J Gastric Cancer.
2015 Sep;15(3):191-200. 10.5230/jgc.2015.15.3.191.
Clinical Outcome of Modified Laparoscopy-Assisted Proximal Gastrectomy Compared to Conventional Proximal Gastrectomy or Total Gastrectomy for Upper-Third Early Gastric Cancer with Special References to Postoperative Reflux Esophagitis
- Affiliations
-
- 1Department of Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. appe98@snu.ac.kr
- 2Cancer Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Surgery, Myongji Hospital, Goyang, Korea.
- 4Department of Surgery, Gachon University Gil Medical Center, Incheon, Korea.
- 5Department of Surgery, Seoul National University Boramae Medical Center, Seoul, Korea.
- KMID: 2372205
- DOI: http://doi.org/10.5230/jgc.2015.15.3.191
Abstract
- PURPOSE
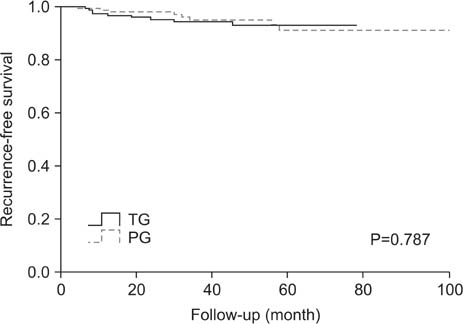
This study evaluated the functional and oncological outcomes of proximal gastrectomy (PG) in comparison with total gastrectomy (TG) for upper-third early gastric cancer (EGC).
MATERIALS AND METHODS
The medical records of upper-third EGC patients who had undergone PG (n=192) or TG (n=157) were reviewed. The PG group was further subdivided into patients who had undergone conventional open PG (cPG; n=157) or modified laparoscopy-assisted PG (mLAPG; n=35). Patients who had undergone mLAPG had a longer portion of their intra-abdominal esophagus preserved than patients who had undergone cPG. Surgical morbidity, recurrence, long-term nutritional status, and the incidence of reflux esophagitis were compared between the groups.
RESULTS
The rate of postoperative complications was significantly lower for PG than TG (16.7% vs. 31.2%), but the five-year overall survival rate was comparable between the two groups (99.3% vs. 96.3%). Postoperative levels of hemoglobin and albumin were significantly higher for patients who had undergone PG. However, the incidence of reflux esophagitis was higher for PG than for TG (37.4% vs. 3.7%; P<0.001). mLAPG was related to a lower incidence of reflux esophagitis after PG (P<0.001).
CONCLUSIONS
Compared to TG, PG showed an advantage in terms of postoperative morbidity and nutrition, and there was a comparable prognosis between the two procedures. Preserving the intra-abdominal esophagus may lower the incidence of reflux esophagitis associated with PG.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Korean Practice Guideline for Gastric Cancer 2018: an Evidence-based, Multi-disciplinary Approach
J Gastric Cancer. 2019;19(1):1-48. doi: 10.5230/jgc.2019.19.e8.Spade-Shaped Anastomosis Following a Proximal Gastrectomy Using a Double Suture to Fix the Posterior Esophageal Wall to the Anterior Gastric Wall (SPADE Operation): Case-Control Study of Early Outcomes
Won Ho Han, Bang Wool Eom, Hong Man Yoon, Junsun Ryu, Young-Woo Kim
J Gastric Cancer. 2020;20(1):72-80. doi: 10.5230/jgc.2020.20.e5.
Reference
-
1. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.2. Harrison LE, Karpeh MS, Brennan MF. Total gastrectomy is not necessary for proximal gastric cancer. Surgery. 1998; 123:127–130.3. Katsoulis IE, Robotis JF, Kouraklis G, Yannopoulos PA. What is the difference between proximal and total gastrectomy regarding postoperative bile reflux into the oesophagus? Dig Surg. 2006; 23:325–330.4. Ahn HS, Lee HJ, Yoo MW, Jeong SH, Park DJ, Kim HH, et al. Changes in clinicopathological features and survival after gastrectomy for gastric cancer over a 20-year period. Br J Surg. 2011; 98:255–260.5. Hirai T, Matsumoto H, Iki K, Hirabayashi Y, Kawabe Y, Ikeda M, et al. Lower esophageal sphincter- and vagus-preserving proximal partial gastrectomy for early cancer of the gastric cardia. Surg Today. 2006; 36:874–878.6. Kim DJ, Lee JH, Kim W. Lower esophageal sphincter-preserving laparoscopy-assisted proximal gastrectomy in patients with early gastric cancer: a method for the prevention of reflux esophagitis. Gastric Cancer. 2013; 16:440–444.7. Armstrong D, Bennett JR, Blum AL, Dent J, De Dombal FT, Galmiche JP, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996; 111:85–92.8. An JY, Youn HG, Choi MG, Noh JH, Sohn TS, Kim S. The difficult choice between total and proximal gastrectomy in proximal early gastric cancer. Am J Surg. 2008; 196:587–591.9. Katai H, Sano T, Fukagawa T, Shinohara H, Sasako M. Prospective study of proximal gastrectomy for early gastric cancer in the upper third of the stomach. Br J Surg. 2003; 90:850–853.10. Shiraishi N, Adachi Y, Kitano S, Kakisako K, Inomata M, Yasuda K. Clinical outcome of proximal versus total gastrectomy for proximal gastric cancer. World J Surg. 2002; 26:1150–1154.11. Imada T, Rino Y, Takahashi M, Suzuki M, Tanaka J, Shiozawa M, et al. Postoperative functional evaluation of pylorus-preserving gastrectomy for early gastric cancer compared with conventional distal gastrectomy. Surgery. 1998; 123:165–170.12. Park DJ, Lee HJ, Jung HC, Kim WH, Lee KU, Yang HK. Clinical outcome of pylorus-preserving gastrectomy in gastric cancer in comparison with conventional distal gastrectomy with Billroth I anastomosis. World J Surg. 2008; 32:1029–1036.13. Katai H, Sano T, Fukagawa T, Shinohara H, Sasako M. Prospective study of proximal gastrectomy for early gastric cancer in the upper third of the stomach. Br J Surg. 2003; 90:850–853.14. Uyama I, Sugioka A, Fujita J, Komori Y, Matsui H, Hasumi A. Completely laparoscopic proximal gastrectomy with jejunal interposition and lymphadenectomy. J Am Coll Surg. 2000; 191:114–119.15. Kinoshita T, Gotohda N, Kato Y, Takahashi S, Konishi M, Kinoshita T. Laparoscopic proximal gastrectomy with jejunal interposition for gastric cancer in the proximal third of the stomach: a retrospective comparison with open surgery. Surg Endosc. 2013; 27:146–153.16. Lim HJ, Jeong YJ, Yang DH. A comparative study on the outcomes of total and proximal gastrectomies performed for gastric cancer. Korean J Gastroenterol. 2002; 40:364–370.17. Pierie JP, de Graaf PW, Poen H, van der Tweel I, Obertop H. Incidence and management of benign anastomotic stricture after cervical oesophagogastrostomy. Br J Surg. 1993; 80:471–474.18. Shemesh E, Czerniak A. Comparison between Savary-Gilliard and balloon dilatation of benign esophageal strictures. World J Surg. 1990; 14:518–521. discussion 521-52219. Brandimarte G, Tursi A. Endoscopic treatment of benign anastomotic esophageal stenosis with electrocautery. Endoscopy. 2002; 34:399–401.20. Hordijk ML, Siersema PD, Tilanus HW, Kuipers EJ. Electrocautery therapy for refractory anastomotic strictures of the esophagus. Gastrointest Endosc. 2006; 63:157–163.21. Bae JM, Park JW, Kim JP. Nutritional assessment and intestinal absorption studies on total gastrectomized gastric cancer patients. J Korean Surg Soc. 1996; 50:475–487.22. Cho SJ, Jegal YJ. Nutritional status, and mucosal morphology of jejunum after total gastrectomy for carcinoma of the stomach. J Korean Surg Soc. 1990; 39:726–734.23. Kim JW, Yoon H, Kong SH, Kim JS, Paeng JC, Lee HJ, et al. Analysis of esophageal reflux after proximal gastrectomy measured by wireless ambulatory 24-hr esophageal pH monitoring and TC-99m diisopropyliminodiacetic acid (DISIDA) scan. J Surg Oncol. 2010; 101:626–633.24. Sakuramoto S, Yamashita K, Kikuchi S, Futawatari N, Katada N, Moriya H, et al. Clinical experience of laparoscopy-assisted proximal gastrectomy with Toupet-like partial fundoplication in early gastric cancer for preventing reflux esophagitis. J Am Coll Surg. 2009; 209:344–351.25. Ichikawa D, Komatsu S, Okamoto K, Shiozaki A, Fujiwara H, Otsuji E. Evaluation of symptoms related to reflux esophagitis in patients with esophagogastrostomy after proximal gastrectomy. Langenbecks Arch Surg. 2013; 398:697–701.26. Nakamura M, Nakamori M, Ojima T, Katsuda M, Iida T, Hayata K, et al. Reconstruction after proximal gastrectomy for early gastric cancer in the upper third of the stomach: an analysis of our 13-year experience. Surgery. 2014; 156:57–63.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Single-Port Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction for Early Gastric Cancer: Report of a Case
- Laparoscopic Proximal Gastrectomy as a Surgical Treatment for Upper Third Early Gastric Cancer
- The Risk Factors of Reflux Complication after Gastrectomy for Proximal Gastric Cancer
- Long-term Results of Proximal and Total Gastrectomy for Adenocarcinoma of the Upper Third of the Stomach
- Non-Randomized Confirmatory Trial of Laparoscopy-Assisted Total Gastrectomy and Proximal Gastrectomy with Nodal Dissection for Clinical Stage I Gastric Cancer: Japan Clinical Oncology Group Study JCOG1401