J Dent Rehabil Appl Sci.
2016 Dec;32(4):263-273. 10.14368/jdras.2016.32.4.263.
A literature review on implant abutment and soft tissue response
- Affiliations
-
- 1Department of Prosthodontics and Research Institute of Oral Science, College of Dentistry, Gangneung-Wonju National University, Gangneung, Republic of Korea. lila@gwnu.ac.kr
- KMID: 2369066
- DOI: http://doi.org/10.14368/jdras.2016.32.4.263
Abstract
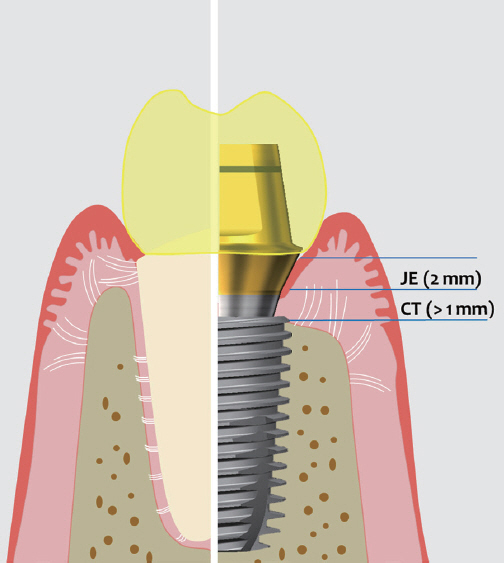
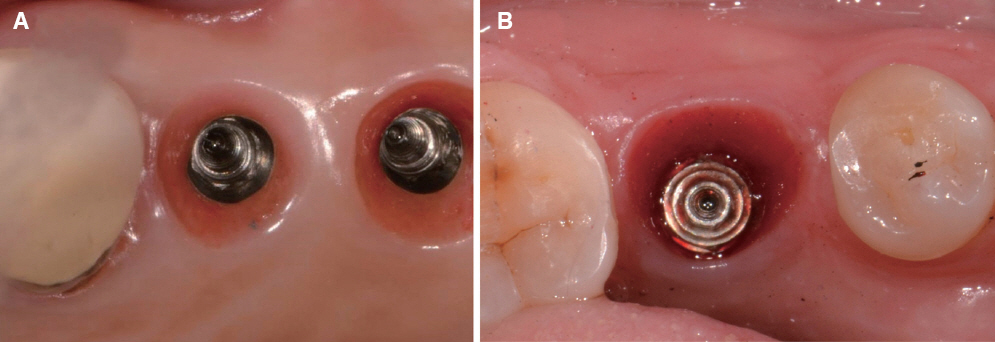
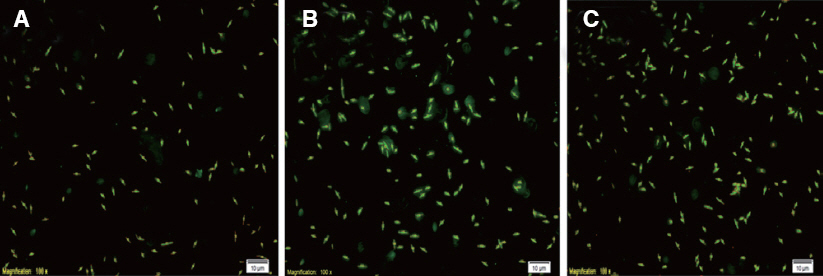
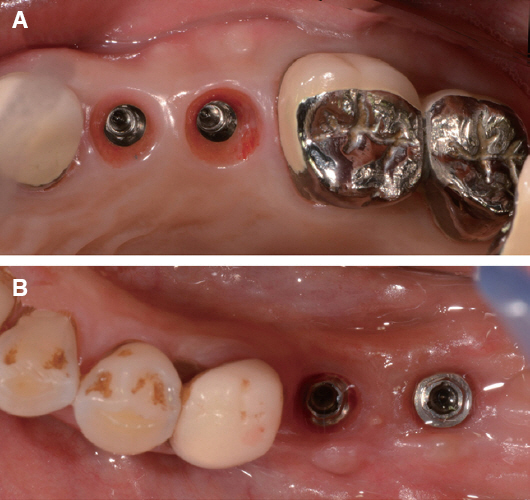
- In the implant prosthetic procedure, the soft tissue reaction was varied with the material and surface treatment of the abutment. It may be the cause of the peri-implantitis, and hence it can affect the long-term prognosis of the implant prosthesis. Titania and zirconia abutment presented superior biocompatibility and stable soft tissue reaction, while gold alloy abutment showed unfavorable reaction sometimes. A soft tissue reaction can be differed by the surface characteristics even in the same material type. Because rougher surface induces a bacterial attachment, the part contacting a soft tissue should have smooth surface. Additional surface treatment can enhance the cellular response without increasing bacterial attachment. Repeated removal and insertion of the abutment and the shape of the abutment may affect the soft tissue reaction, also. Ultrasonic cleaning and argon plasma cleaning are effective way to clean the retained micro-dust on the customized abutment.
Keyword
Figure
Reference
-
References
1. Berglundh T, Lindhe J. Dimension of the periimplant mucosa. Biological width revisited. J Clin Periodontol. 1996; 23:971–3. DOI: 10.1111/j.1600-051X.1996.tb00520.x. PMID: 8915028.2. Nakamura K, Kanno T, Milleding P, Ortengren U. Zirconia as a dental implant abutment material: a systematic review. Int J Prosthodont. 2010; 23:299309.3. Nothdurft FP, Fontana D, Ruppenthal S, May A, Aktas C, Mehraein Y, Lipp P, Kaestner L. Differential behavior of fibroblasts and epithelial cells on structured implant abutment materials: a comparison of materials and surface topographies. Clin Implant Dent Relat Res. 2015; 17:1237–49. DOI: 10.1111/cid.12253. PMID: 25066589.4. Tomasi C, Tessarolo F, Caola I, Wennström J, Nollo G, Berglundh T. Morphogenesis of peri-implant mucosa revisited: an experimental study in humans. Clin Oral Implants Res. 2014; 25:997–1003. DOI: 10.1111/clr.12223. PMID: 23799997.5. Buser D, Weber HP, Donath K, Fiorellini JP, Paquette DW, Williams RC. Soft tissue reactions to non-submerged unloaded titanium implants in beagle dogs. J Periodontol. 1992; 63:225–35. DOI: 10.1902/jop.1992.63.3.225. PMID: 1593416.6. Berglundh T, Lindhe J, Ericsson I, Marinello CP, Liljenberg B, Thomsen P. The soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991; 2:81–90. DOI: 10.1034/j.1600-0501.1991.020206.x. PMID: 1809403.7. Abrahamsson I, Berglundh T, Glantz PO, Lindhe J. The mucosal attachment at different abutments. An experimental study in dogs. J Clin Periodontol. 1998; 25:721–7. DOI: 10.1111/j.1600-051X.1998.tb02513.x. PMID: 9763327.8. Abrahamsson I, Cardaropoli G. Peri-implant hard and soft tissue integration to dental implants made of titanium and gold. Clin Oral Implants Res. 2007; 18:269–74. DOI: 10.1111/j.1600-0501.2006.01326.x. PMID: 17298489.9. Welander M, Abrahamsson I, Berglundh T. The mucosal barrier at implant abutments of different materials. Clin Oral Implants Res. 2008; 19:635–41. DOI: 10.1111/j.1600-0501.2008.01543.x-i2. DOI: 10.1111/j.1600-0501.2008.01543.x. PMID: 18492075.10. van Brakel R, Meijer GJ, Verhoeven JW, Jansen J, de Putter C, Cune MS. Soft tissue response to zirconia and titanium implant abutments: an in vivo within-subject comparison. J Clin Periodontol. 2012; 39:995–1001. DOI: 10.1111/j.1600-051X.2012.01931.x. PMID: 22862854.11. Moon YH, Yoon MK, Moon JS, Kang JH, Kim SH, Yang HS, Kim MS. Focal adhesion linker proteins expression of fibroblast related to adhesion in response to different transmucosal abutment surfaces. J Adv Prosthodont. 2013; 5:341–50. DOI: 10.4047/jap.2013.5.3.341. PMID: 24049577. PMCID: PMC3774950.12. Nothdurft FP, Fontana D, Ruppenthal S, May A, Aktas C, Mehraein Y, Lipp P, Kaestner L. Differential behavior of fibroblasts and epithelial cells on structured implant abutment materials: a comparison of materials and surface topographies. Clin Implant Dent Relat Res. 2015; 17:1237–49. DOI: 10.1111/cid.12253. PMID: 25066589.13. Kim YS, Ko Y, Kye SB, Yang SM. Human gingival fibroblast (HGF-1) attachment and proliferation on several abutment materials with various colors. Int J Oral Maxillofac Implants. 2014; 29:969–75. DOI: 10.11607/jomi.3704. PMID: 24914814.14. Rutkunas V, Bukelskiene V, Sabaliauskas V, Balciunas E, Malinauskas M, Baltriukiene D. Assessment of human gingival fibroblast interaction with dental implant abutment materials. J Mater Sci Mater Med. 2015; 26:169. DOI: 10.1007/s10856-015-5481-8. PMID: 25804303.15. Lindhe J, Meyle J; Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008; 35:282–5. DOI: 10.1111/j.1600-051X.2008.01283.x. PMID: 18724855.16. Agerbaek MR, Lang NP, Persson GR. Comparisons of bacterial patterns present at implant and tooth sites in subjects on supportive periodontal therapy I. Impact of clinical variables, gender and smoking. Clin Oral Implants Res. 2006; 17:18–24. DOI: 10.1111/j.1600-0501.2005.01190.x. PMID: 16441781.17. Subramani K, Jung RE, Molenberg A, Hammerle CH. Biofilm on dental implants: a review of the literature. Int J Oral Maxillofac Implants. 2009; 24:61626.18. Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A. Bacterial adhesion on commercially pure titanium and zirconium oxide disks: an in vivo human study. J Periodontol. 2004; 75:292–6. DOI: 10.1902/jop.2004.75.2.292. PMID: 15068118.19. van Brakel R, Cune MS, van Winkelhoff AJ, de Putter C, Verhoeven JW, van der Reijden W. Early bacterial colonization and soft tissue health around zirconia and titanium abutments: an in vivo study in man. Clin Oral Implants Res. 2011; 22:571–7. DOI: 10.1111/j.1600-0501.2010.02005.x. PMID: 21054554.20. Bollen CM, Lambrechts P, Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature. Dent Mater. 1997; 13:258–69. DOI: 10.1016/S0109-5641(97)80038-3.21. Salihoglu U, Boynuegri D, Engin D, Duman AN, Gokalp P, Balos K. Bacterial adhesion and colonization differences between zirconium oxide and titanium alloys: an in vivo human study. Int J Oral Maxillofac Implants. 2011; 26:101–7. PMID: 21365044.22. de Avila ED, Avila-Campos MJ, Vergani CE, Spolidório DM, Mollo Fde A Jr. Structural and quantitative analysis of a mature anaerobic biofilm on different implant abutment surfaces. J Prosthet Dent. 2016; 115:428–36. DOI: 10.1016/j.prosdent.2015.09.016. PMID: 26597465.23. Yamane K, Ayukawa Y, Takeshita T, Furuhashi A, Yamashita Y, Koyano K. Bacterial adhesion affinities of various implant abutment materials. Clin Oral Implants Res. 2013; 24:1310–5. DOI: 10.1111/j.1600-0501.2012.02574.x. PMID: 22925147.24. Kim HY, Yeo IS, Lee JB, Kim SH, Kim DJ, Han JS. Initial in vitro bacterial adhesion on dental restorative materials. Int J Artif Organs. 2012; 35:773–79. DOI: 10.5301/ijao.5000153.25. Kim ML, Jeong CM, Jeon YC, Byon E, Jeong Y, Cho LR. The effects of Mg-ion implantation and sandblasting on Porphyromonas gingivalis attachment. Clin Oral Implants Res. 2012; 23:245–52. DOI: 10.1111/j.1600-0501.2010.02138.x. PMID: 21426403.26. Kang SN, Jeong CM, Jeon YC, Byon ES, Jeong YS, Cho LR. Effects of Mg-ion and Ca-ion Implantations on P. gingivalis and F. nucleatum Adhesion. Tissue Eng Regen Med. 2014; 11:39–46. DOI: 10.1007/s13770-013-1104-y.27. Sawase T, Wennerberg A, Hallgren C, Albrektsson T, Baba K. Chemical and topographical surface analysis of five different implant abutments. Clin Oral Implants Res. 2000; 11:44–50. DOI: 10.1034/j.1600-0501.2000.011001044.x. PMID: 11168193.28. Guida L, Oliva A, Basile MA, Giordano M, Nastri L, Annunziata M. Human gingival fibroblst functions are stimulated by oxidized nano-structured titanium surfaces. J Dent. 2013; 41:900–7. DOI: 10.1016/j.jdent.2013.07.009. PMID: 23907085.29. Lee DW, Kim JG, Kim MK, Ansari S, Moshaverinia A, Choi SH, Ryu JJ. Effect of laser-dimpled titanium surfaces on attachment of epithelial-like cells and fibroblsts. J Adv Prosthodont. 2015; 7:138–45. DOI: 10.4047/jap.2015.7.2.138. PMID: 25932312. PMCID: PMC4414944.30. Pecora GE, Ceccarelli R, Bonelli M, Alexander H, Ricci JL. Clinical evaluation of laser microtexturing for soft tissue and bone attachment to dental implants. Implant Dent. 2009; 18:57–66. DOI: 10.1097/ID.0b013e31818c5a6d. PMID: 19212238.31. Nevins M, Kim DM, Jun SH, Guze K, Schupbach P, Nevins ML. Histologic evidence of a connective tissue attachment to laser microgrooved abutments: a canine study. Int J Periodontics Restorative Dent. 2010; 30:245–55. PMID: 20386781.32. Li P, Tong Z, Huo L, Yang F, Su W. Antibacterial and biological properties of biofunctionalized nanocomposites on titanium for implant application. J Biomater Appl. 2016; 31:205–14. DOI: 10.1177/0885328216645951. PMID: 27114441.33. Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone changes around titanium implants. A histomertric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001; 72:1372–83. DOI: 10.1902/jop.2001.72.10.1372. PMID: 11699479.34. Alves CC, Muñoz F, Cantalapiedra A, Ramos I, Neves M, Blanco J. Marginal bone and soft tissue behavior following platform switching abutment connection/disconnection-a dog model study. Clin Oral Implants Res. 2015; 26:983–91. DOI: 10.1111/clr.12385. PMID: 24735458.35. Iglhaut G, Becker K, Golubovic V, Schliephake H, Mihatovic I. The impact of dis-/reconnection of laser microgrooved and machined implant abutments on soft- and hard-tissue healing. Clin Oral Implants Res. 2013; 24:391–7. DOI: 10.1111/clr.12040. PMID: 23009248.36. Farronato D, Santoro G, Canullo L, Botticelli D, Maiorana C, Lang NP. Establishment of the epithelial attachment and connective tissue adaptation to implants installed under the concept of “platform switching”: a histologic study in minipigs. Clin Oral Implants Res. 2012; 23:90–4. DOI: 10.1111/j.1600-0501.2011.02196.x. PMID: 21492239.37. Huh JB, Rheu GB, Kim YS, Jeong CM, Lee JY, Shin SW. Influence of Implant transmucosal design on early peri-implant tissue responses in beagle dogs. Clin Oral Implants Res. 2014; 25:962–8. DOI: 10.1111/clr.12179. PMID: 23647221.38. Kim S, Oh KC, Han DH, Heo SJ, Ryu IC, Kwon JH, Han CH. Influence of transmucosal designs of three one-piece implant systems on early tissue responses: a histometric study in beagle dogs. Int J Oral Maxillofac Implants. 2010; 25:309–14. PMID: 20369089.39. Iglhaut G, Schwarz F, Winter RR, Mihatovic I, Stimmelmayr M, Schliephake H. Epithelial attachment and downgrowth on dental implant abutments-a comprehensive review. J Esthet Restor Dent. 2014; 26:324–31. DOI: 10.1111/jerd.12097. PMID: 24612047.40. Canullo L, Micarelli C, Lembo-Fazio L, Iannello G, Clementini M. Microscopical and microbiologic characterization of customized titanium abutments after different cleaning procedures. Clin Oral Implants Res. 2014; 25:328–36. DOI: 10.1111/clr.12089. PMID: 23210704.41. Gehrke P, Tabellion A, Fischer C. Microscopical and chemical surface characterization of CAD/CAM zirconia abutment after different cleaning procedures. A qualitative analysis. J Adv Prosthodont. 2015; 7:151–9. DOI: 10.4047/jap.2015.7.2.151. PMID: 25932314. PMCID: PMC4414946.42. Canullo L, Peñarrocha D, Clementini M, Iannello G, Micarelli C. Impact of plasma of argon cleaning treatment on implant abutments in patients with a history of periodontal disease and thin biotype: radiographic results at 24-month follow-up of a RCT. Clin Oral Implants Res. 2015; 26:8–14. DOI: 10.1111/clr.12290. PMID: 24191873.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical case of implant restoration using customized healing abutment
- Improvement of peri-implant complications through customized prosthesis restoration allowing soft tissue space: a case report
- Considerations in implant crestal module to preserve peri-implant tissue
- Concept and application of implant connection systems: Part II. Placement and restoration of external connection implant and tissue level implant
- Maxillary anterior single implant prosthesis