J Gastric Cancer.
2012 Sep;12(3):173-178.
Transumbilical Single-Incision Laparoscopic Wedge Resection for Gastric Submucosal Tumors: Technical Challenges Encountered in Initial Experience
- Affiliations
-
- 1Gastric Cancer Branch, National Cancer Center, Goyang, Korea. kosmas@ncc.re.kr
Abstract
- PURPOSE
To report the initial clinical experience with single-incision laparoscopic gastric wedge resection for submucosal tumors.
MATERIALS AND METHODS
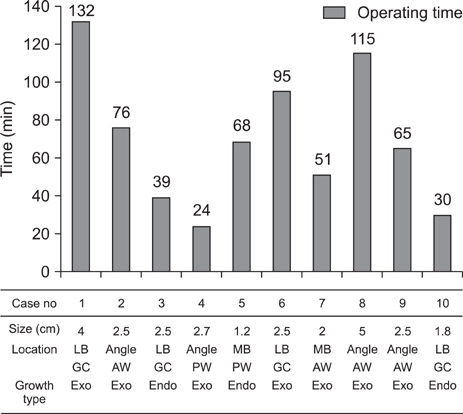
The medical records of 10 patients who underwent single-incision laparoscopic gastric wedge resection between July 2009 and March 2011 were reviewed retrospectively. The demographic data, clinicopathologic and surgical outcomes were assessed.
RESULTS
The mean tumor size was 2.5 cm (range, 1.2~5.0 cm), and the tumors were mostly located on the anterior wall (4/10) or along the greater curvature (4/10), of the stomach. Nine of ten procedures were performed successfully, without the use of additional trocars, or conversion to laparotomy. One patient underwent conversion to multiport laparoscopic surgery, to get simultaneous cholecystectomy safely. The mean operating time was 66.5 minutes (range, 24~132 minutes), and the mean postoperative hospital stay was 5 days (range, 4~7 days). No serious perioperative complications were observed. Of the 10 submucosal tumors, the final pathologic report revealed 5 gastrointestinal stromal tumors, 4 schwannomas, and 1 heterotopic pancreas.
CONCLUSIONS
Single-incision laparoscopic gastric wedge resection for gastric submucosal tumors is feasible and safe, when performed by experienced laparoscopic surgeons. This technique provides favorable cosmetic results, and also short hospital stay and low morbidity, in carefully selected candidates.
Keyword
MeSH Terms
Figure
Reference
-
1. Allori AC, Leitman IM, Heitman E. Natural orifice transluminal endoscopic surgery: lessons learned from the laparoscopic revolution. Arch Surg. 2008. 143:333–334.2. de la Fuente SG, Demaria EJ, Reynolds JD, Portenier DD, Pryor AD. New developments in surgery: Natural Orifice Transluminal Endoscopic Surgery (NOTES). Arch Surg. 2007. 142:295–297.3. Flora ED, Wilson TG, Martin IJ, O'Rourke NA, Maddern GJ. A review of natural orifice translumenal endoscopic surgery (NOTES) for intra-abdominal surgery: experimental models, techniques, and applicability to the clinical setting. Ann Surg. 2008. 247:583–602.
Article4. Bessler M, Stevens PD, Milone L, Parikh M, Fowler D. Transvaginal laparoscopically assisted endoscopic cholecystectomy: a hybrid approach to natural orifice surgery. Gastrointest Endosc. 2007. 66:1243–1245.
Article5. Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc. 2009. 23:1393–1397.
Article6. Reavis KM, Hinojosa MW, Smith BR, Nguyen NT. Single-laparoscopic incision transabdominal surgery sleeve gastrectomy. Obes Surg. 2008. 18:1492–1494.
Article7. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997. 84:695.
Article8. Podolsky ER, Curcillo PG 2nd. Single port access (SPA) surgery--a 24-month experience. J Gastrointest Surg. 2010. 14:759–767.
Article9. Omori T, Oyama T, Akamatsu H, Tori M, Ueshima S, Nishida T. Transumbilical single-incision laparoscopic distal gastrectomy for early gastric cancer. Surg Endosc. 2011. 25:2400–2404.
Article10. Lee YS, Kim JH, Moon EJ, Kim JJ, Lee KH, Oh SJ, et al. Comparative study on surgical outcomes and operative costs of transumbilical single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy in adult patients. Surg Laparosc Endosc Percutan Tech. 2009. 19:493–496.
Article11. Blay JY, Bonvalot S, Casali P, Choi H, Debiec-Richter M, Dei Tos AP, et al. GIST consensus meeting panelists. Consensus meeting for the management of gastrointestinal stromal tumors. Report of the GIST Consensus Conference of 20-21 March 2004, under the auspices of ESMO. Ann Oncol. 2005. 16:566–578.
Article12. Kinoshita K, Isozaki K, Tsutsui S, Kitamura S, Hiraoka S, Watabe K, et al. Endoscopic ultrasonography-guided fine needle aspiration biopsy in follow-up patients with gastrointestinal stromal tumours. Eur J Gastroenterol Hepatol. 2003. 15:1189–1193.
Article13. DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000. 231:51–58.14. Otani Y, Furukawa T, Yoshida M, Saikawa Y, Wada N, Ueda M, et al. Operative indications for relatively small (2-5 cm) gastrointestinal stromal tumor of the stomach based on analysis of 60 operated cases. Surgery. 2006. 139:484–492.
Article15. Huguet KL, Rush RM Jr, Tessier DJ, Schlinkert RT, Hinder RA, Grinberg GG, et al. Laparoscopic gastric gastrointestinal stromal tumor resection: the mayo clinic experience. Arch Surg. 2008. 143:587–590.
Article16. Sasaki A, Koeda K, Obuchi T, Nakajima J, Nishizuka S, Terashima M, et al. Tailored laparoscopic resection for suspected gastric gastrointestinal stromal tumors. Surgery. 2010. 147:516–520.
Article17. Ryu KJ, Jung SR, Choi JS, Jang YJ, Kim JH, Park SS, et al. Laparoscopic resection of small gastric submucosal tumors. Surg Endosc. 2011. 25:271–277.
Article18. Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw. 2010. 8:Suppl 2. S1–S41.
Article19. Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 2002. 131:S306–S311.
Article20. Santambrogio R, Montorsi M, Schubert L, Pisani Ceretti A, Costa M, Moroni E, et al. Laparoscopic ultrasound-guided resection of gastric submucosal tumors. Surg Endosc. 2006. 20:1305–1307.
Article21. Patrzyk M, Schreiber A, Heidecke CD, Glitsch A. Laser-supported diaphanoscopy: an innovative technique for locating gastric stromal tumors in gastroscopic-laparoscopic rendezvous: a case series. Endoscopy. 2009. 41:1090–1094.
Article22. Hiki N, Yamamoto Y, Fukunaga T, Yamaguchi T, Nunobe S, Tokunaga M, et al. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc. 2008. 22:1729–1735.
Article23. Tanabe K, Urabe Y, Tokumoto N, Suzuki T, Yamamoto H, Oka S, et al. A new method for intraluminal gastrointestinal stromal tumor resection using laparoscopic seromuscular dissection technique. Dig Surg. 2010. 27:461–465.
Article24. Stolzenburg JU, Kallidonis P, Oh MA, Ghulam N, Do M, Haefner T, et al. Comparative assessment of laparoscopic single-site surgery instruments to conventional laparoscopic in laboratory setting. J Endourol. 2010. 24:239–245.
Article25. Ragupathi M, Nieto J, Haas EM. Pearls and pitfalls in SILS colectomy. Surg Laparosc Endosc Percutan Tech. 2012. 22:183–188.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Single Port Laparoscopic Gastric Wedge Resection: Case Reports
- The Single Incision Laparoscopic Intragastric Wedge Resection of Gastric Submucosal Tumor
- Factors Associated with Operation Time of Laparoscopic Wedge Resection for Gastric Submucosal Tumors
- Laparoscopic Gastric Wedge Resection and Prophylactic Antireflux Surgery for a Submucosal Tumor of Gastroesophageal Junction
- Choice of LECS Procedure for Benign and Malignant Gastric Tumors