J Korean Soc Radiol.
2017 Mar;76(3):229-232. 10.3348/jksr.2017.76.3.229.
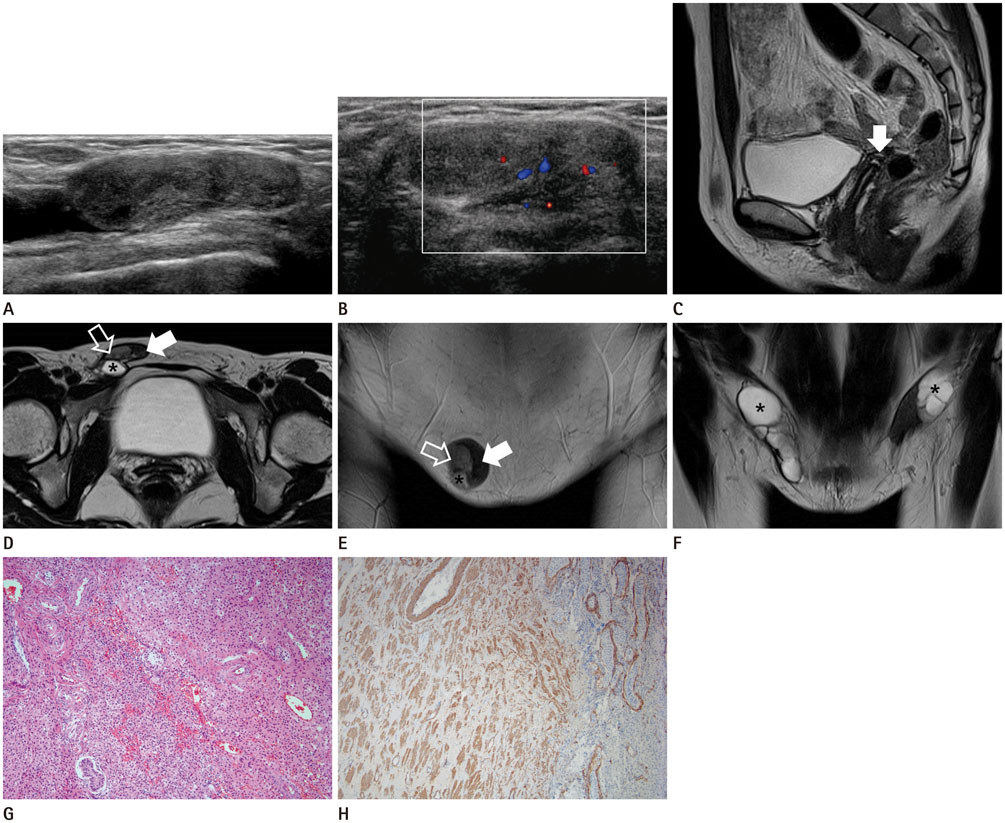
Complete Androgen Insensitivity Syndrome with Paratesticular Leiomyoma: A Case Report
- Affiliations
-
- 1Department of Radiology, Chosun University College of Medicine, Gwangju, Korea. panradiologist@gmail.com
- 2Departments of Pathology, Chosun University College of Medicine, Gwangju, Korea.
- 3Department of Urology, Chosun University College of Medicine, Gwangju, Korea.
- KMID: 2371691
- DOI: http://doi.org/10.3348/jksr.2017.76.3.229
Abstract
- Complete androgen insensitivity syndrome (AIS) is a rare, X-linked recessive disorder. Patients with AIS may develop primary amenorrhea due to androgen receptor resistance, resulting in a normal female phenotype and male (XY) karyotype. We report a case of a 30-year-old woman who was diagnosed with complete AIS. Ultrasonography and magnetic resonance imaging revealed bilateral inguinal cryptorchidism and no ovaries and uterus. After gonadectomy, the inguinal mass was confirmed as testicular atrophy with hamartomatous proliferation of Leydig cells and paratesticular leiomyoma. Although these tumors have been reported in association with AIS, this is the first case of paratesticular leiomyoma with hamartomatous proliferation of Leydig cells in atrophic testes being reported in Korea.
MeSH Terms
Figure
Reference
-
1. Hughes IA, Davies JD, Bunch TI, Pasterski V, Mastroyannopoulou K, MacDougall J. Androgen insensitivity syndrome. Lancet. 2012; 380:1419–1428.2. Khan S, Craig LB. A review of radiologic imaging in patients with androgen insensitivity. J Genit Syst Disord. 2013; S1. DOI: 10.4172/2325-9728.S1-003.3. Siminas S, Kokai G, Kenny SE. Complete androgen insensitivity syndrome associated with bilateral Sertoli cell adenomas and paratesticular leiomyomas: case report and review of the literature. J Pediatr Urol. 2013; 9:e31–e34.4. Sohaib SA, Cook G, Koh DM. Imaging studies for germ cell tumors. Hematol Oncol Clin North Am. 2011; 25:487–502, vii.5. Nezzo M, De Visschere P, T'sjoen G, Weyers S, Villeirs G. Role of imaging in the diagnosis and management of complete androgen insensitivity syndrome in adults. Case Rep Radiol. 2013; 2013:158484.6. Levin HS. Nonneoplastic diseases of the testis. In : Mills SE, Carter D, Greenson JK, Oberman HA, Reuter V, Stoler MH, editors. Sternberg's diagnostic surgical pathology. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2004. p. 2133–2166.7. Iwamoto I, Yanazume S, Fujino T, Yoshioka T, Douchi T. Leydig cell tumor in an elderly patient with complete androgen insensitivity syndrome. Gynecol Oncol. 2005; 96:870–872.8. Asl Zare M, Kalantari MR, Asadpour AA, Kamalati A. Bilateral laparoscopic gonadectomy in a patient with complete androgen insensitivity syndrome and bilateral sertoli-leydig cell tumor: a case report and brief review of the literature. Nephrourol Mon. 2014; 6:e15278.9. Krichen Makni S, Mnif Hachicha L, Ellouze S, Mnif M, Khabir A, Ketata H, et al. [Feminizing testicular syndrome with multiple hamartomas and bilateral paratesticular leiomyomas]. Rev Med Interne. 2005; 26:980–983.10. Tsili AC, Argyropoulou MI, Giannakis D, Sofikitis N, Tsampoulas K. MRI in the characterization and local staging of testicular neoplasms. AJR Am J Roentgenol. 2010; 194:682–689.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Laparoscopic Gonadectomy in Complete Androgen Insensitivity Syndrome
- A Case Report of Complete Androgen Insensitivity Syndrome
- A Case of Complete Androgen Insensitivity Syndrome with Bilateral Inguinal Gonads
- A case report of sisters with complete androgen insensitivity syndrome
- Pelviscopic Gonadectomy in two cases of Complete Androgen Insensitivity Syndrome