Ann Rehabil Med.
2016 Dec;40(6):998-1009. 10.5535/arm.2016.40.6.998.
Can Short-Term Constraint-Induced Movement Therapy Combined With Visual Biofeedback Training Improve Hemiplegic Upper Limb Function of Subacute Stroke Patients?
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. khd1516@naver.com
- 2Department of Rehabilitation Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea.
- KMID: 2371331
- DOI: http://doi.org/10.5535/arm.2016.40.6.998
Abstract
OBJECTIVE
To Investigate the synergic effects of short-term constraint-induced movement therapy (CIMT) and visual biofeedback training (VBT) in subacute stroke patients.
METHODS
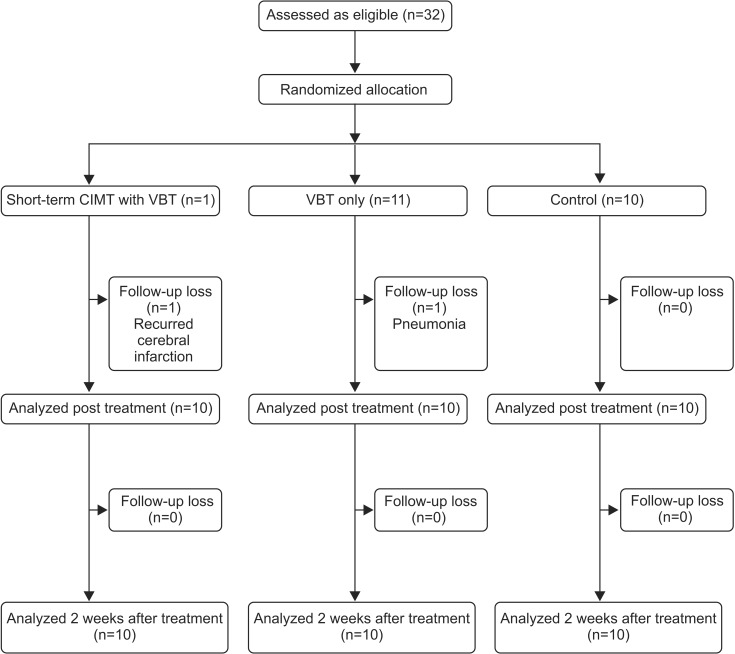
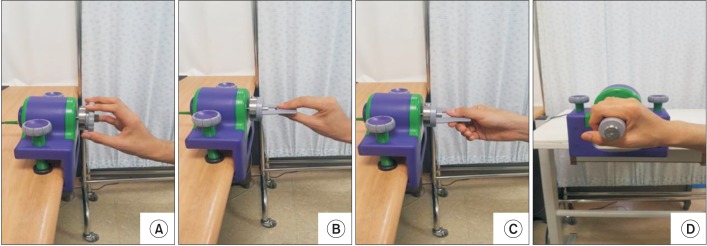
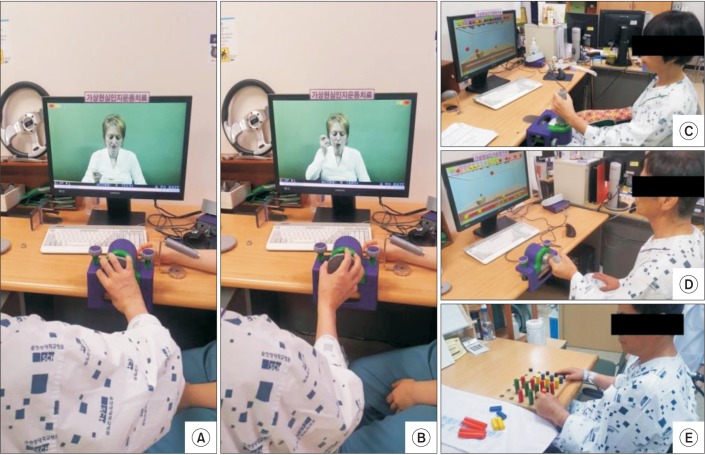
Thirty-two subacute stroke patients were enrolled and randomly assigned to one of three groups: short-term CIMT with VBT, VBT only, and control groups. We applied CIMT for an hour daily during VBT instead of the ordinary restraint time, referred to as 'short-term' CIMT. Short-term CIMT with VBT group received simultaneous VBT with CIMT, whereas the VBT the only group received VBT without CIMT for an hour a day for 2 weeks. The control group received conventional occupational therapy (OT) alone. Patients underwent the Purdue Pegboard Test, the JAMAR grip strength test, the Wolf Motor Function Test, the Fugl-Meyer Assessment (upper extremity), Motricity index and the Korean version of Modified Barthel Index test to evaluate motor functions of the hemiplegic upper limb at baseline, post-treatment, and 2 weeks after treatment.
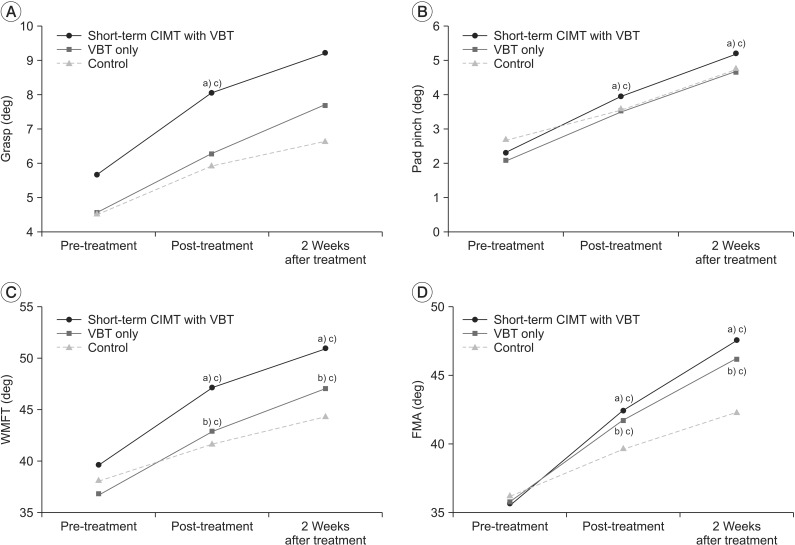
RESULTS
No significant differences were observed between short-term CIMT with VBT and VBT only groups. Both groups showed significantly higher scores compared to the control group in the WMFT and FMA tests. However, the short-term CIMT with VBT group showed significant improvement (p<0.05) compared with the control group in both grasp and pad pinch at post-treatment and 2 weeks after treatment while the VBT only group did not.
CONCLUSION
Short-term CIMT with VBT group did not show significant improvement of hemiplegic upper limb function of subacute stroke patients, compared to VBT only group. Larger sample sizes and different restraint times would be needed to clarify the effect.
MeSH Terms
Figure
Reference
-
1. Kwakkel G, Kollen BJ, van der Grond J, Prevo AJ. Probability of regaining dexterity in the flaccid upper limb: impact of severity of paresis and time since onset in acute stroke. Stroke. 2003; 34:2181–2186. PMID: 12907818.2. Wolf SL, Thompson PA, Winstein CJ, Miller JP, Blanton SR, Nichols-Larsen DS, et al. The EXCITE stroke trial: comparing early and delayed constraint-induced movement therapy. Stroke. 2010; 41:2309–2315. PMID: 20814005.3. Taub E, Miller NE, Novack TA, Cook EW 3rd, Fleming WC, Nepomuceno CS, et al. Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil. 1993; 74:347–354. PMID: 8466415.4. Sterr A, Freivogel S, Schmalohr D. Neurobehavioral aspects of recovery: assessment of the learned nonuse phenomenon in hemiparetic adolescents. Arch Phys Med Rehabil. 2002; 83:1726–1731. PMID: 12474177.
Article5. Morris DM, Crago JE, Deluca SC, Pidikiti RD, Taub E. Constraint-induced movement therapy for moter recovery after stroke. NeuroRehabilitation. 1997; 9:29–43. PMID: 24526089.
Article6. Page SJ, Levine P, Sisto S, Bond Q, Johnston MV. Stroke patients’ and therapists’ opinions of constraint-induced movement therapy. Clin Rehabil. 2002; 16:55–60. PMID: 11837526.
Article7. Choi SW, Kim KM, Jang SJ, Kim HJ, Kim SS, Son MO, et al. The importance of motivation and dropping out from treatment in constraint-induced movement therapy for stroke patients. J Korean Acad Rehabil Med. 2008; 32:20–25.8. Urra O, Casals A, Jane R. The impact of visual feedback on the motor control of the upper-limb. Conf Proc IEEE Eng Med Biol Soc. 2015; 2015:3945–3948. PMID: 26737157.
Article9. Kim CY, Lee JS, Lee JH, Kim YG, Shin AR, Shim YH, et al. Effect of spatial target reaching training based on visual biofeedback on the upper extremity function of hemiplegic stroke patients. J Phys Ther Sci. 2015; 27:1091–1096. PMID: 25995564.
Article10. Butler AJ, Page SJ. Mental practice with motor imagery: evidence for motor recovery and cortical reorganization after stroke. Arch Phys Med Rehabil. 2006; 87(12 Suppl 2):S2–S11. PMID: 17140874.
Article11. Yoon JA, Koo BI, Shin MJ, Shin YB, Ko HY, Shin YI. Effect of constraint-induced movement therapy and mirror therapy for patients with subacute stroke. Ann Rehabil Med. 2014; 38:458–466. PMID: 25229024.
Article12. Kim KS, Kim KS, Kang JY. Effects of upper extremity exercise training using biofeedback and constraint-induced movement on the upper extremity function of hemiplegic patients. J Korean Acad Nurs. 2003; 33:591–600.13. Duncan PW, Samsa GP, Weinberger M, Goldstein LB, Bonito A, Witter DM, et al. Health status of individuals with mild stroke. Stroke. 1997; 28:740–745. PMID: 9099189.
Article14. Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, et al. Interventions for improving upper limb function after stroke. Cochrane Database Syst Rev. 2014; (11):CD010820. PMID: 25387001.
Article15. Holden MK. Virtual environments for motor rehabilitation: review. Cyberpsychol Behav. 2005; 8:187–219. PMID: 15971970.
Article16. Yin CW, Sien NY, Ying LA, Chung SF, Tan May Leng D. Virtual reality for upper extremity rehabilitation in early stroke: a pilot randomized controlled trial. Clin Rehabil. 2014; 28:1107–1114. PMID: 24803644.
Article17. Blanton S, Wilsey H, Wolf SL. Constraint-induced movement therapy in stroke rehabilitation: perspectives on future clinical applications. NeuroRehabilitation. 2008; 23:15–28. PMID: 18356586.
Article18. Woldag H, Waldmann G, Heuschkel G, Hummelsheim H. Is the repetitive training of complex hand and arm movements beneficial for motor recovery in stroke patients? Clin Rehabil. 2003; 17:723–730. PMID: 14606737.19. Woldag H, Stupka K, Hummelsheim H. Repetitive training of complex hand and arm movements with shaping is beneficial for motor improvement in patients after stroke. J Rehabil Med. 2010; 42:582–587. PMID: 20549164.
Article20. Sterr A, Saunders A. CI therapy distribution: theory, evidence and practice. NeuroRehabilitation. 2006; 21:97–105. PMID: 16917157.
Article21. Sterr A, Freivogel S. Motor-improvement following intensive training in low-functioning chronic hemiparesis. Neurology. 2003; 61:842–844. PMID: 14504336.
Article22. Brogardh C, Sjolund BH. Constraint-induced movement therapy in patients with stroke: a pilot study on effects of small group training and of extended mitt use. Clin Rehabil. 2006; 20:218–227. PMID: 16634340.
Article23. Souza WC, Conforto AB, Orsini M, Stern A, Andre C. Similar effects of two modified constraint-induced therapy protocols on motor impairment, motor function and quality of life in patients with chronic stroke. Neurol Int. 2015; 7:5430. PMID: 26294941.
Article24. Treger I, Aidinof L, Lehrer H, Kalichman L. Constraint-induced movement therapy alters cerebral blood flow in subacute post-stroke patients. Am J Phys Med Rehabil. 2012; 91:804–809. PMID: 22660371.
Article25. Shi YX, Tian JH, Yang KH, Zhao Y. Modified constraint-induced movement therapy versus traditional rehabilitation in patients with upper-extremity dysfunction after stroke: a systematic review and metaanalysis. Arch Phys Med Rehabil. 2011; 92:972–982. PMID: 21621674.
Article26. Pedlow K, Lennon S, Wilson C. Application of constraint-induced movement therapy in clinical practice: an online survey. Arch Phys Med Rehabil. 2014; 95:276–282. PMID: 24025659.
Article27. Burns A, Burridge J, Pickering R. Does the use of a constraint mitten to encourage use of the hemiplegic upper limb improve arm function in adults with subacute stroke? Clin Rehabil. 2007; 21:895–904. PMID: 17981848.
Article28. Gauthier LV, Taub E, Perkins C, Ortmann M, Mark VW, Uswatte G. Remodeling the brain: plastic structural brain changes produced by different motor therapies after stroke. Stroke. 2008; 39:1520–1525. PMID: 18323492.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Upper Extremity Exercise Training Using Biefeedback and Constraint-induced Movement on the Upper Extremity Function of Hemiplegic Patients
- Effect of Constraint-Induced Movement Therapy and Mirror Therapy for Patients With Subacute Stroke
- Effect of Constraint-Induced Movement Therapy in Chronic Hemiplegic Patients
- Effects of Constraint-Induced Movement Using Self-Efficacy Enhancing Strategies on the Upper Extremity Function of Chronic Hemiplegic Patients
- The Effects of Constraint-induced Movement Therapy on Affected Upper Limb Functions in Patients with Hemiplegia