J Gastric Cancer.
2010 Dec;10(4):196-205.
Prognostic Significance of Preoperative Blood Transfusion in Stomach Cancer
- Affiliations
-
- 1Department of Surgery, Research Institute for Medical Science, Chungnam National Universuty School of Medicine, Daejeon, Korea. seungnoh@cnu.ac.kr
Abstract
- PURPOSE
We did a retrospective study to understand the prognostic effects of preoperative blood transfusions in stomach cancer surgery.
MATERIALS AND METHODS
Data for 1,360 patients who underwent gastrectomy for stomach cancer between 2001 and 2009 were retrospectively reviewed. We analyzed factors that affect preoperative transfusion and clinicopathologic features. We also analyzed 5-year and overall survival rates of the transfusion and non transfusion subgroups.
RESULTS
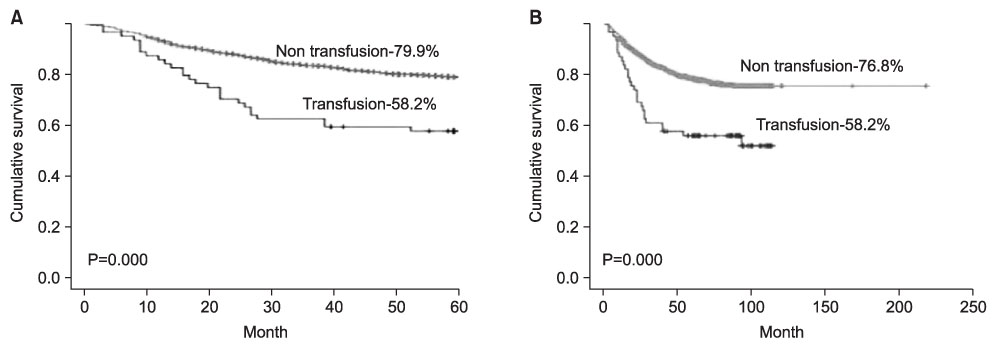
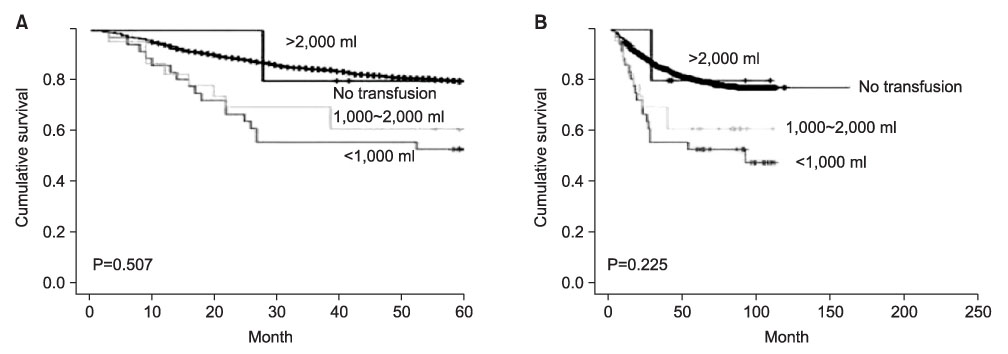
Sixty patients (4.4%) required blood transfusion within the preoperative period. The transfused group included patients who took aspirin or clopidogrel (P<0.001), with more advanced T stages (P<0.001), with more advanced nodal metastasis (P=0.00), and with more advanced stages (P=0.00) than the non transfusion group. On multivariate analysis, preoperative transfusion was a statistically significant negative influence on 5-year survival and overall survival rates (58.2% vs 79.9% (P=0.00), 58.2% vs 76.8% (P=0.00)). Applying Cox-regression analyses, blood transfusion did appear to have an effect on prognosis and on 5-year and overall survival rates.
CONCLUSIONS
We found a direct negative relation between preoperative transfusion and long term prognosis in patients receiving gastric cancer surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Ministry of Health in Japan. About the use of blood products. 2007. 3rd ed.2. Hyung WJ, Noh SH, Shin DW, Huh J, Huh BJ, Choi SH, et al. Adverse effects of perioperative transfusion on patients with stage III and IV gastric cancer. Ann Surg Oncol. 2002. 9:5–12.
Article3. Amato A, Pescatori M. Perioperative blood transfusions for the recurrence of colorectal cancer. Cochrane Database Syst Rev. 2006. (1):CD005033.
Article4. Nilsson KR, Berenholtz SM, Dorman T, Garrett E, Lipsett P, Kaufman HS, et al. Preoperative predictors of blood transfusion in colorectal cancer surgery. J Gastrointest Surg. 2002. 6:753–762.
Article5. Centers for Disease Control of Health and Welfare in Korea. Institute of Transfusion in Korea. Guidelines for transfusion. 2009.6. Murphy MF, Wallington TB, Kelsey P, Boulton F, Bruce M, Cohen H, et al. British Committee for Standards in Haematology. Blood Transfusion Task Force. Guidelines for the clinical use of red cell transfusions. Br J Haematol. 2001. 113:24–31.
Article7. British Committee for Standards in Haematology. Stainsby D, MacLennan S, Thomas D, Isaac J, Hamilton PJ. Guidelines on the management of massive blood loss. Br J Haematol. 2006. 135:634–641.
Article8. Wilkerson DK, Rosen AL, Sehgal LR, Gould SA, Sehgal HL, Moss GS. Limits of cardiac compensation in anemic baboons. Surgery. 1988. 103:665–670.9. Kaneda M, Horimi T, Ninomiya M, Nagae S, Mukai K, Takeda I, et al. Adverse affect of blood transfusions on survival of patients with gastric cancer. Transfusion. 1987. 27:375–377.
Article10. Kampschöer GH, Maruyama K, Sasako M, Kinoshita T, van de Velde CJ. The effects of blood transfusion on the prognosis of patients with gastric cancer. World J Surg. 1989. 13:637–643.
Article11. Moriguchi S, Maehara Y, Akazawa K, Sugimachi K, Nose Y. Lack of relationship between perioperative blood transfusion and survival time after curative resection for gastric cancer. Cancer. 1990. 66:2331–2335.
Article12. Fong Y, Karpeh M, Mayer K, Brennan MF. Association of perioperative transfusions with poor outcome in resection of gastric adenocarcinoma. Am J Surg. 1994. 167:256–260.
Article13. Singh SK, Marquet RL, de Bruin RW, Hop WC, Westbroek DL, Jeekel J. Consequences of blood loss on growth of artificial metastases. Br J Surg. 1988. 75:377–379.
Article14. Benoist S, Panis Y, Pannegeon V, Alves A, Valleur P. Predictive factors for perioperative blood transfusions in rectal resection for cancer: A multivariate analysis of a group of 212 patients. Surgery. 2001. 129:433–439.
Article15. Vamvakas EC, Carven JH. Allogeneic blood transfusion, hospital charges, and length of hospitalization: a study of 487 consecutive patients undergoing colorectal cancer resection. Arch Pathol Lab Med. 1998. 122:145–151.16. Matsumata T, Itasaka H, Shirabe K, Shimada M, Yanaga K, Sugimachi K. Strategies for reducing blood transfusions in hepatic resection. HPB Surg. 1994. 8:1–6.
Article17. Opelz G, Terasaki PI. Poor kidney-transplant survival in recipients with frozen-blood transfusions or no transfusions. Lancet. 1974. 2:696–698.
Article18. Taylor RW, Manganaro L, O'Brien J, Trottier SJ, Parkar N, Veremakis C. Impact of allogenic packed red blood cell transfusion on nosocomial infection rates in the critically ill patient. Crit Care Med. 2002. 30:2249–2254.
Article19. Nowak MM, Ponsky JL. Blood transfusion and disease-free survival in carcinoma of the breast. J Surg Oncol. 1984. 27:124–130.
Article20. Hyman NH, Foster RS Jr, DeMeules JE, Costanza MC. Blood transfusions and survival after lung cancer resection. Am J Surg. 1985. 149:502–507.
Article21. Manyonda IT, Shaw DE, Foulkes A, Osborn DE. Renal cell carcinoma: blood transfusion and survival. Br Med J (Clin Res Ed). 1986. 293:537–538.
Article22. Johnson JT, Taylor FH, Thearle PB. Blood transfusion and outcome in stage III head and neck carcinoma. Arch Otolaryngol Head Neck Surg. 1987. 113:307–310.
Article23. Grzelak I, Zaleska M, Olszewski WL. Blood transfusions downregulate hematopoiesis and subsequently downregulate the immune response. Transfusion. 1998. 38:1104–1114.
Article24. Carson JL, Chen AY. In search of the transfusion trigger. Clin Orthop Relat Res. 1998. 357:30–35.
Article25. Chen AY, Carson JL. Perioperative management of anaemia. Br J Anaesth. 1998. 81:Suppl 1. 20–24.26. Carson JL, Duff A, Poses RM, Berlin JA, Spence RK, Trout R, et al. Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet. 1996. 348:1055–1060.
Article27. Practice Guidelines for blood component therapy: a report by the American society of anesthesiologists task force on blood component therapy. Anesthesiology. 1996. 84:732–747.28. Consensus Conference. Perioperative red blood cell transfusion. JAMA. 1988. 260:2700–2703.29. van de Watering LM, Hermans J, Houbiers JG, van den Broek PJ, Bouter H, Boer F, et al. Beneficial effects of leukocyte depletion of transfused blood on postoperative complications in patients undergoing cardiac surgery: a randomized clinical trial. Circulation. 1998. 97:562–568.
Article30. Naidech AM, Drescher J, Ault ML, Shaibani A, Batjer HH, Alberts MJ. Higher hemoglobin is associated with less cerebral infarction, poor outcome, and death after subarachnoid hemorrhage. Neurosurgery. 2006. 59:775–779.
Article31. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987. 40:373–383.
Article32. Lübke T, Mönig SP, Schneider PM, Hölscher AH, Bollschweiler E. Does Charlson-comorbidity index correlate with short-term outcome in patients with gastric cancer? Zentralbl Chir. 2003. 128:970–976.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Prognostic Significance of Transfusion in Periampullary Cancer Following Pancreatoduodenectomy
- Effects of Perioperative Transfusion in Gastric Cancer
- The Relationship between Perioperative Blood Transfusion and Prognosis in Stomach Cancer
- A Study upon the Changes of Hemoglobin and Hematocrit between Preoperative and Postoperative Values
- Preoperative consultation for determining the appropriate transfusion strategy