J Korean Med Sci.
2016 Jul;31(7):1094-1099. 10.3346/jkms.2016.31.7.1094.
The Risk Factors and Pregnancy Outcomes of 48 Cases of Heterotopic Pregnancy from a Single Center
- Affiliations
-
- 1Division of Reproductive Endocrinology and Infertility, Department of Obstetrics and Gynecology, Cheil General Hospital and Women's Healthcare Center, Dankook University College of Medicine, Seoul, Korea. drgracekim1005@gmail.com
- 2Department of Medical Statistics & Informatics, School of Medicine, Catholic University of Daegu, Daegu, Korea.
- KMID: 2373729
- DOI: http://doi.org/10.3346/jkms.2016.31.7.1094
Abstract
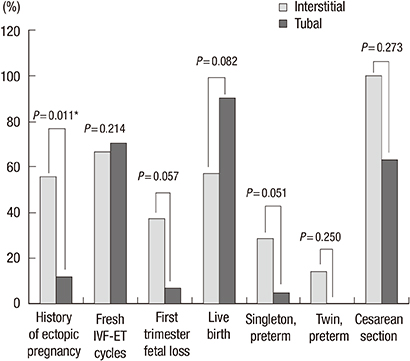
- The purpose of this study was to investigate risk factors that are associated with heterotopic pregnancy (HP) following in vitro fertilization (IVF)-embryo transfer (ET) and to demonstrate the outcomes of HP after the surgical treatment of ectopic pregnancies. Forty-eight patients from a single center, who were diagnosed with HP between 1998 and 2012 were included. All of the patients had received infertility treatments, such as Clomid with timed coitus (n = 1, 2.1%), superovulation with intrauterine insemination (n = 7, 14.6%), fresh non-donor IVF-ET (n = 33, 68.8%), and frozen-thawed cycles (n = 7, 14.6%). Eighty-four additional patients were randomly selected as controls from the IVF registry database. HP was diagnosed at 7.5 ± 1.2 weeks (range 5.4-10.3) gestational age. In six cases (12.5%), the diagnosis was made three weeks after the patients underwent treatment for abortion. There were significant differences in the history of ectopic pregnancy (22.5% vs. 3.6%, P = 0.002). There were no significant differences in either group between the rates of first trimester intrauterine fetal loss (15.0% vs. 13.1%) or live birth (80.0% vs. 84.1%) after the surgical treatment for ectopic pregnancy. The risk factors for HP include a history of ectopic pregnancy (OR 7.191 [1.591-32.513], P = 0.010), abortion (OR 3.948 [1.574-9.902], P = 0.003), and ovarian hyperstimulation syndrome (OHSS) (OR 10.773 [2.415-48.060], P = 0.002). In patients undergoing IVF-ET, history of ectopic pregnancy, abortion, and OHSS may be risk factors for HP as compared to the control group of other IVF patients. The surgical treatment of HP does not appear to affect the rates of first trimester fetal loss or live birth.
Keyword
MeSH Terms
Figure
Reference
-
1. Rizk B, Tan SL, Morcos S, Riddle A, Brinsden P, Mason BA, Edwards RG. Heterotopic pregnancies after in vitro fertilization and embryo transfer. Am J Obstet Gynecol. 1991; 164:161–164.2. Dor J, Seidman DS, Levran D, Ben-Rafael Z, Ben-Shlomo I, Mashiach S. The incidence of combined intrauterine and extrauterine pregnancy after in vitro fertilization and embryo transfer. Fertil Steril. 1991; 55:833–834.3. Marcus SF, Macnamee M, Brinsden P. Heterotopic pregnancies after in-vitro fertilization and embryo transfer. Hum Reprod. 1995; 10:1232–1236.4. Marcus SF, Brinsden PR. Analysis of the incidence and risk factors associated with ectopic pregnancy following in-vitro fertilization and embryo transfer. Hum Reprod. 1995; 10:199–203.5. Clayton HB, Schieve LA, Peterson HB, Jamieson DJ, Reynolds MA, Wright VC. A comparison of heterotopic and intrauterine-only pregnancy outcomes after assisted reproductive technologies in the United States from 1999 to 2002. Fertil Steril. 2007; 87:303–309.6. Soriano D, Shrim A, Seidman DS, Goldenberg M, Mashiach S, Oelsner G. Diagnosis and treatment of heterotopic pregnancy compared with ectopic pregnancy. J Am Assoc Gynecol Laparosc. 2002; 9:353–358.7. Luo X, Lim CE, Huang C, Wu J, Wong WS, Cheng NC. Heterotopic pregnancy following in vitro fertilization and embryo transfer: 12 cases report. Arch Gynecol Obstet. 2009; 280:325–329.8. Shah Y, Zevallos H, Moody L. Combined intra- and extrauterine pregnancy. A diagnostic challenge. J Reprod Med. 1980; 25:290–292.9. Dimitry ES, Subak-Sharpe R, Mills M, Margara R, Winston R. Nine cases of heterotopic pregnancies in 4 years of in vitro fertilization. Fertil Steril. 1990; 53:107–110.10. Tummon IS, Whitmore NA, Daniel SA, Nisker JA, Yuzpe AA. Transferring more embryos increases risk of heterotopic pregnancy. Fertil Steril. 1994; 61:1065–1067.11. Verhulst G, Camus M, Bollen N, Van Steirteghem A, Devroey P. Analysis of the risk factors with regard to the occurrence of ectopic pregnancy after medically assisted procreation. Hum Reprod. 1993; 8:1284–1287.12. Reece EA, Petrie RH, Sirmans MF, Finster M, Todd WD. Combined intrauterine and extrauterine gestations: a review. Am J Obstet Gynecol. 1983; 146:323–330.13. Buckett WM, Chian RC, Dean NL, Sylvestre C, Holzer HE, Tan SL. Pregnancy loss in pregnancies conceived after in vitro oocyte maturation, conventional in vitro fertilization, and intracytoplasmic sperm injection. Fertil Steril. 2008; 90:546–550.14. Barlow P, Lejeune B, Puissant F, Englert Y, Van Rysselberge M, Degueldre M, Vekemans M, Leroy F. Early pregnancy loss and obstetrical risk after in-vitro fertilization and embryo replacement. Hum Reprod. 1988; 3:671–675.15. Soriano D, Vicus D, Schonman R, Mashiach R, Shashar-Levkovitz D, Schiff E, Seidman DS, Goldenberg M. Long-term outcome after laparoscopic treatment of heterotopic pregnancy: 19 cases. J Minim Invasive Gynecol. 2010; 17:321–324.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Heterotopic Pregnancy following in vitro fertilization: transcervical evacuation with preserved intrauterine pregnancy
- A case of heterotopic pregnancy
- A case of heterotopic pregnancy: 16 weeks of intrauterine pregnancy with fetal Edwards syndrome and tubal pregnancy, following IVF-ET
- A Case of Discovery of Heterotopic Pregnancy After Elective Abortion
- A Case of Heterotopic Pregnancy Diagnosed after the Operation of Left Tubal Pregnancy