J Gastric Cancer.
2010 Dec;10(4):247-253.
Comparison of Learning Curves and Clinical Outcomes between Laparoscopy-assisted Distal Gastrectomy and Open Distal Gastrectomy
- Affiliations
-
- 1Department of Surgery, Chonbuk National University Medical School, Jeonju, Korea. happyhill@jbnu.ac.kr
Abstract
- PURPOSE
Most stomach surgeons have been educated sufficiently in conventional open distal gastrectomy (ODG) but insufficiently in laparoscopy-assisted distal gastrectomy (LADG). We compared learning curves and clinical outcomes between ODG and LADG by a single surgeon who had sufficient education of ODG and insufficient education of LADG.
MATERIALS AND METHODS
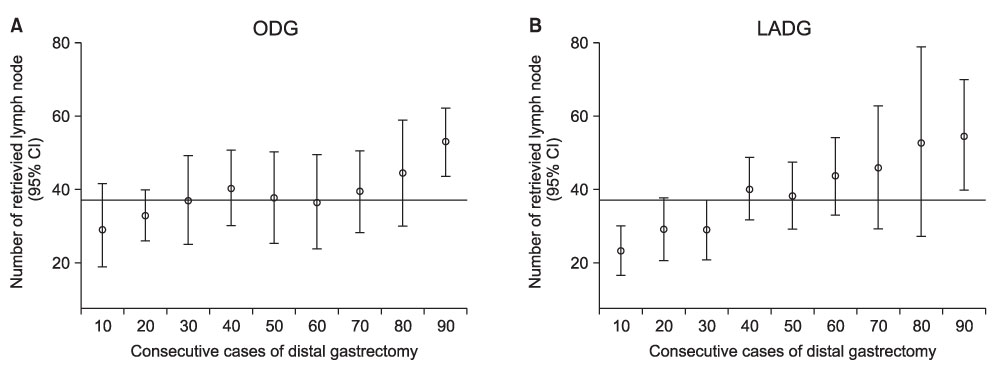
ODG (90 patients, January through September, 2004) and LADG groups (90 patients, June 2006 to June 2007) were compared. The learning curve was assessed with the mean number of retrieved lymph nodes, operation time, and postoperative morbidity/mortality.
RESULTS
Mean operation time was 168.3 minutes for ODG and 183.6 minutes for LADG. The mean number of retrieved lymph nodes was 37.9. Up to about the 20th to 25th cases, the slope decrease in the learning curve for LADG was more apparent than for ODG, although they both reached plateaus after the 50th cases. The mean number of retrieved lymph nodes reached the overall mean after the 30th and 40th cases for ODG and LADG, respectively. For ODG, complications were evenly distributed throughout the subgroups, whereas for LADG, complications occurred in 10 (33.3%) of the first 30 cases.
CONCLUSIONS
Compared with conventional ODG, LADG is feasible, in particular for a surgeon who has had much experience with conventional ODG, although LADG required more operative time, slightly more time to get adequately retrieved lymph nodes and more complications. However, there were more minor problems in the first 30 LADG than ODG cases. The unfavorable results for LADG can be overcome easily through an adequate training program for LADG.
Keyword
Figure
Reference
-
1. Crew KD, Neugut AI. Epidemiology of gastric cancer. World J Gastroenterol. 2006. 12:354–362.
Article2. Goh PM, Alponat A, Mak K, Kum CK. Early international results of laparoscopic gastrectomies. Surg Endosc. 1997. 11:650–652.
Article3. Adachi Y, Shiraishi N, Shiromizu A, Bandoh T, Aramaki M, Kitano S. Laparoscopy-assisted Billroth I gastrectomy compared with conventional open gastrectomy. Arch Surg. 2000. 135:806–810.
Article4. Etoh T, Shiraishi N, Kitano S. Laparoscopic gastrectomy for cancer. Dig Dis. 2005. 23:113–118.
Article5. Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 2002. 131:1 suppl. S306–S311.
Article6. Kitano S, Bandoh T, Kawano K. Endoscopic surgery in Japan. Minim Invasive Ther Allied Technol. 2001. 10:215–219.
Article7. Sobin LH, Wittekind C, editors. International Union Against Cancer (UICC): TNM Classification of Malignant Tumor. 2002. 6th ed. New York: Wiley-Liss.8. Sachdeva AK, Russell TR. Safe introduction of new procedures and emerging technologies in surgery: education, credentialing, and privileging. Surg Oncol Clin N Am. 2007. 16:101–114.
Article9. Schmidt RA, Lee T, editors. Motor Control and Learning: A Behavioral Emphasis. 2005. 4th ed. Champaign, Human Kinetics.10. Kim MC, Jung GJ, Kim HH. Learning curve of laparoscopy-assisted distal gastrectomy with systemic lymphadenectomy for early gastric cancer. World J Gastroenterol. 2005. 11:7508–7511.
Article11. Kim JH, Jung YS, Kim BS, Jeong O, Lim JT, Yook JH, et al. Learning curve of a laparoscopy assisted distal gastrectomy for a surgeon expert in performing a conventional open gastrectomy. J Korean Gastric Cancer Assoc. 2006. 6:167–172.
Article12. Kim KC, Yook JH, Choi JE, Cheong O, Lim JT, Oh ST, et al. The Learning Curve of Laparoscopy-assisted Distal Gastrectomy (LADG) for cancer. J Korean Gastric Cancer Assoc. 2008. 8:232–236.
Article13. Yoo CH, Kim HO, Hwang SI, Son BH, Shin JH, Kim H. Short-term outcomes of laparoscopic-assisted distal gastrectomy for gastric cancer during a surgeon's learning curve period. Surg Endosc. 2009. 23:2250–2257.
Article14. Jin SH, Kim DY, Kim H, Jeong IH, Kim MW, Cho YK, et al. Multidimensional learning curve in laparoscopy-assisted gastrectomy for early gastric cancer. Surg Endosc. 2007. 21:28–33.
Article15. Dinçler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P. Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectum. 2003. 46:1371–1378.
Article16. Forbes TL. A cumulative analysis of an individual surgeon's early experience with elective open abdominal aortic aneurysm repair. Am J Surg. 2005. 189:469–473.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Totally Laparoscopic Distal Gastrectomy after Learning Curve Completion: Comparison with Laparoscopy-Assisted Distal Gastrectomy
- Comparison of laparoscopy-assisted and totally laparoscopic Billroth-II distal gastrectomy for gastric cancer
- Comparison of Laparoscopy-Assisted and Totally Laparoscopic Distal Gastrectomy: The Short-Term Outcome at a Low Volume Center
- Comparison of a Postoperative Pain in Laparoscopy-Assisted Distal Gastrectomy and Totally Laparoscopic Distal Gastrectomy according to the Location of the Mini-Laparotomy Site
- Laparoscopy-Assisted Distal Gastrectomy for Early Gastric Cancer in the Elderly