J Gastric Cancer.
2014 Mar;14(1):15-22.
The Impact of Esophageal Reflux-Induced Symptoms on Quality of Life after Gastrectomy in Patients with Gastric Cancer
- Affiliations
-
- 1Gangnam Severance Cancer Hospital, Seoul, Korea.
- 2Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. choish@yuhs.ac
- 3Division of Gastroenterology, Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
To evaluate the prevalence of esophageal reflux-induced symptoms after gastrectomy owing to gastric cancer and assess the relationship between esophageal reflux-induced symptoms and quality of life.
MATERIALS AND METHODS
From January 2012 to May 2012, 332 patients were enrolled in this cross-sectional study. The patients had a history of curative resection for gastric cancer at least 6 months previously without recurrence, other malignancy, or ongoing chemotherapy. Esophageal reflux-induced symptoms were evaluated with the GerdQ questionnaire. The quality of life was evaluated with the European Organization for Research and Treatment QLQ-C30 and STO22 questionnaires.
RESULTS
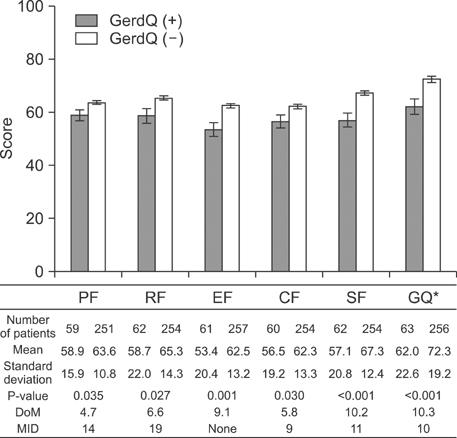
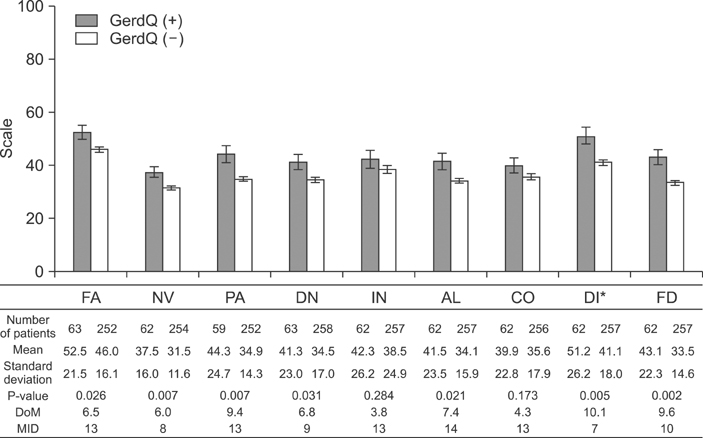
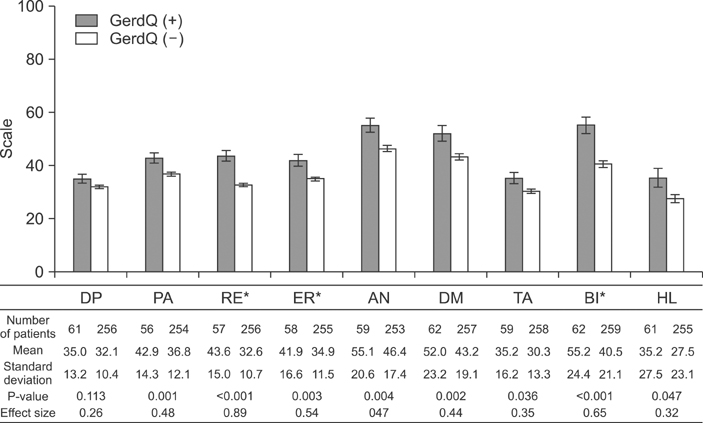
Of the 332 patients, 275 had undergone subtotal gastrectomy and 57 had undergone total gastrectomy. The number of GerdQ(+) patients was 58 (21.1%) after subtotal gastrectomy, and 7 (12.3%) after total gastrectomy (P=0.127). GerdQ(+) patients showed significantly worse scores compared to those for GerdQ(-) patients in nearly all functional and symptom QLQ-C30 scales, with the difference in the mean score of global health status/quality of life and diarrhea symptoms being higher than in the minimal important difference. Additionally, in the QLQ STO22, GerdQ(+) patients had significantly worse scores in every symptom scale. The GerdQ score was negatively correlated with the global quality of life score (r=-0.170, P=0.002).
CONCLUSIONS
Esophageal reflux-induced symptoms may develop at a similar rate or more frequently after subtotal gastrectomy compared to that after total gastrectomy, and decrease quality of life in gastric cancer patients. To improve quality of life after gastrectomy, new strategies are required to prevent or reduce esophageal reflux.
MeSH Terms
Figure
Reference
-
1. Guggenheim DE, Shah MA. Gastric cancer epidemiology and risk factors. J Surg Oncol. 2013; 107:230–236.
Article2. Conroy T, Marchal F, Blazeby JM. Quality of life in patients with oesophageal and gastric cancer: an overview. Oncology. 2006; 70:391–402.
Article3. Gisbert JP, Cooper A, Karagiannis D, Hatlebakk J, Agréus L, Jablonowski H, et al. Impact of gastroesophageal reflux disease on patients' daily lives: a European observational study in the primary care setting. Health Qual Life Outcomes. 2009; 7:60.
Article4. Toghanian S, Wahlqvist P, Johnson DA, Bolge SC, Liljas B. The burden of disrupting gastro-oesophageal reflux disease: a database study in US and European cohorts. Clin Drug Investig. 2010; 30:167–178.5. Inokuchi M, Kojima K, Yamada H, Kato K, Hayashi M, Motoyama K, et al. Long-term outcomes of Roux-en-Y and Billroth-I reconstruction after laparoscopic distal gastrectomy. Gastric Cancer. 2013; 16:67–73.
Article6. Nunobe S, Okaro A, Sasako M, Saka M, Fukagawa T, Katai H, et al. Billroth 1 versus Roux-en-Y reconstructions: a quality-of-life survey at 5 years. Int J Clin Oncol. 2007; 12:433–439.
Article7. Lee MS, Ahn SH, Lee JH, Park do J, Lee HJ, Kim HH, et al. What is the best reconstruction method after distal gastrectomy for gastric cancer? Surg Endosc. 2012; 26:1539–1547.
Article8. Matei D, Dadu R, Prundus R, Danci I, Ciobanu L, Mocan T, et al. Alkaline reflux esophagitis in patients with total gastrectomy and Roux en Y esojejunostomy. J Gastrointestin Liver Dis. 2010; 19:247–252.9. Kim JW, Yoon H, Kong SH, Kim JS, Paeng JC, Lee HJ, et al. Analysis of esophageal reflux after proximal gastrectomy measured by wireless ambulatory 24-hr esophageal pH monitoring and TC-99m diisopropyliminodiacetic acid (DISIDA) scan. J Surg Oncol. 2010; 101:626–633.
Article10. Enjoji M, Yamada H, Kojima K, Inokuchi M, Kato K, Kawano T, et al. Scoring system for evaluating functional disorders following laparoscopy-assisted distal gastrectomy. J Surg Res. 2010; 164:e229–e233.
Article11. Kim JH, Park H, Lee YC. MIGHT study group. Is minimal change esophagitis really part of the spectrum of endoscopic findings of gastroesophageal reflux disease? A prospective, multicenter study. Endoscopy. 2011; 43:190–195.
Article12. Shaw MJ, Talley NJ, Beebe TJ, Rockwood T, Carlsson R, Adlis S, et al. Initial validation of a diagnostic questionnaire for gastroesophageal reflux disease. Am J Gastroenterol. 2001; 96:52–57.
Article13. Jones R, Coyne K, Wiklund I. The gastro-oesophageal reflux disease impact scale: a patient management tool for primary care. Aliment Pharmacol Ther. 2007; 25:1451–1459.
Article14. Revicki DA, Wood M, Wiklund I, Crawley J. Reliability and validity of the Gastrointestinal Symptom Rating Scale in patients with gastroesophageal reflux disease. Qual Life Res. 1998; 7:75–83.15. Jones R, Junghard O, Dent J, Vakil N, Halling K, Wernersson B, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther. 2009; 30:1030–1038.
Article16. Ponce J, Garrigues V, Agréus L, Tabaglio E, Gschwantler M, Guallar E, et al. Structured management strategy based on the Gastro-oesophageal Reflux Disease (GERD) Questionnaire (GerdQ) vs. usual primary care for GERD: pooled analysis of five cluster-randomised European studies. Int J Clin Pract. 2012; 66:897–905.
Article17. Dent J, Vakil N, Jones R, Bytzer P, Schöning U, Halling K, et al. Accuracy of the diagnosis of GORD by questionnaire, physicians and a trial of proton pump inhibitor treatment: the Diamond Study. Gut. 2010; 59:714–721.
Article18. Huang CC, Lien HH, Sung YC, Liu HT, Chie WC. Quality of life of patients with gastric cancer in Taiwan: validation and clinical application of the Taiwan Chinese version of the EORTC QLQ-C30 and EORTC QLQ-STO22. Psychooncology. 2007; 16:945–949.
Article19. Shaw M, Dent J, Beebe T, Junghard O, Wiklund I, Lind T, et al. The Reflux Disease Questionnaire: a measure for assessment of treatment response in clinical trials. Health Qual Life Outcomes. 2008; 6:31.
Article20. Blazeby JM, Conroy T, Bottomley A, Vickery C, Arraras J, Sezer O, et al. European Organisation for Research and Treatment of Cancer Gastrointestinal and Quality of Life Groups. Clinical and psychometric validation of a questionnaire module, the EORTC QLQ-STO 22, to assess quality of life in patients with gastric cancer. Eur J Cancer. 2004; 40:2260–2268.
Article21. Blazeby JM, Currie E, Zee BC, Chie WC, Poon RT, Garden OJ. EORTC Quality of Life Group. Development of a questionnaire module to supplement the EORTC QLQ-C30 to assess quality of life in patients with hepatocellular carcinoma, the EORTC QLQ-HCC18. Eur J Cancer. 2004; 40:2439–2444.
Article22. Yun YH, Park YS, Lee ES, Bang SM, Heo DS, Park SY, et al. Validation of the Korean version of the EORTC QLQ-C30. Qual Life Res. 2004; 13:863–868.
Article23. Kong H, Kwon OK, Yu W. Changes of quality of life after gastric cancer surgery. J Gastric Cancer. 2012; 12:194–200.
Article24. Fayer PM, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A, et al. EORTC QLQ-C30 scoring manual. 3rd ed. Brussels: European Organisation for Research and Treatment of Cancer;2001.25. Cocks K, King MT, Velikova G, Martyn St-James M, Fayers PM, Brown JM. Evidence-based guidelines for determination of sample size and interpretation of the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. J Clin Oncol. 2011; 29:89–96.
Article26. King MT. A point of minimal important difference (MID): a critique of terminology and methods. Expert Rev Pharmacoecon Outcomes Res. 2011; 11:171–184.
Article27. Cohen J. Statistical power analysis for the behavioral sciences. New York: Academic Press;1977.28. Copay AG, Subach BR, Glassman SD, Polly DW Jr, Schuler TC. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J. 2007; 7:541–546.
Article29. Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005; 54:710–717.
Article30. El-Serag HB. Epidemiology of non-erosive reflux disease. Digestion. 2008; 78:Suppl 1. 6–10.
Article31. Lehnert T, Buhl K. Techniques of reconstruction after total gastrectomy for cancer. Br J Surg. 2004; 91:528–539.
Article32. Katsoulis IE, Robotis JF, Kouraklis G, Yannopoulos PA. What is the difference between proximal and total gastrectomy regarding postoperative bile reflux into the oesophagus? Dig Surg. 2006; 23:325–330.
Article33. Hsu CP, Chen CY, Hsieh YH, Hsia JY, Shai SE, Kao CH. Esophageal reflux after total or proximal gastrectomy in patients with adenocarcinoma of the gastric cardia. Am J Gastroenterol. 1997; 92:1347–1350.34. Tokunaga M, Hiki N, Ohyama S, Nunobe S, Miki A, Fukunaga T, et al. Effects of reconstruction methods on a patient's quality of life after a proximal gastrectomy: subjective symptoms evaluation using questionnaire survey. Langenbecks Arch Surg. 2009; 394:637–641.
Article35. Ichikawa D, Komatsu S, Okamoto K, Shiozaki A, Fujiwara H, Otsuji E. Evaluation of symptoms related to reflux esophagitis in patients with esophagogastrostomy after proximal gastrectomy. Langenbecks Arch Surg. 2013; 398:697–701.
Article36. Johnson DA, Fennerty MB. Heartburn severity underestimates erosive esophagitis severity in elderly patients with gastroesophageal reflux disease. Gastroenterology. 2004; 126:660–664.
Article37. Iida F, Ishizaka K, Sugenoya A. Lower esophageal sphincter pressure after subtotal gastrectomy and postoperative reflux esophagitis. Hepatogastroenterology. 1994; 41:581–584.38. Fujiwara Y, Nakao K, Inoue T, Koishi K, Nishio Y, Yagyu R, et al. Clinical significance of hiatal hernia in the development of gastroesophageal reflux after distal gastrectomy for cancer of the stomach. J Gastroenterol Hepatol. 2006; 21:1103–1107.
Article39. Crookes PF. Gastroesophageal reflux after partial gastrectomy. Am J Gastroenterol. 1998; 93:3–4.
Article40. Fujiwara Y, Nakagawa K, Kusunoki M, Tanaka T, Yamamura T, Utsunomiya J. Gastroesophageal reflux after distal gastrectomy: possible significance of the angle of His. Am J Gastroenterol. 1998; 93:11–15.
Article41. Windsor CW. Gastro-oesophageal reflux after partial gastrectomy. Br Med J. 1964; 2:1233–1234.
Article42. Gutschow C, Collard JM, Romagnoli R, Salizzoni M, Hölscher A. Denervated stomach as an esophageal substitute recovers intraluminal acidity with time. Ann Surg. 2001; 233:509–514.
Article43. Shibata Y. Effect of semifundoplication with subtotal gastrectomy for prevention of postoperative gastroesophageal reflux. J Am Coll Surg. 2004; 198:212–217.
Article44. Montesani C, D'Amato A, Santella S, Pronio A, Giovannini C, Cristaldi M, et al. Billroth I versus Billroth II versus Roux-en-Y after subtotal gastrectomy. Prospective [correction of prespective] randomized study. Hepatogastroenterology. 2002; 49:1469–1473.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Small Intestinal(gastro)esophageal Reflux in Different Types of Gastrectomy : 24 Hour Esophageal Bilirubin Monitoring
- A Comparative Study on the Outcomes of Total and Proximal Gastrectomies Performed for Gastric Cancer
- A Study of Esophageal Acidity and Motility Change after a Gastrectomy for Stomach Cancer
- The Risk Factors of Reflux Complication after Gastrectomy for Proximal Gastric Cancer
- Clinical Significance of a Pylorus-preserving Gastrectomy for Early Gastric Cancer