J Gastric Cancer.
2011 Dec;11(4):212-218.
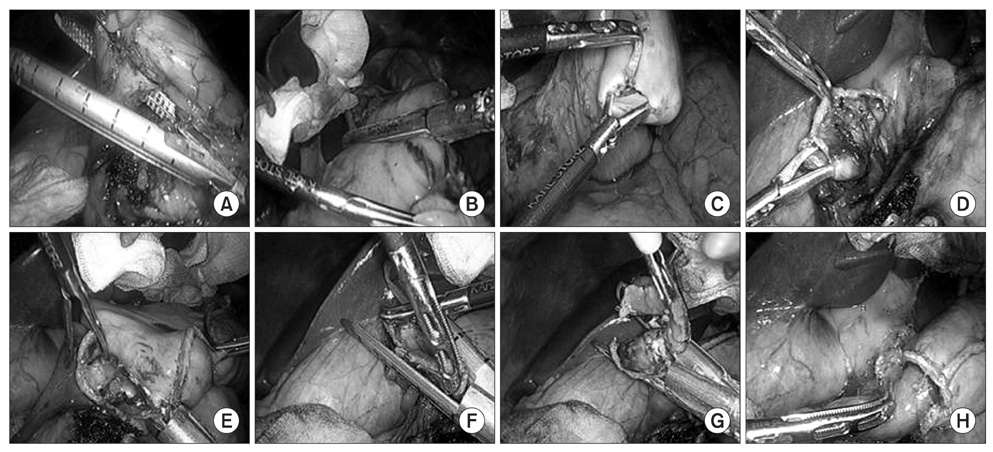
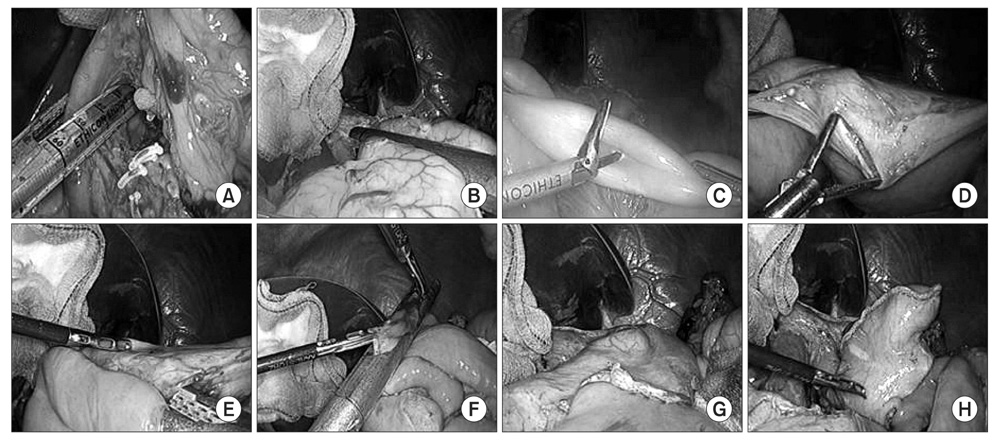
Intracorporeal Anastomosis Using Linear Stapler in Laparoscopic Distal Gastrectomy: Comparison between Gastroduodenostomy and Gastrojejunostomy
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. wjhyung@yuhs.ac
- 2Robot and MIS Center, Yonsei University College of Medicine, Seoul, Korea.
- 3Brain Korea 21 Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
Intracorporeal anastomosis during laparoscopic gastrectomy is becoming increasingly prevalent. However, selection of the anastomosis method after laparoscopic distal gastrectomy is equivocal because of a lack of technical feasibility and safety. We compared intracorporeal gastroduodenostomy with gastrojejunostomy using linear staplers to evaluate the technical feasibility and safety of intracorporeal anastomoses as well as its' minimally invasiveness.
MATERIALS AND METHODS
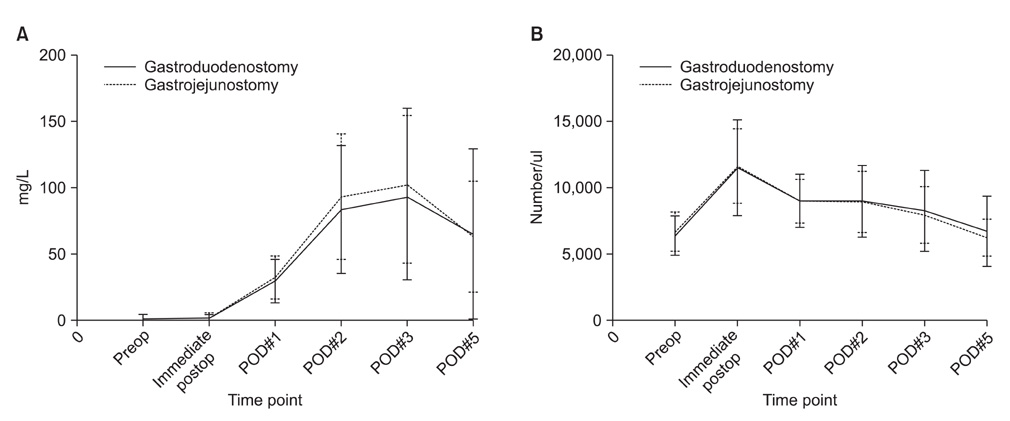
Retrospective analyses of a prospectively collected database for gastric cancer revealed 47 gastric cancer patients who underwent laparoscopic distal gastrectomy with either intracorporeal gastroduodenostomy or gastrojejunostomy from March 2011 to June 2011. Perioperative outcomes such as operation time, postoperative complication, and hospital stay were compared according to the type of anastomosis. Postoperative inflammatory response was also compared between the two groups using white blood cell count and high sensitivity C-reactive protein.
RESULTS
Among the 47 patients, 26 patients received gastroduodenostomy, whereas 21 patients received gastrojejunostomy without open conversion or additional mini-laparotomy incision. There was no difference in mean operation time, blood loss, and length of postoperative hospital stays. There was no statistically significant difference in postoperative complication or mortality between two groups. However, significantly more staplers were used for gastroduodenostomy than for gastrojejunostomy (n=6) than for gastroduodenostomy and (n=5).
CONCLUSIONS
Intracorporeal anastomosis during laparoscopic gastrectomy using linear stapler, either gastroduodenostomy or gastrojejunostomy, shows comparable and acceptable early postoperative outcomes and are safe and feasible. Therefore, surgeons may choose either anastomosis method as long as oncological safety is guaranteed.
MeSH Terms
Figure
Reference
-
1. Jeong O, Park YK. Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer. 2011. 11:69–77.
Article2. Hyung WJ, Kim SS, Choi WH, Cheong JH, Choi SH, Kim CB, et al. Changes in treatment outcomes of gastric cancer surgery over 45 years at a single institution. Yonsei Med J. 2008. 49:409–415.
Article3. Song KY, Park CH, Kang HC, Kim JJ, Park SM, Jun KH, et al. Is totally laparoscopic gastrectomy less invasive than laparoscopy-assisted gastrectomy?: prospective, multicenter study. J Gastrointest Surg. 2008. 12:1015–1021.
Article4. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg. 2002. 195:284–287.
Article5. Kanaya S, Kawamura Y, Kawada H, Iwasaki H, Gomi T, Satoh S, et al. The delta-shaped anastomosis in laparoscopic distal gastrectomy: analysis of the initial 100 consecutive procedures of intracorporeal gastroduodenostomy. Gastric Cancer. 2011. 14:365–371.
Article6. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma - 2nd English edition -. Gastric Cancer. 1998. 1:10–24.7. Hyung WJ, Song C, Cheong JH, Choi SH, Noh SH. Factors influencing operation time of laparoscopy-assisted distal subtotal gastrectomy: analysis of consecutive 100 initial cases. Eur J Surg Oncol. 2007. 33:314–319.
Article8. Kim HI, Hyung WJ, Lee CR, Lim JS, An JY, Cheong JH, et al. Intraoperative portable abdominal radiograph for tumor localization: a simple and accurate method for laparoscopic gastrectomy. Surg Endosc. 2011. 25:958–963.
Article9. Lee SW, Bouras G, Nomura E, Yoshinaka R, Tokuhara T, Nitta T, et al. Intracorporeal stapled anastomosis following laparoscopic segmental gastrectomy for gastric cancer: technical report and surgical outcomes. Surg Endosc. 2010. 24:1774–1780.
Article10. Hyung WJ, Lim JS, Cheong JH, Kim J, Choi SH, Song SY, et al. Intraoperative tumor localization using laparoscopic ultrasonography in laparoscopic-assisted gastrectomy. Surg Endosc. 2005. 19:1353–1357.
Article11. Lee HJ, Kim HH, Kim MC, Ryu SY, Kim W, Song KY, et al. Korean Laparoscopic Gastrointestinal Surgery Study Group. The impact of a high body mass index on laparoscopy assisted gastrectomy for gastric cancer. Surg Endosc. 2009. 23:2473–2479.
Article12. Song KY, Kim SN, Park CH. Laparoscopy-assisted distal gastrectomy with D2 lymph node dissection for gastric cancer: technical and oncologic aspects. Surg Endosc. 2008. 22:655–659.
Article13. Park DJ, Lee HJ, Kim HH, Yang HK, Lee KU, Choe KJ. Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg. 2005. 92:1099–1102.
Article14. Sah BK, Chen MM, Yan M, Zhu ZG. Gastric cancer surgery: Billroth I or Billroth II for distal gastrectomy? BMC Cancer. 2009. 9:428.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Linear-Shaped Gastroduodenostomy in Totally Laparoscopic Distal Gastrectomy
- Modified intracorporeal gastroduodenostomy in totally laparoscopic distal gastrectomy for gastric cancer: early experience
- Pledget as a Useful Substitute for a Knot in Intracorporeal Continuous Gastrointestinal Suturing
- Totally Laparoscopic Roux-en-Y Gastrojejunostomy after Laparoscopic Distal Gastrectomy: Analysis of Initial 50 Consecutive Cases of Single Surgeon in Comparison with Totally Laparoscopic Billroth I Reconstruction