Yonsei Med J.
2015 Jul;56(4):1114-1121. 10.3349/ymj.2015.56.4.1114.
The Effects of Oral Atenolol or Enalapril Premedication on Blood Loss and Hypotensive Anesthesia in Orthognathic Surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. sjbai1@yuhs.ac
- 2Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 4Department of Oral and Maxillofacial Surgery, Oral Science Research Center, College of Dentistry, Yonsei University, Seoul, Korea.
- KMID: 2366355
- DOI: http://doi.org/10.3349/ymj.2015.56.4.1114
Abstract
- PURPOSE
The aim of this study was to evaluate the effects of premedication with oral atenolol or enalapril, in combination with remifentanil under sevoflurane anesthesia, on intraoperative blood loss by achieving adequate deliberate hypotension (DH) during orthognathic surgery. Furthermore, we investigated the impact thereof on the amount of nitroglycerin (NTG) administered as an adjuvant agent.
MATERIALS AND METHODS
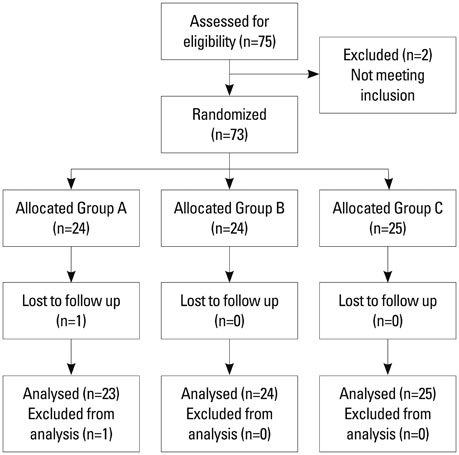
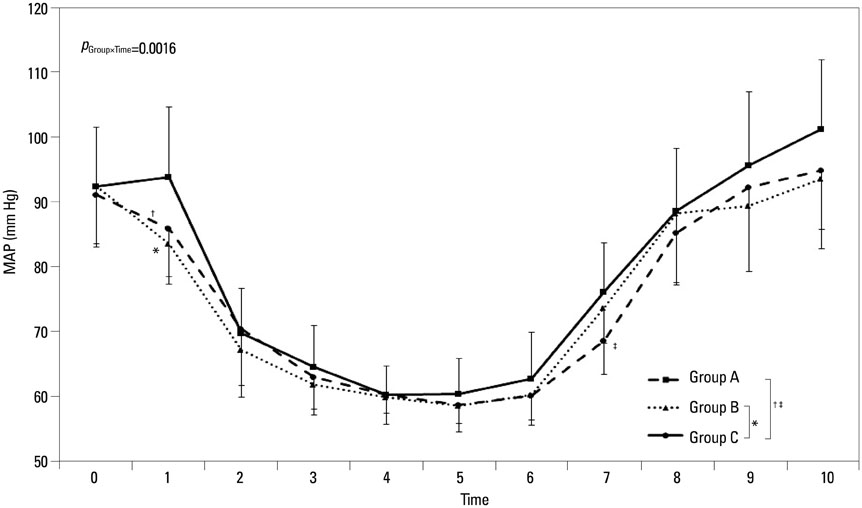
Seventy-three patients undergoing orthognathic surgery were randomly allocated into one of three groups: an angiotensin converting enzyme inhibitor group (Group A, n=24) with enalapril 10 mg, a beta blocker group (Group B, n=24) with atenolol 25 mg, or a control group (Group C, n=25) with placebo. All patients were premedicated orally 1 h before the induction of anesthesia. NTG was the only adjuvant agent used to achieve DH when mean arterial blood pressure (MAP) was not controlled, despite the administration of the maximum remifentanil dose (0.3 microg kg-1min-1) with sevoflurane.
RESULTS
Seventy-two patients completed the study. Blood loss was significantly reduced in Group A, compared to Group C (adjusted p=0.045). Over the target range of MAP percentage during DH was significantly higher in Group C than in Groups A and B (adjusted p-values=0.007 and 0.006, respectively). The total amount of NTG administered was significantly less in Group A than Group C (adjusted p=0.015).
CONCLUSION
Premedication with enalapril (10 mg) combined with remifentanil under sevoflurane anesthesia attenuated blood loss and achieved satisfactory DH during orthognathic surgery. Furthermore, the amount of NTG was reduced during the surgery.
Keyword
MeSH Terms
-
Administration, Oral
Adrenergic beta-Antagonists/administration & dosage/*pharmacology
Adult
Aged
*Anesthesia, Inhalation
Atenolol/administration & dosage/*pharmacology
Blood Loss, Surgical
Blood Pressure/drug effects
Cardiac Output/drug effects
Double-Blind Method
Enalapril/administration & dosage/*pharmacology
Female
Heart Rate/drug effects
Humans
Intraoperative Care
Male
Methyl Ethers/*administration & dosage
Middle Aged
*Orthognathic Surgical Procedures
Piperidines/*administration & dosage
*Premedication
Treatment Outcome
Adrenergic beta-Antagonists
Atenolol
Enalapril
Methyl Ethers
Piperidines
Figure
Reference
-
1. Carlos E, Monnazzi MS, Castiglia YM, Gabrielli MF, Passeri LA, Guimarães NC. Orthognathic surgery with or without induced hypotension. Int J Oral Maxillofac Surg. 2014; 43:577–580.
Article2. Praveen K, Narayanan V, Muthusekhar MR, Baig MF. Hypotensive anaesthesia and blood loss in orthognathic surgery: a clinical study. Br J Oral Maxillofac Surg. 2001; 39:138–140.
Article3. Consensus conference. Perioperative red blood cell transfusion. JAMA. 1988; 260:2700–2703.4. Rohling RG, Zimmermann AP, Biro P, Haers PE, Sailer HF. Alternative methods for reduction of blood loss during elective orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999; 14:77–82.5. Enderby GE. A report on mortality and morbidity following 9,107 hypotensive anaesthetics. Br J Anaesth. 1961; 33:109–113.
Article6. Degoute CS. Controlled hypotension: a guide to drug choice. Drugs. 2007; 67:1053–1076.7. Testa LD, Tobias JD. Pharmacologic drugs for controlled hypotension. J Clin Anesth. 1995; 7:326–337.
Article8. Apipan B, Rummasak D. Efficacy and safety of oral propranolol premedication to reduce reflex tachycardia during hypotensive anesthesia with sodium nitroprusside in orthognathic surgery: a double-blind randomized clinical trial. J Oral Maxillofac Surg. 2010; 68:120–124.
Article9. Boezaart AP, van der Merwe J, Coetzee A. Comparison of sodium nitroprusside- and esmolol-induced controlled hypotension for functional endoscopic sinus surgery. Can J Anaesth. 1995; 42(5 Pt 1):373–376.
Article10. He YM, Feng L, Huo DM, Yang ZH, Liao YH. Enalapril versus losartan for adults with chronic kidney disease: a systematic review and meta-analysis. Nephrology (Carlton). 2013; 18:605–614.
Article11. Amr YM, Amin SM. Effects of preoperative β-blocker on blood loss and blood transfusion during spinal surgeries with sodium nitroprusside-controlled hypotension. Saudi J Anaesth. 2012; 6:263–267.
Article12. Petrozza PH. Induced hypotension. Int Anesthesiol Clin. 1990; 28:223–229.
Article13. Lessard MR, Trépanier CA, Baribault JP, Brochu JG, Brousseau CA, Coté JJ, et al. Isoflurane-induced hypotension in orthognathic surgery. Anesth Analg. 1989; 69:379–383.
Article14. Choi WS, Samman N. Risks and benefits of deliberate hypotension in anaesthesia: a systematic review. Int J Oral Maxillofac Surg. 2008; 37:687–703.
Article15. Precious DS, Splinter W, Bosco D. Induced hypotensive anesthesia for adolescent orthognathic surgery patients. J Oral Maxillofac Surg. 1996; 54:680–683.
Article16. Schaberg SJ, Kelly JF, Terry BC, Posner MA, Anderson EF. Blood loss and hypotensive anesthesia in oral-facial corrective surgery. J Oral Surg. 1976; 34:147–156.
Article17. Shin S, Lee JW, Kim SH, Jung YS, Oh YJ. Heart rate variability dynamics during controlled hypotension with nicardipine, remifentanil and dexmedetomidine. Acta Anaesthesiol Scand. 2014; 58:168–176.
Article18. Yoshikawa F, Kohase H, Umino M, Fukayama H. Blood loss and endocrine responses in hypotensive anaesthesia with sodium nitroprusside and nitroglycerin for mandibular osteotomy. Int J Oral Maxillofac Surg. 2009; 38:1159–1164.
Article19. Marshall WK, Bedford RF, Arnold WP, Miller ED, Longnecker DE, Sussman MD, et al. Effects of propranolol on the cardiovascular and renin-angiotensin systems during hypotension produced by sodium nitroprusside in humans. Anesthesiology. 1981; 55:277–280.
Article20. Nair S, Collins M, Hung P, Rees G, Close D, Wormald PJ. The effect of beta-blocker premedication on the surgical field during endoscopic sinus surgery. Laryngoscope. 2004; 114:1042–1046.
Article21. Tohmo H, Karanko M, Scheinin M, Viinamäki O, Salonen M, Nieminen V. Enalapril premedication attenuates the blood pressure response to tracheal intubation and stabilizes postoperative blood pressure after controlled hypotension with sodium nitroprusside in neurovascular patients. J Neurosurg Anesthesiol. 1993; 5:13–21.
Article22. Gerson JI, Allen FB, Seltzer JL, Parker FB Jr, Markowitz AH. Arterial and venous dilation by nitroprusside and nitroglycerin--is there a difference? Anesth Analg. 1982; 61:256–260.
Article23. Yaster M, Simmons RS, Tolo VT, Pepple JM, Wetzel RC, Rogers MC. A comparison of nitroglycerin and nitroprusside for inducing hypotension in children: a double-blind study. Anesthesiology. 1986; 65:175–179.
Article24. Herrick AL, Waller PC, Berkin KE, Pringle SD, Callender JS, Robertson MP, et al. Comparison of enalapril and atenolol in mild to moderate hypertension. Am J Med. 1989; 86:421–426.
Article25. Kraiczi H, Hedner J, Peker Y, Grote L. Comparison of atenolol, amlodipine, enalapril, hydrochlorothiazide, and losartan for antihypertensive treatment in patients with obstructive sleep apnea. Am J Respir Crit Care Med. 2000; 161:1423–1428.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of tranexamic acid on blood loss reduction in patients undergoing orthognathic surgery under hypotensive anesthesia: a single-center, retrospective, observational study
- Blood Loss And Hematologic Change After Orthognathic Surgery
- A hematologic study of orthognathic surgery patients
- A COMPARATIVE STUDY ON THE EFFECT OF ESMOLOL AND NITROGLYCERIN AS DRUGS FOR HYPOTENSIVE ANESTHESIA IN OREHOGNATHIC SURGERY
- Effect of Clonidine Premedication on Isoflurane Induced Hypotensive Anesthesia