Tuberc Respir Dis.
2017 Apr;80(2):169-178. 10.4046/trd.2017.80.2.169.
The Need for a Well-Organized, Video-Assisted Asthma Education Program at Korean Primary Care Clinics
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Kyung Hee University College of Medicine, Seoul, Korea.
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Konkuk University Medical Center, Seoul, Korea. khyou@kuh.ac.kr
- 3Department of Clinical Pharmacology, Konkuk University Medical Center, Seoul, Korea.
- 4Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea.
- 5Department of Internal Medicine, Hallym University Medical Center, Hallym University College of Medicine, Seoul, Korea.
- 6Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 7Department of Internal Medicine, Hanyang University Guri Hospital, Guri, Korea.
- 8Division of Pulmonology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 9Department of Internal Medicine, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 10Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea.
- 11Department of Internal Medicine, Inje University Seoul Paik Hospital, Seoul, Korea.
- 12Department of Internal Medicine, Ewha Womans University School of Medicine, Seoul, Korea.
- 13Division of Pulmonary Medicine, Department of Internal Medicine, Chung-Ang University School of Medicine, Seoul, Korea.
- 14Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 15Department of Internal Medicine, Research Institute of Clinical Medicine, Chonbuk National University Medical School, Jeonju, Korea.
- 16Department of Internal Medicine, Chonnam National University Hospital, Gwangju, Korea.
- 17Division of Pulmonology, Department of Internal Medicine, Chungnam National University College of Medicine, Daejeon, Korea.
- 18Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 19Department of Internal Medicine and Environmental Health Center, Kangwon National University Hospital, Chuncheon, Korea.
- 20Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea.
- 21Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea.
- 22Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea.
- 23Division of Pulmonology, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 24Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 25Department of Internal Medicine, Ajou University School of Medicine, Suwon, Korea.
- 26Regional Center for Respiratory Disease, Yeungnam University Medical Center, Yeungnam University College of Medicine, Daegu, Korea.
- 27Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea.
- KMID: 2375986
- DOI: http://doi.org/10.4046/trd.2017.80.2.169
Abstract
- BACKGROUND
The purpose of this study was to assess the effect of our new video-assisted asthma education program on patients' knowledge regarding asthma and asthma control.
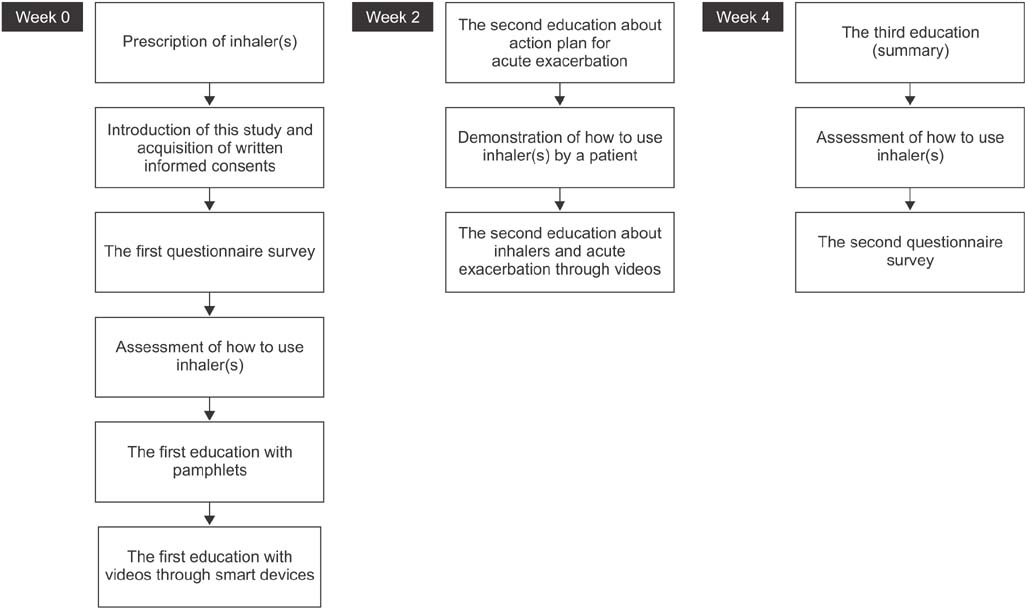
METHODS
Adult asthmatics who were diagnosed by primary care physicians and followed for at least 1 year were educated via smart devices and pamphlets. The education sessions were carried out three times at 2-week intervals. Each education period lasted at most 5 minutes. The effectiveness was then evaluated using questionnaires and an asthma control test (ACT).
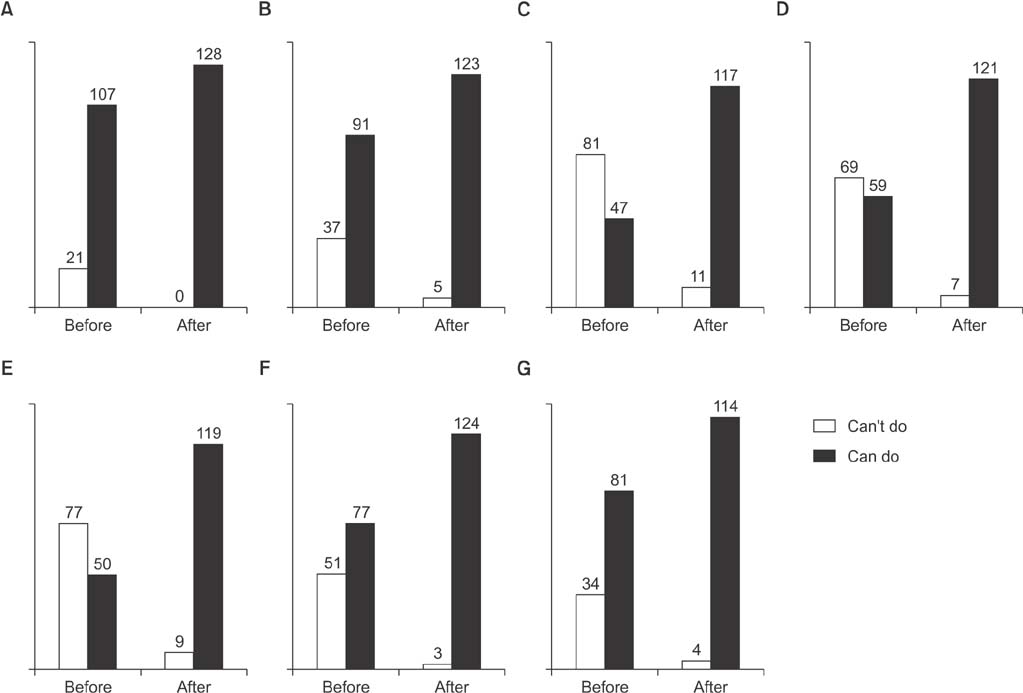
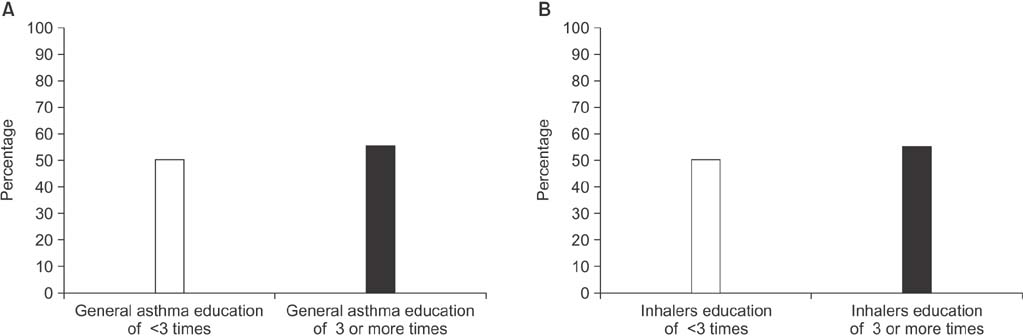
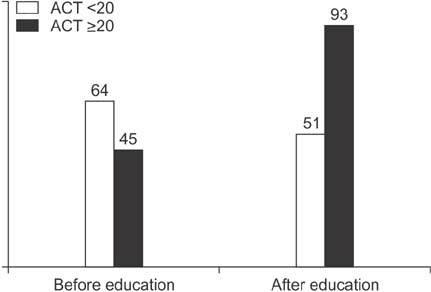
RESULTS
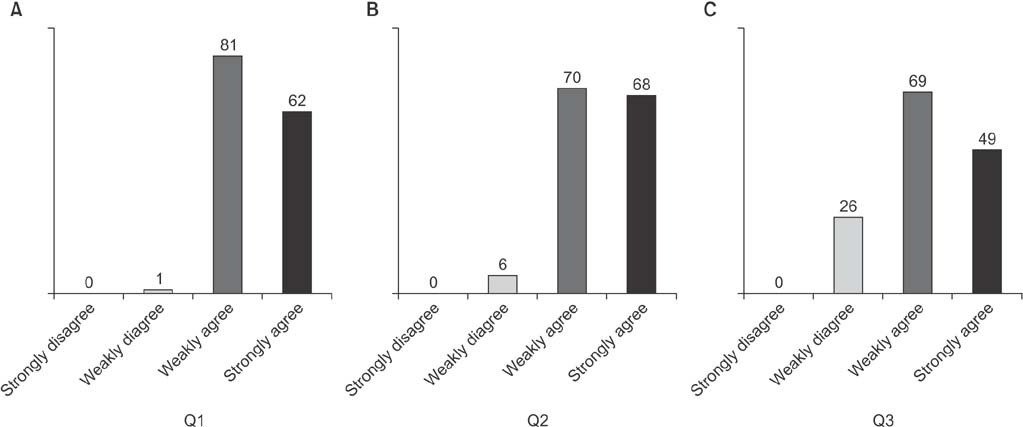
The study enrolled 144 patients (mean age, 56.7±16.7 years). Half of the patients had not been taught how to use their inhalers. After participating in the education program, the participants' understanding of asthma improved significantly across all six items of a questionnaire assessing their general knowledge of asthma. The proportion of patients who made errors while manipulating their inhalers was reduced to less than 10%. The ACT score increased from 16.6±4.6 to 20.0±3.9 (p<0.001). The number of asthmatics whose ACT score was at least 20 increased from 45 (33.3%) to 93 (65.3%) (p<0.001). The magnitude of improvement in the ACT score did not differ between patients who received an education session at least three times within 1 year and those who had not. The majority of patients agreed to the need for an education program (95.8%) and showed a willingness to pay an additional cost for the education (81.9%).
CONCLUSION
This study indicated that our newly developed education program would become an effective component of asthma management in primary care clinics.
Keyword
MeSH Terms
Figure
Reference
-
1. Global Initiative for Asthma. Global strategy for asthma management and prevention. Global Initiative for Asthma;2016.2. FitzGerald JM, Boulet LP, McIvor RA, Zimmerman S, Chapman KR. Asthma control in Canada remains suboptimal: the Reality of Asthma Control (TRAC) study. Can Respir J. 2006; 13:253–259.3. Lee JY, Yoo KH, Kim DK, Kim SH, Kim TE, Kim TH, et al. Effects of educational interventions for chronic airway disease on primary care. J Korean Med Sci. 2016; 31:1069–1074.4. Boulet LP, Boulay ME, Gauthier G, Battisti L, Chabot V, Beauchesne MF, et al. Benefits of an asthma education program provided at primary care sites on asthma outcomes. Respir Med. 2015; 109:991–1000.5. Martin MA, Mosnaim GS, Rojas D, Hernandez O, Sadowski LS. Evaluation of an asthma medication training program for immigrant Mexican community health workers. Prog Community Health Partnersh. 2011; 5:95–103.6. Health Insurance Review and Assessment Service [Internet]. Wonju: Health Insurance Review and Assessment Service;2013. cited 2017 Feb 2. Available from: https://www.hira.or.kr.7. Cloutier MM, Schatz M, Castro M, Clark N, Kelly HW, Mangione-Smith R, et al. Asthma outcomes: composite scores of asthma control. J Allergy Clin Immunol. 2012; 129:3 Suppl. S24–S33.8. Kim DK, Park YB, Oh YM, Jung KS, Yoo JH, Yoo KH, et al. Korean asthma guideline 2014: summary of major updates to the Korean asthma guideline 2014. Tuberc Respir Dis. 2016; 79:111–120.9. Plaza Moral V, Alonso Mostaza S, Alvarez Rodriguez C, Gomez-Outes A, Gomez Ruiz F, Lopez Vina A, et al. Spanish guideline on the management of asthma. J Investig Allergol Clin Immunol. 2016; 26:Suppl 1. 1–92.10. Kim S, Kim J, Kim K, Kim Y, Park Y, Baek S, et al. Healthcare use and prescription patterns associated with adult asthma in Korea: analysis of the NHI claims database. Allergy. 2013; 68:1435–1442.11. Adams RJ, Fuhlbrigge A, Guilbert T, Lozano P, Martinez F. Inadequate use of asthma medication in the United States: results of the asthma in America national population survey. J Allergy Clin Immunol. 2002; 110:58–64.12. Cazzoletti L, Marcon A, Janson C, Corsico A, Jarvis D, Pin I, et al. Asthma control in Europe: a real-world evaluation based on an international population-based study. J Allergy Clin Immunol. 2007; 120:1360–1367.13. Kim SH, Cho BL, Shin DW, Hwang SS, Lee H, Ahn EM, et al. The effect of asthma clinical guideline for adults on inhaled corticosteroids prescription trend: a quasi-experimental study. J Korean Med Sci. 2015; 30:1048–1054.14. Kelloway JS, Wyatt RA, Adlis SA. Comparison of patients' compliance with prescribed oral and inhaled asthma medications. Arch Intern Med. 1994; 154:1349–1352.15. Bae YJ, Kim TB, Jee YK, Park HW, Chang YS, Cho SH, et al. Severe asthma patients in Korea overestimate their adherence to inhaled corticosteroids. J Asthma. 2009; 46:591–595.16. Capanoglu M, Dibek Misirlioglu E, Toyran M, Civelek E, Kocabas CN. Evaluation of inhaler technique, adherence to therapy and their effect on disease control among children with asthma using metered dose or dry powder inhalers. J Asthma. 2015; 52:838–845.17. Price D, David-Wang A, Cho SH, Ho JC, Jeong JW, Liam CK, et al. Asthma in Asia: physician perspectives on control, inhaler use and patient communications. J Asthma. 2016; 53:761–769.18. Arora P, Kumar L, Vohra V, Sarin R, Jaiswal A, Puri MM, et al. Evaluating the technique of using inhalation device in COPD and bronchial asthma patients. Respir Med. 2014; 108:992–998.19. Oliveira PD, Menezes AM, Bertoldi AD, Wehrmeister FC, Macedo SE. Assessment of inhaler techniques employed by patients with respiratory diseases in southern Brazil: a population-based study. J Bras Pneumol. 2014; 40:513–520.20. Al-Jahdali H, Ahmed A, Al-Harbi A, Khan M, Baharoon S, Bin Salih S, et al. Improper inhaler technique is associated with poor asthma control and frequent emergency department visits. Allergy Asthma Clin Immunol. 2013; 9:8.21. Al-Jahdali H, Anwar A, Al-Harbi A, Baharoon S, Halwani R, Al Shimemeri A, et al. Factors associated with patient visits to the emergency department for asthma therapy. BMC Pulm Med. 2012; 12:80.22. Gibson PG, Powell H, Coughlan J, Wilson AJ, Abramson M, Haywood P, et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev. 2003; (1):CD001117.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The learning characteristics of primary care physicians
- The Effects of the Video Education Program on the Residual urine, Gas Passing and State Anxiety of Hysterectomy Patients
- Effects of Video-centered Nursing Education Program on Anxiety, Uncertainty, and Self-care among Cataract Surgery Patients
- Effects of a Discharge Education Program using Computerized Animation Video for Post-operative Colon Cancer Patients
- Development of Computer-Tailored Education Program for Patients with Total Hip Replacement