Korean J Gastroenterol.
2015 Feb;65(2):118-122. 10.4166/kjg.2015.65.2.118.
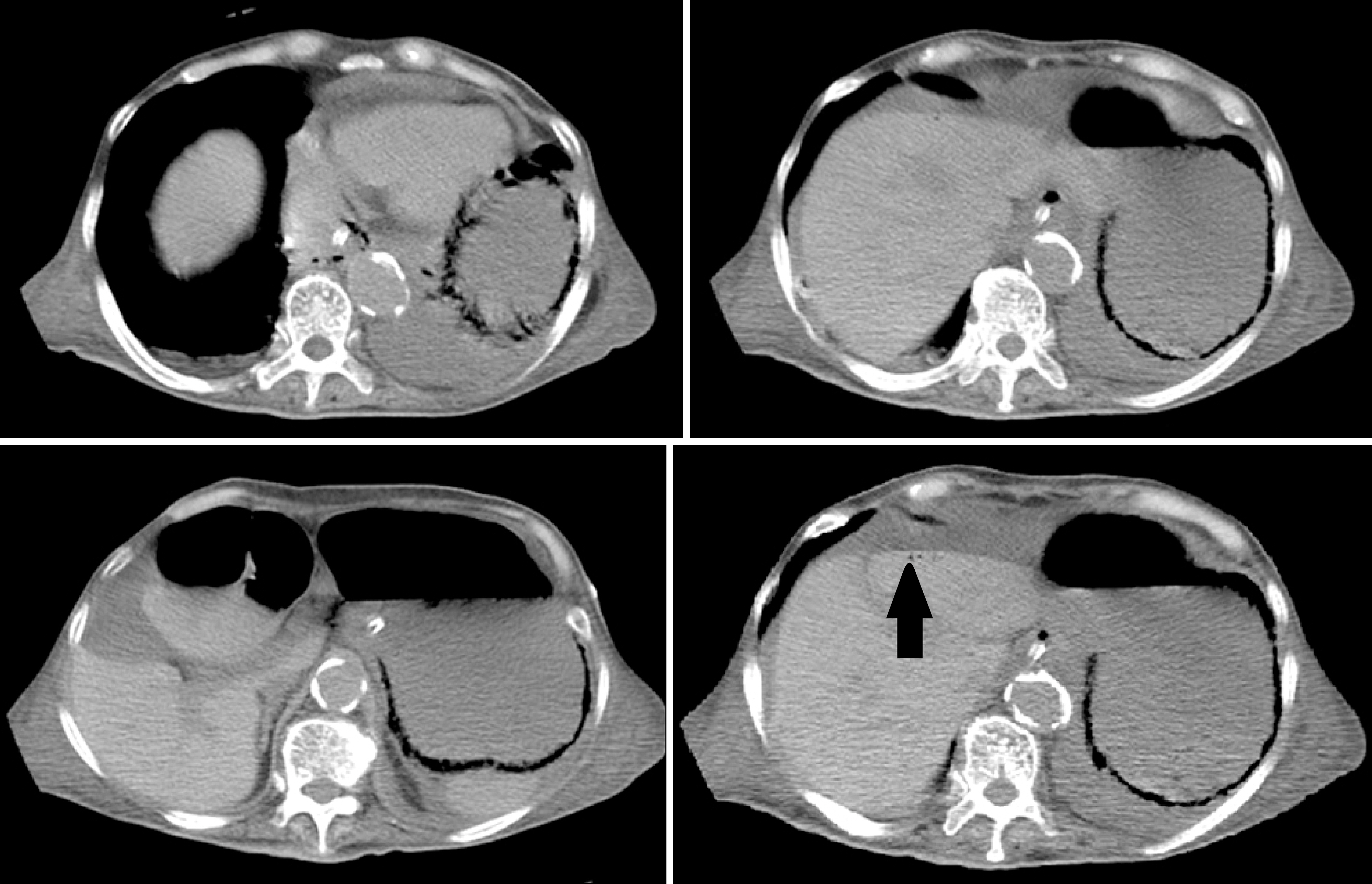
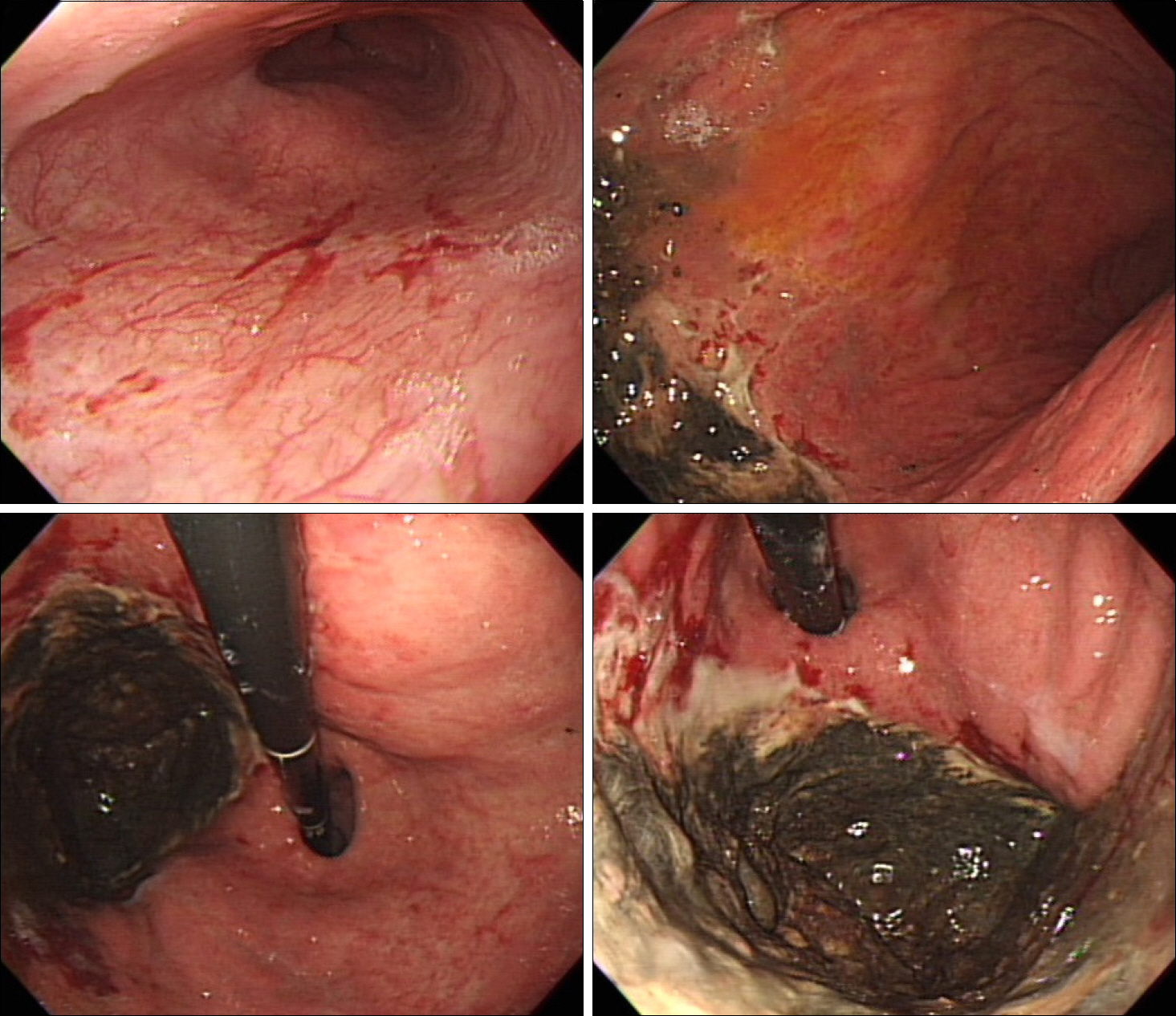
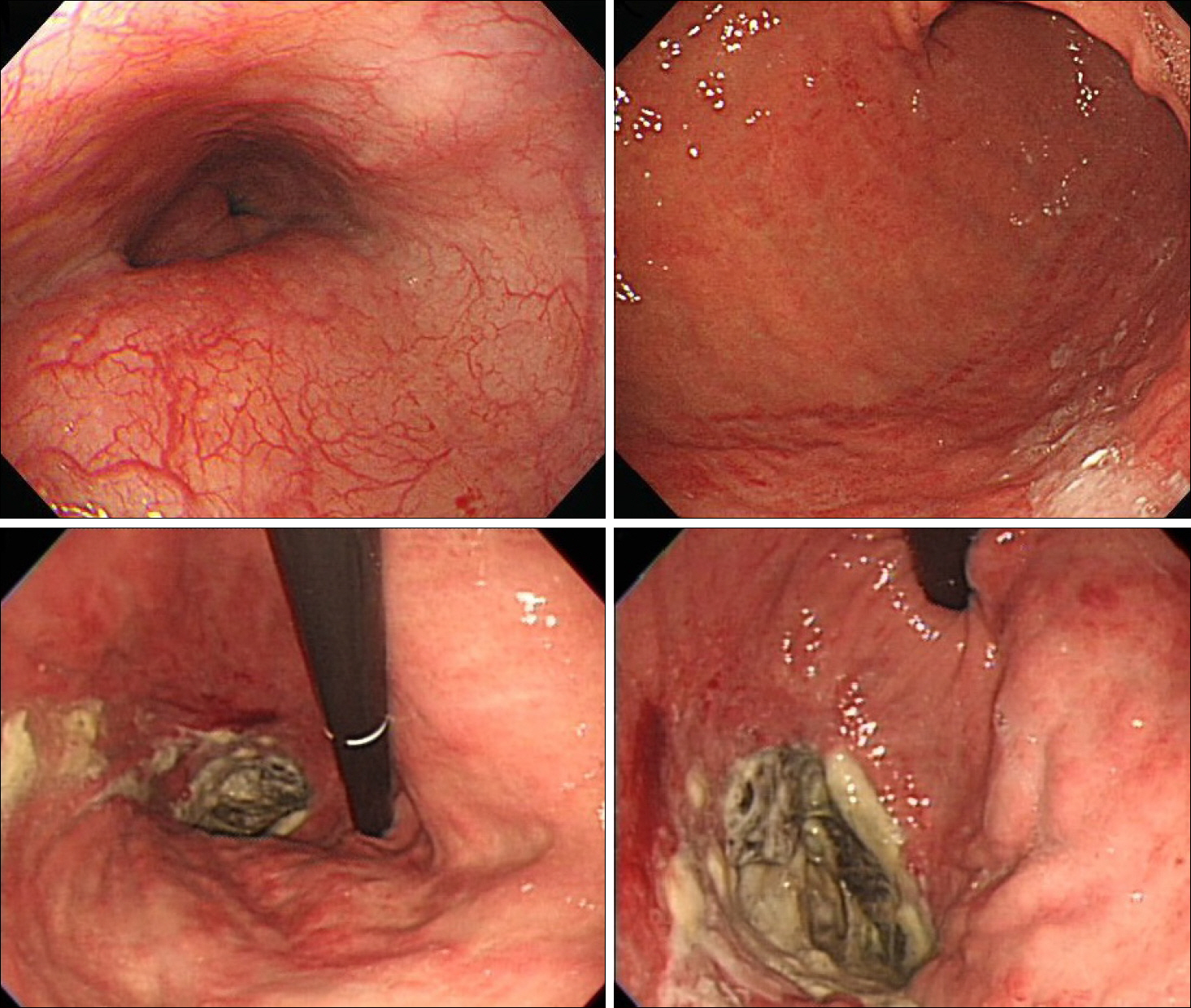
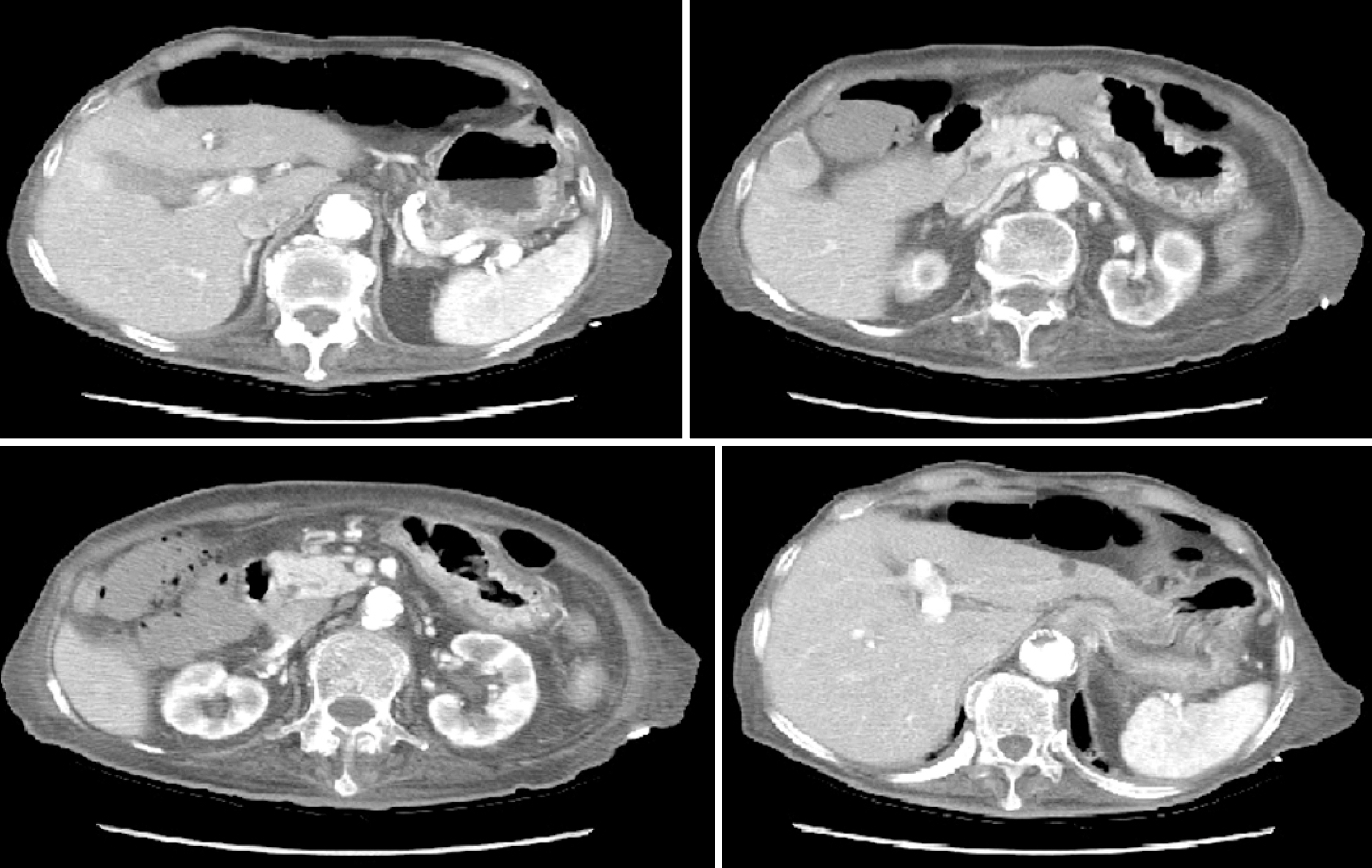
Emphysematous Gastritis with Concomitant Portal Venous Air
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. jikim@catholic.ac.kr
- KMID: 2373193
- DOI: http://doi.org/10.4166/kjg.2015.65.2.118
Abstract
- Emphysematous gastritis is a rare form of gastritis caused by infection of the stomach wall by gas forming bacteria. It is a very rare condition that carries a high mortality rate. Portal venous gas shadow represents elevation of intestinal luminal pressure which manifests as emphysematous gastritis or gastric emphysema. Literature reviews show that the mortality rate is especially high when portal venous gas shadow is present on CT scan. Until recently, the treatment of emphysematous gastritis has been immediate surgical intervention. However, there is a recent trend of avoiding surgery because of the frequent occurrence of post-operative complications such as anastomosis leakage. In addition, aggressive surgical treatment has failed to show significant improvement in prognosis. Recently, the authors experienced a case of emphysematous gastritis accompanied by portal venous gas which was treated successfully by conservative treatment without immediate surgical intervention. Herein, we present a case of emphysematous gastritis with concomitant portal venous air along with literature review.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Allan K, Barriga J, Afshani M, Davila R, Tombazzi C. Emphysematous gastritis. Am J Med Sci. 2005; 329:205–207.
Article2. Al-Jundi W, Shebl A. Emphysematous gastritis: case report and literature review. Int J Surg. 2008; 6:e63–e66.
Article3. Lee SM, Kim GH, Kang DH, Kim TO, Song GA, Kim S. Education and imaging. Gastrointestinal: emphysematous gastritis. J Gastroenterol Hepatol. 2007; 22:2036.4. Loi TH, See JY, Diddapur RK, Issac JR. Emphysematous gastritis: a case report and a review of literature. Ann Acad Med Singapore. 2007; 36:72–73.5. Paul M, John S, Menon MC, Golewale NH, Weiss SL, Murthy UK. Successful medical management of emphysematous gastritis with concomitant portal venous air: a case report. J Med Case Rep. 2010; 4:140.
Article6. Szuchmacher M, Bedford T, Sukharamwala P, Nukala M, Parikh N, Devito P. Is surgical intervention avoidable in cases of emphysematous gastritis? A case presentation and literature review. Int J Surg Case Rep. 2013; 4:456–459.
Article7. Wormer BA, Mostafa G. Emphysematous gastritis with delayed gastric perforation. J Gastrointest Surg. 2013; 17:1336–1338.
Article8. Ng A, Spanger M, Lubel JS. Education and imaging. Hepatobiliary and pancreatic: emphysematous gastritis with hepatic portal venous gas. J Gastroenterol Hepatol. 2012; 27:1130.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Emphysematous Gastritis with Concomitant Portal Venous Air in a Healthy Woman
- Emphysematous Gastritis with Concomitant Portal Venous Air and Acute Necrotizing Esophagitis in Type 1 Diabetes with Diabetic Ketoacidosis: A Case Report and Literature Review of a Rare Complication in Diabetes
- CT finding of emphysematous gastritis
- Portal and superior mesenteric venous gas with retroperitoneal abscess: CT diagnosis (case report)
- A Case of Necrotizing Fasciitis and Severe Sepsis Complicated by Emphysematous Gastritis