Obstet Gynecol Sci.
2017 Mar;60(2):163-169. 10.5468/ogs.2017.60.2.163.
Predicting factors for success of vaginal delivery in preterm induction with prostaglandin Eâ‚‚
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ohsymd@skku.edu
- KMID: 2372800
- DOI: http://doi.org/10.5468/ogs.2017.60.2.163
Abstract
OBJECTIVE
To evaluate the efficacy and safety of prostaglandin (PG) Eâ‚‚ for preterm labor induction and to investigate the predictive factors for the success of vaginal delivery.
METHODS
A retrospective cohort study was performed in women (n=155) at 24+0 to 36+6 weeks of gestation who underwent induction of labor using a PGEâ‚‚ vaginal pessary (10 mg, Propess) from January 2009 to December 2015. Success rates of vaginal delivery according to gestational age at induction and incidence of intrapartum complications such as tachysystole and nonreassuring fetal heart rate were investigated. Multivariable logistic regression analysis was performed to evaluate the predictive factors for success of labor induction.
RESULTS
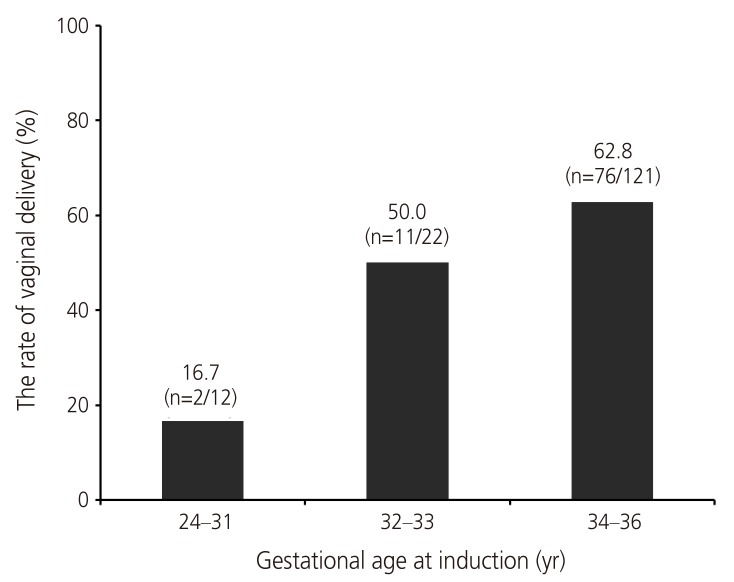
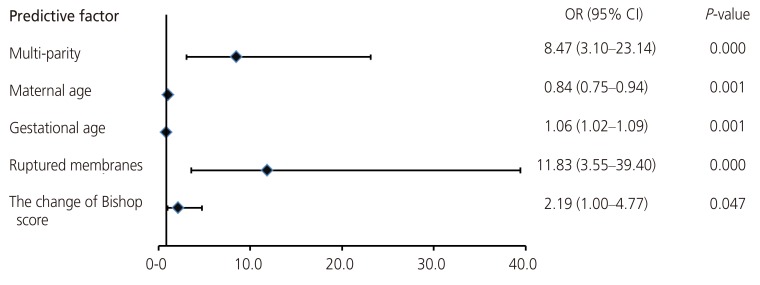
The vaginal delivery rate was 57% (n=89) and the rate of cesarean delivery after induction was 43% (n=66). According to gestational age, labor induction was successful in 16.7%, 50.0%, and 62.8% of patients at 24 to 31, 32 to 33, and 34 to 36 weeks, showing a stepwise increase (P=0.006). There were 18 cases (11%) of fetal distress, 9 cases (5.8%) of tachysystole, and 6 cases (3.8%) of massive postpartum bleeding (>1,000 mL). After adjusting for confounding factors, multiparity (odds ratio [OR], 8.47; 95% confidence interval [CI], 3.10 to 23.14), younger maternal age (OR, 0.84; 95% CI, 0.75 to 0.94), advanced gestational age at induction (OR, 1.06; 95% CI, 1.02 to 1.09), rupture of membranes (OR, 11.83; 95% CI, 3.55 to 39.40), and the Bishop score change after removal of PGEâ‚‚ (OR, 2.19; 95% CI, 1.0 to 4.8) were significant predictors of successful preterm vaginal delivery.
CONCLUSION
An understanding of the principal predictive factors of successful preterm labor induction, as well as the safety of PGEâ‚‚, will provide useful information when clinicians consult with preterm pregnant women requiring premature delivery.
MeSH Terms
Figure
Reference
-
1. Vrouenraets FP, Roumen FJ, Dehing CJ, van den Akker ES, Aarts MJ, Scheve EJ. Bishop score and risk of cesarean delivery after induction of labor in nulliparous women. Obstet Gynecol. 2005; 105:690–697. PMID: 15802392.
Article2. Hendricks CH, Brenner WE, Kraus G. Normal cervical dilatation pattern in late pregnancy and labor. Am J Obstet Gynecol. 1970; 106:1065–1082. PMID: 5435658.
Article3. ACOG Committee on Practice Bulletins Obstetrics. ACOG Practice Bulletin No. 107: Induction of labor. Obstet Gynecol. 2009; 114:386–397. PMID: 19623003.4. Min JA, Choi SJ, Jung KL, Oh SY, Kim JH, Roh CR. The clinical practice pattern of postterm pregnancy in Korea. Korean J Obstet Gynecol. 2007; 50:79–84.5. Kelly AJ, Kavanagh J, Thomas J. Vaginal prostaglandin (PGE2 and PGF2a) for induction of labour at term. Cochrane Database Syst Rev. 2003; 4:CD003101.
Article6. Abelin Tornblom S, Ostlund E, Granstrom L, Ekman G. Pre-term cervical ripening and labor induction. Eur J Obstet Gynecol Reprod Biol. 2002; 104:120–123. PMID: 12206923.7. Carlan SJ, O'Brien WF, Logan S. Serial intravaginal prostaglandin E2 gel cervical ripening in preterm pregnancies. Prostaglandins. 1996; 52:237–246. PMID: 8908623.
Article8. Moore LE, Rayburn WF. Elective induction of labor. Clin Obstet Gynecol. 2006; 49:698–704. PMID: 16885673.
Article9. Hofmeyr GJ, Gulmezoglu AM. Vaginal misoprostol for cervical ripening and induction of labour. Cochrane Database Syst Rev. 2003; (1):CD000941. PMID: 12535398.
Article10. Ray DA, Garite TJ. Prostaglandin E2 for induction of labor in patients with premature rupture of membranes at term. Am J Obstet Gynecol. 1992; 166:836–843. PMID: 1550149.
Article11. Ben-Haroush A, Yogev Y, Glickman H, Bar J, Kaplan B, Hod M. Mode of delivery in pregnancies with premature rupture of membranes at or before term following induction of labor with vaginal prostaglandin E2. Am J Perinatol. 2004; 21:263–268. PMID: 15232758.
Article12. Melamed N, Yogev Y, Hadar E, Hod M, Ben-Haroush A. Preinduction cervical ripening with prostaglandin E2 at preterm. Acta Obstet Gynecol Scand. 2008; 87:63–67. PMID: 18158629.13. Ehrenthal DB, Jiang X, Strobino DM. Labor induction and the risk of a cesarean delivery among nulliparous women at term. Obstet Gynecol. 2010; 116:35–42. PMID: 20567165.
Article14. Johnson DP, Davis NR, Brown AJ. Risk of cesarean delivery after induction at term in nulliparous women with an unfavorable cervix. Am J Obstet Gynecol. 2003; 188:1565–1569. PMID: 12824994.
Article15. Anderson AB, Turnbull AC. Relationship between length of gestation and cervical dilatation, uterine contractility, and other factors during pregnancy. Am J Obstet Gynecol. 1969; 105:1207–1214. PMID: 5360251.
Article16. Yogev Y, Ben-Haroush A, Gilboa Y, Chen R, Kaplan B, Hod M. Induction of labor with vaginal prostaglandin E2. J Matern Fetal Neonatal Med. 2003; 14:30–34. PMID: 14563089.
Article17. Prysak M, Castronova FC. Elective induction versus spontaneous labor: a case-control analysis of safety and efficacy. Obstet Gynecol. 1998; 92:47–52. PMID: 9649091.18. Lee HR, Kim MN, You JY, Choi SJ, Oh SY, Roh CR, et al. Risk of cesarean section after induced versus spontaneous labor at term gestation. Obstet Gynecol Sci. 2015; 58:346–352. PMID: 26430658.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Intravaginal Misoprostol and Prostaglandin E2 Vaginal Tablet in Termination of Mid - Trimester Pregnancy
- Vaginal Birth after Cesarean Delivery : Development of a Scoring System for Predicting Success Rate
- Randomized comparison of vaginal prostaglandin E2 pessary with vaginal prostaglandin E2 tablet for the induction of labor
- Expression of Tissue Tissue-transglutaminase-2 (TGM2) and Cyclo-oxygenase (COX) in the Fetal Membrane of Preterm Birth
- Uterine Cervical Length Measurement by Transvaginal Ultrasonography for Prediction of Preterm Delivery