J Korean Orthop Assoc.
2017 Feb;52(1):33-39. 10.4055/jkoa.2017.52.1.33.
The Optimal Surgical Approach and Complications in Resecting Osteochondroma around the Lesser Trochanter
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea Cancer Center Hospital, Seoul, Korea. dgjeon@kirams.re.kr
- KMID: 2369569
- DOI: http://doi.org/10.4055/jkoa.2017.52.1.33
Abstract
- PURPOSE
Surgical risks associated with the resection of osteochondroma around the proximal tibia and fibula, as well as the proximal humerus have been well established; however, the clinical presentation and optimal surgical approach for osteochondroma around the lesser trochanter have not been fully addressed.
MATERIALS AND METHODS
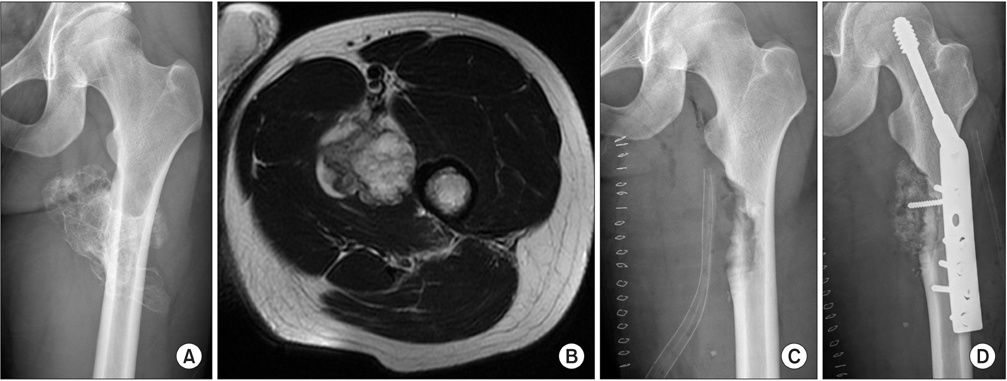
Thirteen patients with osteochondroma around the lesser trochanter underwent resection. We described the chief complaint, duration of symptom, location of the tumor, mass protrusion pattern on axial computed tomography image, tumor volume, surgical approach, iliopsoas tendon integrity after resection, and complication according to the each surgical approach.
RESULTS
Pain on walking or exercise was the chief complaint in 7 patients, and numbness and radiating pain in 6 patients. The average duration of symptom was 19 months (2-72 months). The surgical approach for 5 tumors that protruded postero-laterally was postero-lateral (n=3), anterior (n=1), and medial (n=1). All 4 patients with antero-medially protruding tumor underwent the anterior approach. Two patients with both antero-medially and postero-laterally protruding tumor received the medial and anterior approach, respectively. Two patients who underwent medial approach for postero-laterally protruded tumor showed extensive cortical defect after resection. One patient who received the anterior approach to resect a large postero-laterally protruded tumor developed complete sciatic nerve palsy, which was recovered 6 months after re-exploration.
CONCLUSION
For large osteochondromas with posterior protrusion, we should not underestimate the probability of sciatic nerve compression. When regarding the optimal surgical approach, the medial one is best suitable for small tumors, while the anterior approach is good for antero-medial or femur neck tumor. For postero-laterally protruded large tumors, posterior approach may minimize the risk of sciatic nerve palsy.
Keyword
MeSH Terms
Figure
Reference
-
1. Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH. Imaging of osteochondroma: variants and complications with radiologic-pathologic correlation. Radiographics. 2000; 20:1407–1434.
Article2. Stieber JR, Dormans JP. Manifestations of hereditary multiple exostoses. J Am Acad Orthop Surg. 2005; 13:110–120.
Article3. de Souza AM, Bispo Júnior RZ. Osteochondroma: ignore or investigate? Rev Bras Ortop. 2014; 49:555–564.
Article4. Saglik Y, Altay M, Unal VS, Basarir K, Yildiz Y. Manifestations and management of osteochondromas: a retrospective analysis of 382 patients. Acta Orthop Belg. 2006; 72:748–755.5. Wirganowicz PZ, Watts HG. Surgical risk for elective excision of benign exostoses. J Pediatr Orthop. 1997; 17:455–459.
Article6. Eschelman DJ, Gardiner GA Jr, Deely DM. Osteochondroma: an unusual cause of vascular disease in young adults. J Vasc Interv Radiol. 1995; 6:605–613.
Article7. Makhdom AM, Jiang F, Hamdy RC, Benaroch TE, Lavigne M, Saran N. Hip joint osteochondroma: systematic review of the literature and report of three further cases. Adv Orthop. 2014; 2014:180254.
Article8. Yu Y, Sun X, Song X, Tian Z, Zhou Y. A novel surgical approach for the treatment of tumors in the lesser trochanter. Exp Ther Med. 2015; 10:201–206.
Article9. Li M, Luettringhaus T, Walker KR, Cole PA. Operative treatment of femoral neck osteochondroma through a digastric approach in a pediatric patient: a case report and review of the literature. J Pediatr Orthop B. 2012; 21:230–234.10. Göbel V, Jürgens H, Etspüler G, et al. Prognostic significance of tumor volume in localized Ewing's sarcoma of bone in children and adolescents. J Cancer Res Clin Oncol. 1987; 113:187–191.
Article11. Weinstein SL, Ponseti IV. Congenital dislocation of the hip. J Bone Joint Surg Am. 1979; 61:119–124.
Article12. Ludloff K. The open reduction of the congenital hip dislocation by an anterior incision. J Bone Joint Surg Am. 1913; 210:438–454.13. Moore AT. The moore self-locking Vitallium prosthesis in fresh femoral neck fractures: a new low posterior approach (the southern exposure). AAOS Instr Course Lect. 1959; 16:309–321.14. Vasseur MA, Fabre O. Vascular complications of osteochondromas. J Vasc Surg. 2000; 31:532–538.
Article15. Kong CB, Lee KY, Cho SH, et al. Rupture of a brachial artery caused by a humeral osteochondroma. J Korean Orthop Assoc. 2013; 48:297–301.
Article16. Ramos-Pascua LR, Sánchez-Herráez S, Alonso-Barrio JA, Alonso-León A. Solitary proximal end of femur osteochondroma. An indication and result of the en bloc resection without hip luxation. Rev Esp Cir Ortop Traumatol. 2012; 56:24–31.
Article17. Kim HJ, Kim SS, Kim CH, Kim HJ. Sciatic nerve compression secondary due to ischial tuberosity osteochondroma. J Korean Hip Soc. 2012; 24:65–69.
Article18. Yu K, Meehan JP, Fritz A, Jamali AA. Osteochondroma of the femoral neck: a rare cause of sciatic nerve compression. Orthopedics [Internet]. 2010. cited 2010 Aug 11. 2010;33. DOI: 10.3928/01477447-20100625-26. Available from: http://www.healio.com/orthopedics/journals/ortho/2010-8-33-8/%7Bd3161a80-dff0-42b3-ad54-bb3eb266cd00%7D/osteochondroma-of-the-femoral-neck-a-rare-cause-of-sciatic-nerve-compression.19. Bottner F, Rodl R, Kordish I, Winklemann W, Gosheger G, Lindner N. Surgical treatment of symptomatic osteochondroma. A three- to eight-year follow-up study. J Bone Joint Surg Br. 2003; 85:1161–1165.20. Tschokanow K. 2 cases of osteochondroma of the femur neck. Beitr Orthop Traumatol. 1969; 16:751–752.21. Siebenrock KA, Ganz R. Osteochondroma of the femoral neck. Clin Orthop Relat Res. 2002; 394:211–218.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Osteochondroma on the Mandibular Condyle through Intraoral Approach: Case Report
- New Wiring Method for Lesser Trochanter Fixation in Unstable Intertrochanteric Fractures: Technical Note
- Delayed Pseudoaneurysm of Deep Femoral Artery Caused by Migration of Lesser Trochanter, Subsequent to an Intertrochanteric Fracture Surgery - A Case Report -
- Injury of the Ascending Branch of the Lateral Femoral Circumflex Artery Caused by a Spike of the Displaced Lesser Trochanter in an Intertrochanteric Femoral Fracture - A Case Report -
- Stress Fracture after Arthroscopic Lesser Trochanter Resection: Diagnosis and Therapy