J Gastric Cancer.
2012 Dec;12(4):237-242.
Laparoscopic Primary Repair with Omentopexy for Duodenal Ulcer Perforation: A Single Institution Experience of 21 Cases
- Affiliations
-
- 1Department of Surgery, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea. md9650@hanyang.ac.kr
Abstract
- PURPOSE
Despite the great advances in laparoscopic techniques, most active general surgeons do not apply laparoscopic surgery in the treatment of duodenal ulcer perforation when facing a real-life emergency. Therefore, our study was designed to evaluate the feasibility of laparoscopic surgery in duodenal ulcer perforation, and provide a step-by-step protocol with tips and recommendations for less experienced surgeons.
MATERIALS AND METHODS
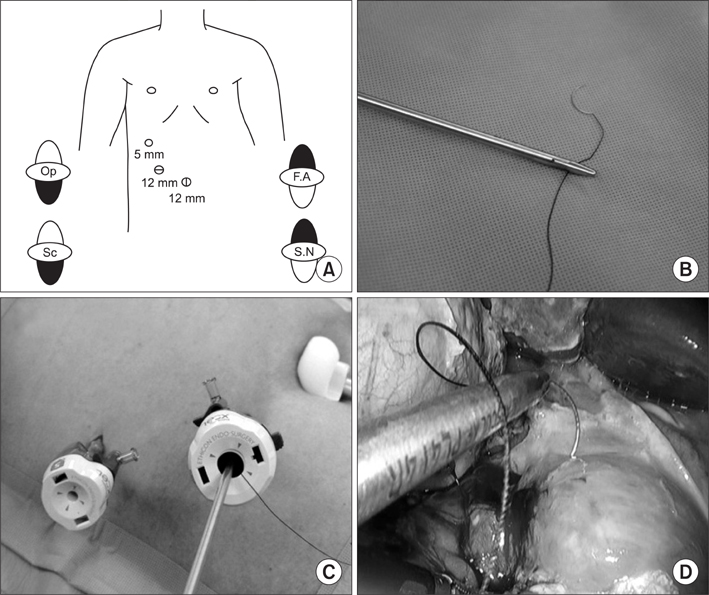
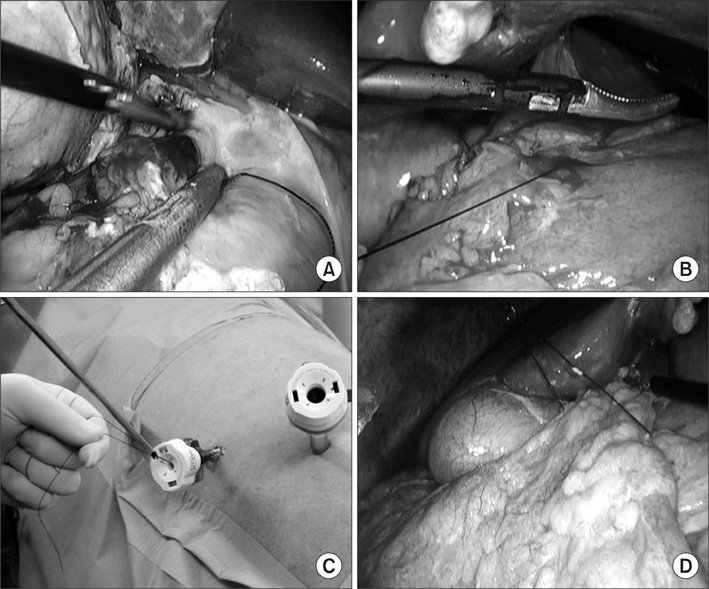
Between March, 2011 and May, 2012, 21 patients presenting with duodenal ulcer perforation underwent laparoscopic primary repair with omentopexy. There were no contraindications to perform laparoscopic surgery, and the choice of primary repair was decided according to the size of the perforation. The procedure for laparoscopic primary repair with omentopexy consisted of peritoneal lavage, primary suture, and omentopexy using a knot pusher.
RESULTS
During the operation, no conversion to open surgery or intra-operative events occurred. The median operation time was 45.0 minutes (20~80 minutes). Median day of commencement of a soft diet was day 6 (4~17 days). After surgery, the median hospital stay was 8.0 days (5~27 days). Postoperative complications occurred in one patient, which included a minor leakage. This complication was resolved by conservative management.
CONCLUSIONS
Although our study was carried out on a small number of patients at a single institution, we conclude that laparoscopic primary repair can be an effective surgical method in the treatment of duodenal ulcer perforation. We believe that the detailed explanation of our procedure will help beginners to perform laparoscopic primary repair more easily.
Keyword
MeSH Terms
Figure
Reference
-
1. Abdel-Salam WN, Katri KM, Bessa SS, El-Kayal el-SA. Laparoscopic-assisted truncal vagotomy and gastro-jejunostomy: trial of simplification. J Laparoendosc Adv Surg Tech A. 2009. 19:125–127.
Article2. Jani K, Saxena AK, Vaghasia R. Omental plugging for large-sized duodenal peptic perforations: a prospective randomized study of 100 patients. South Med J. 2006. 99:467–471.
Article3. Lal P, Vindal A, Hadke NS. Controlled tube duodenostomy in the management of giant duodenal ulcer perforation: a new technique for a surgically challenging condition. Am J Surg. 2009. 198:319–323.
Article4. Lam PW, Lam MC, Hui EK, Sun YW, Mok FP. Laparoscopic repair of perforated duodenal ulcers: the "three-stitch" Graham patch technique. Surg Endosc. 2005. 19:1627–1630.
Article5. Lee J, Sung K, Lee D, Lee W, Kim W. Single-port laparoscopic repair of a perforated duodenal ulcer: intracorporeal "cross and twine" knotting. Surg Endosc. 2011. 25:229–233.6. Song KY, Kim TH, Kim SN, Park CH. Laparoscopic repair of perforated duodenal ulcers: the simple "one-stitch" suture with omental patch technique. Surg Endosc. 2008. 22:1632–1635.7. Kim MG, Park HK, Park JJ, Lee HG, Nam YS. The applicability of laparoscopic gastrectomy in the surgical treatment of giant duodenal ulcer perforation. Surg Laparosc Endosc Percutan Tech. 2012. 22:122–126.
Article8. Lunevicius R, Morkevicius M. Comparison of laparoscopic versus open repair for perforated duodenal ulcers. Surg Endosc. 2005. 19:1565–1571.
Article9. Nathanson LK, Easter DW, Cuschieri A. Laparoscopic repair/peritoneal toilet of perforated duodenal ulcer. Surg Endosc. 1990. 4:232–233.
Article10. Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, et al. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg. 2002. 235:313–319.
Article11. Lau WY, Leung KL, Kwong KH, Davey IC, Rovertson C, Dawson JJ, et al. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg. 1996. 224:131–138.
Article12. Seelig MH, Seelig SK, Behr C, Schönleben K. Comparison between open and laparoscopic technique in the management of perforated gastroduodenal ulcers. J Clin Gastroenterol. 2003. 37:226–229.
Article13. Mehendale VG, Shenoy SN, Joshi AM, Chaudhari NC. Laparoscopic versus open surgical closure of perforated duodenal ulcers: a comparative study. Indian J Gastroenterol. 2002. 21:222–224.
Article14. Sø JB, Kum CK, Fernandes ML, Goh P. Comparison between laparoscopic and conventional omental patch repair for perforated duodenal ulcer. Surg Endosc. 1996. 10:1060–1063.
Article15. Siu WT, Chau CH, Law BK, Tang CN, Ha PY, Li MK. Routine use of laparoscopic repair for perforated peptic ulcer. Br J Surg. 2004. 91:481–484.
Article16. Robertson GS, Wemyss-Holden SA, Maddern GJ. Laparoscopic repair of perforated peptic ulcers. The role of laparoscopy in generalised peritonitis. Ann R Coll Surg Engl. 2000. 82:6–10.
Article17. Bergamaschi R, Mårvik R, Johnsen G, Thoresen JE, Ystgaard B, Myrvold HE. Open vs laparoscopic repair of perforated peptic ulcer. Surg Endosc. 1999. 13:679–682.
Article18. Michelet I, Agresta F. Perforated peptic ulcer: laparoscopic approach. Eur J Surg. 2000. 166:405–408.
Article19. Matsuda M, Nishiyama M, Hanai T, Saeki S, Watanabe T. Laparoscopic omental patch repair for perforated peptic ulcer. Ann Surg. 1995. 221:236–240.
Article20. Naesgaard JM, Edwin B, Reiertsen O, Trondsen E, Faerden AE, Rosseland AR. Laparoscopic and open operation in patients with perforated peptic ulcer. Eur J Surg. 1999. 165:209–214.
Article21. Jin SH, Kim DY, Kim H, Jeong IH, Kim MW, Cho YK, et al. Multidimensional learning curve in laparoscopy-assisted gastrectomy for early gastric cancer. Surg Endosc. 2007. 21:28–33.
Article22. Kim MC, Jung GJ, Kim HH. Learning curve of laparoscopy-assisted distal gastrectomy with systemic lymphadenectomy for early gastric cancer. World J Gastroenterol. 2005. 11:7508–7511.
Article23. Kunisaki C, Makino H, Yamamoto N, Sato T, Oshima T, Nagano Y, et al. Learning curve for laparoscopy-assisted distal gastrectomy with regional lymph node dissection for early gastric cancer. Surg Laparosc Endosc Percutan Tech. 2008. 18:236–241.
Article24. Zhang X, Tanigawa N. Learning curve of laparoscopic surgery for gastric cancer, a laparoscopic distal gastrectomy-based analysis. Surg Endosc. 2009. 23:1259–1264.
Article25. Kim MG, Kim KC, Yook JH, Kim BS, Kim TH, Kim BS. A practical way to overcome the learning period of laparoscopic gastrectomy for gastric cancer. Surg Endosc. 2011. 25:3838–3844.
Article26. Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009. 250:177–186.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Single Figure of Eight Suturing Omentopexy for the Treatment of a Perforated Duodenal Ulcer
- Perforation on the superior side of duodenum is a risk factor of laparoscopic primary repair for duodenal ulcer perforation
- Suture Omentopexy of Perforated Duodenal Ulcer: Laparoscopic vs. Open Surgery
- Laparoscopic Repair with Omental Patch for Perforated Duodenal Ulcer
- Covered Self-expandable Metallic Stent Insertion as a Rescue Procedure for Postoperative Leakage after Primary Repair of Perforated Duodenal Ulcer