1. PMID: 10863370.21. Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull. 1968; 70:213–20. DOI: 10.1037/h0026256. PMID: 19673146.22. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group. Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928. DOI: 10.1136/bmj.d5928. PMID: 22008217. PMCID: PMC3196245.23. Clinicaltrials.gov. A service of the U.S. National Institutes of Health. Bethesda: U.S. National Library of Medicine;2000. Available from: https://clinicaltrials.gov/. (updated 2015 Apr 5).24. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–60. DOI: 10.1136/bmj.327.7414.557. PMID: 12958120. PMCID: PMC192859.25. Aras H, Calayan F, Güncü GN, Berberolu A, Kilinç K. Effect of systemically administered naproxen sodium on clinical parameters and myeloperoxidase and elastase-like activity levels in gingival crevicular fluid. J Periodontol. 2007; 78:868–73. DOI: 10.1902/jop.2007.060412. PMID: 17470020.26. Azoubel MC, Sarmento VA, Cangussú V, Azoubel E, Bittencourt S, Cunha FQ, Ribeiro RA, Brito GA. Adjunctive benefits of systemic etoricoxib in non-surgical treatment of aggressive periodontitis: short-term evaluation. J Periodontol. 2008; 79:1719–25. DOI: 10.1902/jop.2008.080019. PMID: 18771374.27. Buduneli N, Buduneli E, Cetin EO, Kirilmaz L, Kütükçüler N. Clinical findings and gingival crevicular fluid prostaglandin E2 and interleukin-1-beta levels following initial periodontal treatment and short-term meloxicam administration. Expert Opin Pharmacother. 2010; 11:1805–12. DOI: 10.1517/14656566.2010.490555. PMID: 20518615.28. Jeffcoat MK, Page R, Reddy M, Wannawisute A, Waite P, Palcanis K, Cogen R, Williams RC, Basch C. Use of digital radiography to demonstrate the potential of naproxen as an adjunct in the treatment of rapidly progressive periodontitis. J Periodontal Res. 1991; 26:415–21. DOI: 10.1111/j.1600-0765.1991.tb01731.x. PMID: 1832454.29. Ng VW, Bissada NF. Clinical evaluation of systemic doxycycline and ibuprofen administration as an adjunctive treatment for adult periodontitis. J Periodontol. 1998; 69:772–6. DOI: 10.1902/jop.1998.69.7.772. PMID: 9706854.30. Ozgören O, Develioglu H, Güncü G, Akman A, Berker E. The adjunctive effect of tenoxicam during non-surgical periodontal treatment on clinical parameters and gingival crevicular fluid levels of MMP-8 and TNF-alpha in patients with chronic periodontitis - randomized, double-blind clinical trial. Adv Clin Exp Med. 2014; 23:559–65. DOI: 10.17219/acem/37223. PMID: 25166440.31. Reddy MS, Palcanis KG, Barnett ML, Haigh S, Charles CH, Jeffcoat MK. Efficacy of meclofenamate sodium (Meclomen) in the treatment of rapidly progressive periodontitis. J Clin Periodontol. 1993; 20:635–40. DOI: 10.1111/j.1600-051X.1993.tb00708.x. PMID: 8227450.32. Taiyeb Ali TB, Waite IM. The effect of systemic ibuprofen on gingival inflammation in humans. J Clin Periodontol. 1993; 20:723–8. DOI: 10.1111/j.1600-051X.1993.tb00697.x.33. Vardar S, Baylas H, Huseyinov A. Effects of selective cyclooxygenase-2 inhibition on gingival tissue levels of prostaglandin E2 and prostaglandin F2alpha and clinical parameters of chronic periodontitis. J Periodontol. 2003; 74:57–63. DOI: 10.1902/jop.2003.74.1.57. PMID: 12593597.34. Knowles JW, Burgett FG, Nissle RR, Shick RA, Morrison EC, Ramfjord SP. Results of periodontal treatment related to pocket depth and attachment level. Eight years. J Periodontol. 1979; 50:225–33. DOI: 10.1902/jop.1979.50.5.225. PMID: 287778.35. Rostom A, Dube C, Wells G, Tugwell P, Welch V, Jolicoeur E, McGowan J. Prevention of NSAIDinduced gastroduodenal ulcers. Cochrane Database Syst Rev. 2002; 4:CD002296.36. Slomiany BL, Slomiany A. Nonsteroidal antiinflammatory drugs impair oral mucosal repair by eliciting disturbances in endothelin-converting enzyme-1 and constitutive nitric oxide synthase. J Physiol Pharmacol. 2001; 52:81–92. PMID: 11321515.37. Kotsakis GA, Thai A, Ioannou AL, Demmer RT, Michalowicz BS. Association between low-dose aspirin and periodontal disease: results from the continuous national health and nutrition examination survey (NHANES) 2011-2012. J Clin Periodontol. 2015; 42:333–41. DOI: 10.1111/jcpe.12380. PMID: 25683058.38. Salvi GE, Lang NP. Host response modulation in the management of periodontal diseases. J Clin Periodontol. 2005; 32(Suppl6):108–29. DOI: 10.1111/j.1600-051X.2005.00785.x. PMID: 16128833.39. Salvi GE, Lang NP. The effects of non-steroidal anti-inflammatory drugs (selective and non-selective) on the treatment of periodontal diseases. Curr Pharm Des. 2005; 11:1757–69. DOI: 10.2174/1381612053764878.40. Thomson WM, Williams SM. Partial- or full-mouth approaches to assessing the prevalence of and risk factors for periodontal disease in young adults. J Periodontol. 2002; 73:1010–4. DOI: 10.1902/jop.2002.73.9.1010. PMID: 12296585.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Potential Strategies in the Prevention of Nonsteroidal Anti-inflammatory Drugs-Associated Adverse Effects in the Lower Gastrointestinal Tract
- Comparison of different nonsteroidal anti-inflammatory drugs for cesarean section: a systematic review and network meta-analysis
- Efficacy of probiotics for managing infantile colic due to their anti-inflammatory properties: a meta-analysis and systematic review
- Relationship between Periodontal Disease and Chronic Kidney Disease: A Systematic Review of Cohort Studies
- Medical treatment of rheumatoid arthritis (I): Nonsteroidal anti-inflammatory drugs, disease modifying antirheumatic drugs and glucocorticoids