J Korean Med Assoc.
2017 Jan;60(1):72-80. 10.5124/jkma.2017.60.1.72.
Duration of and fee for comprehensive assessment and care planning for patients with hypertension and/or diabetes in primary care
- Affiliations
-
- 1Department of Health Policy and Management, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Social and Preventive Medicine, College of Medicine, Hallym University, Chuncheon, Korea. ychoi@hallym.ac.kr
- 3Health Services Research Center, Hallym University, Chuncheon, Korea.
- 4Public Health Medical Service, Seoul National University Hospital, Seoul, Korea.
- 5Institute of Health Policy and Management, Medical Research Center, Seoul National University, Seoul, Korea.
- KMID: 2367732
- DOI: http://doi.org/10.5124/jkma.2017.60.1.72
Abstract
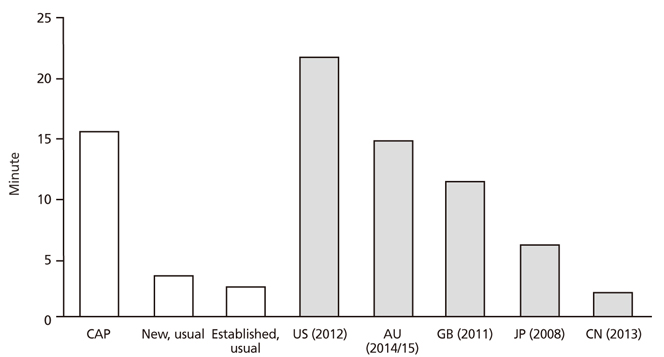
- The enhanced primary care demonstration (EPD) was launched in November 2014 to provide high-quality care for people with chronic illnesses. In the EPD, comprehensive assessment and care planning (CAP) is a critical component, along with behavior modification and case management services. In this study, we measured CAP duration and calculated the fee for CAP sessions performed with patients with hypertension and/or diabetes mellitus. In 5 primary care clinics participating in the EPD, the duration of CAP sessions and usual consultations was measured. The duration of CAP sessions was measured on 2 separate occasions because CAP involves 2 separate consultations, including an initial consultation for comprehensive patient assessment and laboratory testing and a follow-up consultation for creating a care plan based on the assessment and test results. The CAP fee was calculated as the ratio of CAP time to the usual consultation time. The median (interquartile range) and the mean ± standard deviation of CAP duration were 15.4 (7.1) minutes and 15.6 ± 4.2 minutes, respectively. The first and second CAP sessions lasted for 5.3 and 4.6 times longer than usual consultations, respectively. The calculated CAP fees were 76,299 won (median) and 65,766 won (mean). The length of CAP sessions for patients with hypertension and/or diabetes mellitus was approximately 5 times longer than that of usual consultations. If consultation lengths were measured in a representative patient sample, it would be possible to improve the external validity of the measurements.
MeSH Terms
Figure
Reference
-
1. Korea Centers for Disease Control and Prevention. Disease control white paper 2007. Seoul: Centers for Disease Control and Prevention;2008.2. Ministry of Health and Welfare. Health and welfare white paper 2010. Seoul: Ministry of Health and Welfare;2011.3. Ministry of Health and Welfare. Health and welfare white paper 2011. Seoul: Ministry of Health and Welfare;2012.4. Ministry of Health and Welfare. Health and welfare white paper 2013. Seoul: Ministry of Health and Welfare;2014.5. Ministry of Health and Welfare. Health and welfare white paper 2012. Seoul: Ministry of Health and Welfare;2013.6. Ministry of Health and Welfare. Health and welfare white paper 2014. Seoul: Ministry of Health and Welfare;2015.7. Cho JJ, Kwon YJ, Jung SH. Community based health care service design on chronic disease for enhancing primary care and the status of community based primary care project. Korean J Fam Pract. 2015; 5:173–178.8. Cho B, Park JH, Son KY, Shin DW, Kim SH, Seo YG, Min HY, Kim SJ, Kim SH, Jeong SM, Jeong WJ, Park MH. Development of a service model for chronic care in primary care. Seoul: National Evidence-based Healthcare Collaborating Agency;2016.9. Kim Y, Choi Y, An AR, Lee JH. Development of a payment model for chronic care in primary care. Seoul: National Evidence-based Healthcare Collaborating Agency;2016.10. Lee CS, Kang GW, Byeon SA. Unit for Relative Value Scale Research and Development. A research report on relative value scale revision. Seoul: Health Insurance Review and Assessment Service;2006.11. Jeon CS, Park HG, Yeom W, Hong SB, Lee WP, Ji YG, Kim YJ, Yang HS, Jang SI. Korean Medical Association. Revaluation of Korean evaluation and management fee. Seoul: Health Insurance Review and Assessment Service;2009.12. Centers for Disease Control and Prevention, National Center for Health Statistics. National Ambulatory Medical Care Survey: 2012 state and national summary tables [Internet]. Atlanta: Centers for Disease Control and Prevention;2016. cited 2016 Sep 15. Available from: http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2012_namcs_web_tables.pdf.13. Britt H, Miller GC, Henderson J, Bayram C, Harrison C, Valenti L, Wong C, Gordon J, Pollack AJ, Pan Y, Charles J. General practice activity in Australia 2014-15. Sydney: Sydney University Press;2015.14. Drennan VM, Halter M, Joly L, Gage H, Grant RL, Gabe J, Brearley S, Carneiro W, de Lusignan S. Physician associates and GPs in primary care: a comparison. Br J Gen Pract. 2015; 65:e344–e350.
Article15. Jin G, Zhao Y, Chen C, Wang W, Du J, Lu X. The length and content of general practice consultation in two urban districts of Beijing: a preliminary observation study. PLoS One. 2015; 10:e0135121.
Article16. Wooldridge AN, Arato N, Sen A, Amenomori M, Fetters MD. Truth or fallacy? Three hour wait for three minutes with the doctor: findings from a private clinic in rural Japan. Asia Pac Fam Med. 2010; 9:11.
Article17. Park SH. Analysis of factors delaying on waiting time for medical examination of outpatient on a hospital. Qual Improv Health Care. 2001; 8:56–72.18. Hwang JI. Factors influencing consultation time and waiting time of ambulatory patients in a tertiary teaching hospital. Qual Improv Health Care. 2006; 12:6–16.19. Lee CH, Lim H, Kim Y, Park AH, Park EC, Kang JG. Analysis of appropriate outpatient consultation time for clinical departments. Health Policy Manag. 2014; 24:254–260.
Article20. Freeman GK, Horder JP, Howie JG, Hungin AP, Hill AP, Shah NC, Wilson A. Evolving general practice consultation in Britain: issues of length and context. BMJ. 2002; 324:880–882.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in the Mixed Fee-Based Payment System in Primary Care: Cases and Implications
- Care Tips for Self-Care among Older Diabetic Patients
- Direction of Health Care and Health Insurance System Reform to Strengthen Primary Care: Comparative Analysis of Korea, Japan and Taiwan
- Current Status and Future Directions of Primary Care in the World: Insights from Australia
- Comprehensive Management in Patients with Type 2 Diabetes Mellitus