Ann Surg Treat Res.
2015 Dec;89(6):306-312. 10.4174/astr.2015.89.6.306.
Modified intracorporeal gastroduodenostomy in totally laparoscopic distal gastrectomy for gastric cancer: early experience
- Affiliations
-
- 1Department of Surgery, Chungnam National University Hospital, Daejeon, Korea. mr231@cnu.ac.kr
- KMID: 2148305
- DOI: http://doi.org/10.4174/astr.2015.89.6.306
Abstract
- PURPOSE
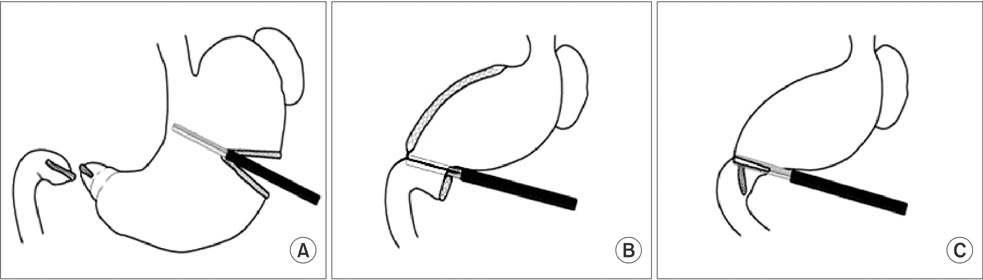
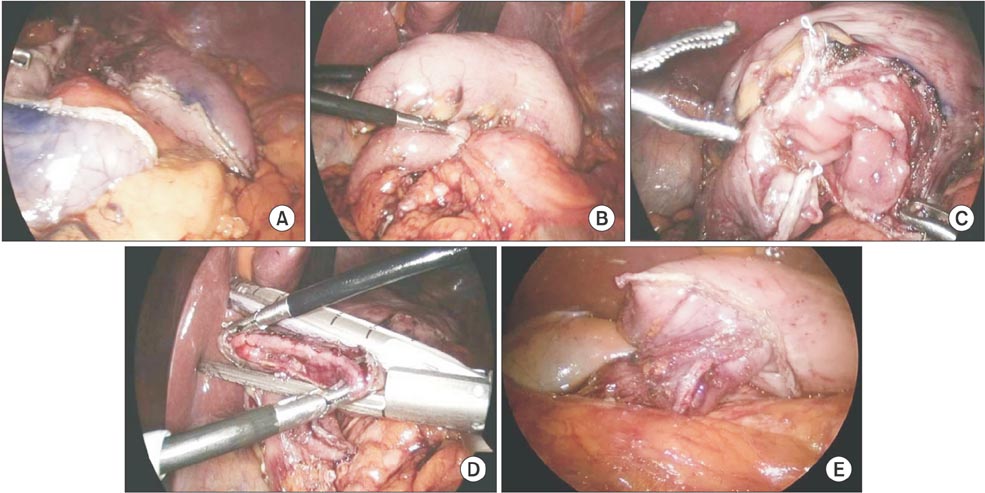
This study presents findings on the clinical usefulness of an overlap method that is another modification for the currently well-known intracorporeal gastroduodenostomy in totally laparoscopic distal gastrectomy (TLDG).
METHODS
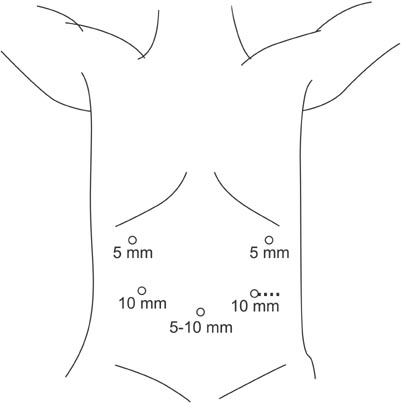
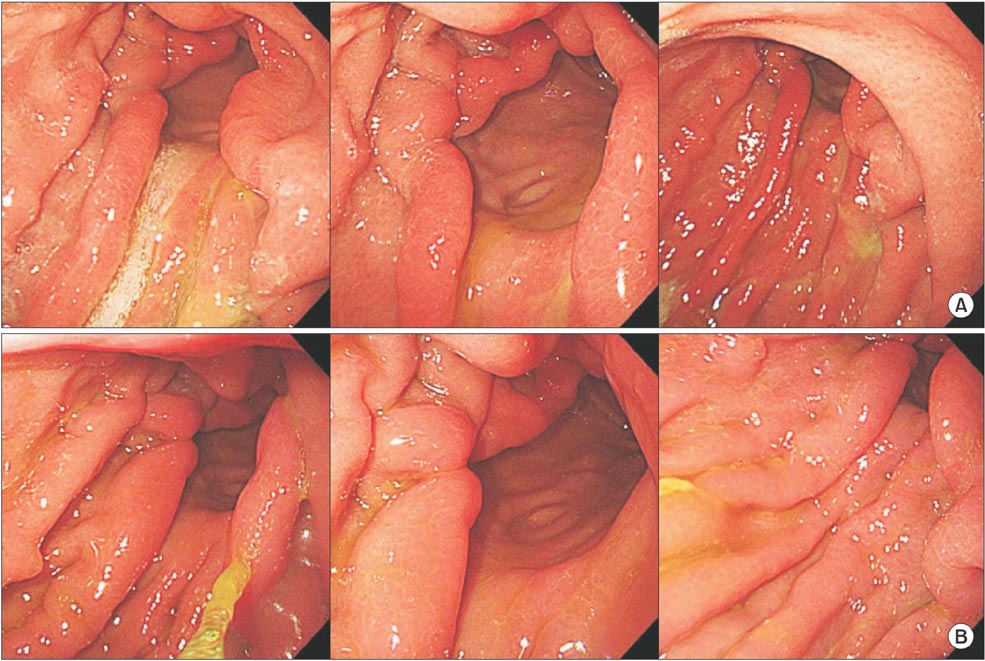
We studied 42 patients diagnosed with gastric cancer who underwent TLDG between December 2011 and March 2013. Endoscopic linear staplers were used for intracorporeal anastomosis and patients were observed with endoscopic tracking six months after surgery. We retrospectively reviewed the outcome of the operation, the clinical pathological results, and the endoscopy results.
RESULTS
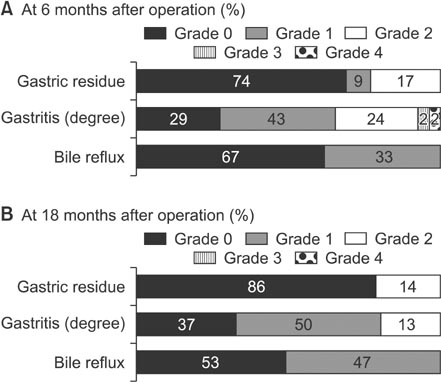
The mean duration of the operation for 42 patients was 228.3 +/- 42.5 minutes and the mean time to complete the anastomosis was 12.18 +/- 2.3 minutes. There were no mortalities and no cases of open conversion. Following the operation, 37 patients had stage IA, 5 in stage IB, and 3 in stage II gastric cancer. Abscesses were seen in 3 patients and 5 cases of stasis during the postoperative period. Duodenoscopy 6 months after the operation showed 11 cases of gastric stasis, 28 cases of bile reflux, and 1 new case of erosive gastritis. We did not observe contraction in any of the patients.
CONCLUSION
The overlap method for intracorporeal gastroduodenostomy, using an endoscopic linear stapler, can be considered a feasible and safe technique for the treatment of stomach cancer. However, a long-term comparative study is required to sufficiently evaluate our findings.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Modified Book Binding Technique (MBBT) for Intracorporeal Gastroduodenostomy in Totally Laparoscopic Distal Gastrectomy: Initial Experience
Jin Sung Kim, Eun Young Park, Dong Jin Park, Gyu Yeol Kim
J Gastric Cancer. 2019;19(3):355-364. doi: 10.5230/jgc.2019.19.e30.
Reference
-
1. Kim JJ, Song KY, Chin HM, Kim W, Jeon HM, Park CH, et al. Totally laparoscopic gastrectomy with various types of intracorporeal anastomosis using laparoscopic linear staplers: preliminary experience. Surg Endosc. 2008; 22:436–442.2. Song KY, Park CH, Kang HC, Kim JJ, Park SM, Jun KH, et al. Is totally laparoscopic gastrectomy less invasive than laparoscopy-assisted gastrectomy?: prospective, multicenter study. J Gastrointest Surg. 2008; 12:1015–1021.3. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg. 2002; 195:284–287.4. Hosono S, Arimoto Y, Ohtani H, Kanamiya Y. Meta-analysis of short-term outcomes after laparoscopy-assisted distal gastrectomy. World J Gastroenterol. 2006; 12:7676–7683.5. Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N. Japanese Laparoscopic Surgery Study Group.A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007; 245:68–72.6. Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N, Taomoto J, Masuda T, et al. Advantages of totally laparoscopic distal gastrectomy over laparoscopically assisted distal gastrectomy for gastric cancer. Surg Endosc. 2009; 23:2374–2379.7. Kim MG, Kawada H, Kim BS, Kim TH, Kim KC, Yook JH, et al. A totally laparoscopic distal gastrectomy with gastroduodenostomy (TLDG) for improvement of the early surgical outcomes in high BMI patients. Surg Endosc. 2011; 25:1076–1082.8. Kinoshita T, Shibasaki H, Oshiro T, Ooshiro M, Okazumi S, Katoh R. Comparison of laparoscopy-assisted and total laparoscopic Billroth-I gastrectomy for gastric cancer: a report of short-term outcomes. Surg Endosc. 2011; 25:1395–1401.9. Shehzad K, Mohiuddin K, Nizami S, Sharma H, Khan IM, Memon B, et al. Current status of minimal access surgery for gastric cancer. Surg Oncol. 2007; 16:85–98.10. Song HM, Lee SL, Hur H, Cho YK, Han SU. Linear-shaped gastroduodenostomy in totally laparoscopic distal gastrectomy. J Gastric Cancer. 2010; 10:69–74.11. Kanaya S, Kawamura Y, Kawada H, Iwasaki H, Gomi T, Satoh S, et al. The delta-shaped anastomosis in laparoscopic distal gastrectomy: analysis of the initial 100 consecutive procedures of intracorporeal gastroduodenostomy. Gastric Cancer. 2011; 14:365–371.12. Kim JJ, Kim SK, Jun KH, Kang HC, Song KY, Chin HM, et al. Clinical usefulness of a totally laparoscopic gastrectomy. J Korean Gastric Cancer Assoc. 2007; 7:132–138.13. Hosogi H, Kanaya S. Intracorporeal anastomosis in laparoscopic gastric cancer surgery. J Gastric Cancer. 2012; 12:133–139.14. Park SK, Lee HH, Kim JJ, Park SM. Delta-shaped gastroduodenostomy after totally laparoscopic distal gastrectomy: a comparison analysis between early and late experience. J Korean Surg Soc. 2010; 79:110–115.15. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.16. Kubo M, Sasako M, Gotoda T, Ono H, Fujishiro M, Saito D, et al. Endoscopic evaluation of the remnant stomach after gastrectomy: proposal for a new classification. Gastric Cancer. 2002; 5:83–89.17. Chen K, Mou YP, Xu XW, Cai JQ, Wu D, Pan Y, et al. Short-term surgical and long-term survival outcomes after laparoscopic distal gastrectomy with D2 lymphadenectomy for gastric cancer. BMC Gastroenterol. 2014; 14:41.18. Kitagami H, Morimoto M, Nozawa M, Nakamura K, Tanimura S, Murakawa K, et al. Evaluation of the delta-shaped anastomosis in laparoscopic distal gastrectomy: midterm results of a comparison with Roux-en-Y anastomosis. Surg Endosc. 2014; 28:2137–2144.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- The Early Experience with a Totally Laparoscopic Distal Gastrectomy
- Modified Book Binding Technique (MBBT) for Intracorporeal Gastroduodenostomy in Totally Laparoscopic Distal Gastrectomy: Initial Experience
- Linear-Shaped Gastroduodenostomy in Totally Laparoscopic Distal Gastrectomy
- Intracorporeal Anastomosis Using Linear Stapler in Laparoscopic Distal Gastrectomy: Comparison between Gastroduodenostomy and Gastrojejunostomy