J Korean Soc Spine Surg.
2016 Dec;23(4):234-238. 10.4184/jkss.2016.23.4.234.
The Co-occurance of Meningitis and Para-spinal Infection after Repetitive Procedural Treatment of the Spine: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Changwon Gyeongsang National University School of Medicine, Gyeongsangnam-do, Korea.
- 2Department of Orthopedic Surgery, Keimyung University School of Medicine, Daegu, Korea. polo4164@naver.com
- KMID: 2365084
- DOI: http://doi.org/10.4184/jkss.2016.23.4.234
Abstract
- STUDY DESIGN: Case report.
OBJECTIVES
We report a case of meningitis combined with paraspinal infection in a patients who underwent numerous surgeries for and repetitive procedural treatment of the spine. SUMMARY OF LITERATURE REVIEW: In patients with a history surgical and repetitive procedural treatment of the spine, one symptom of infection may be a fever with localized pain or tenderness along the spine.
MATERIALS AND METHODS
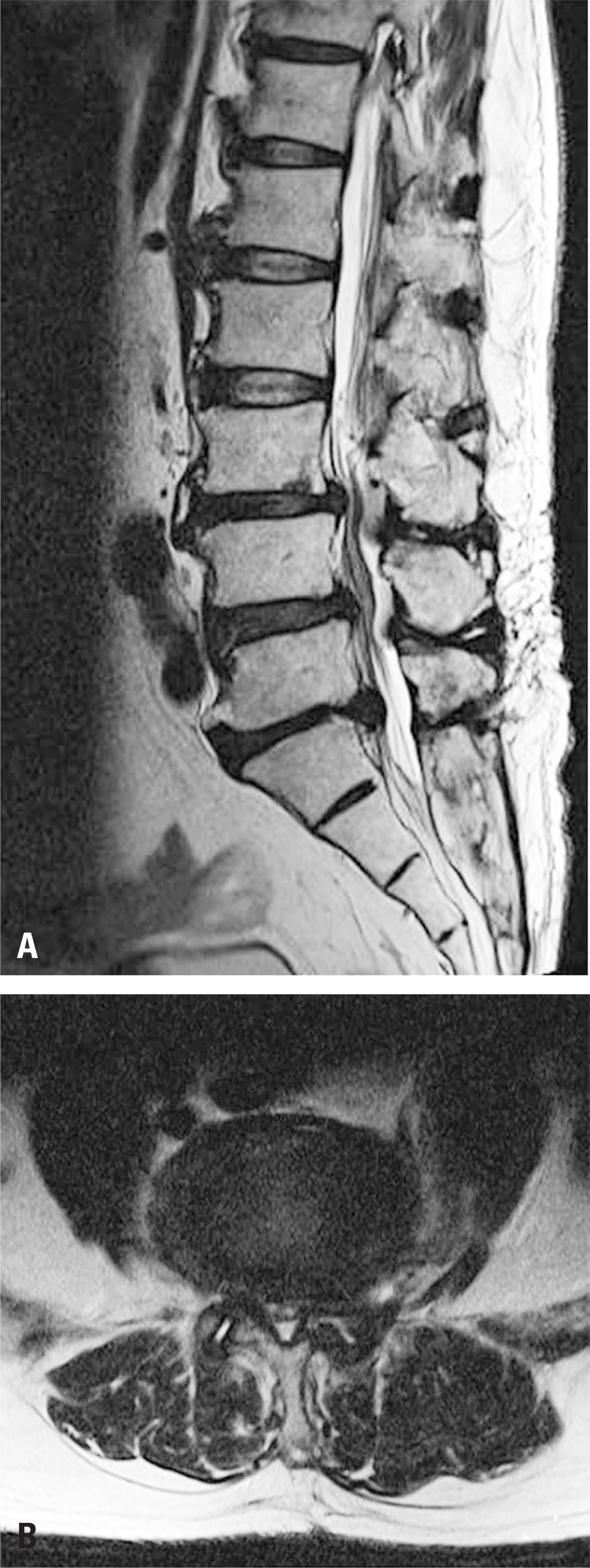
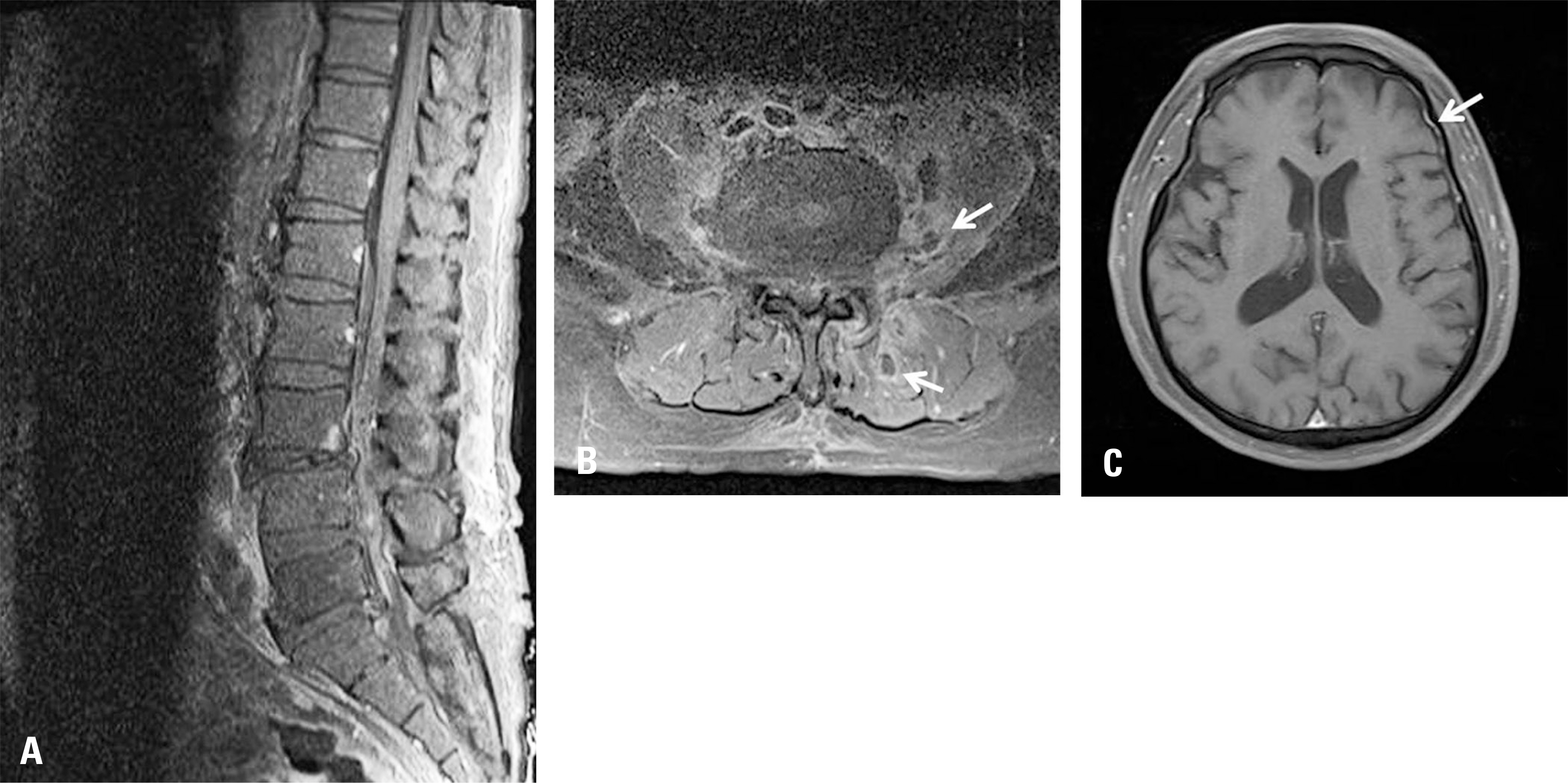
A 69-year-old man was hospitalized due to pyrexia and myalgia. Eight years ago, he underwented spine surgery. After that, the patient underwent spinal intervention more than once per week in another hospital due to remaining pain. One week before his visit to the emergency room, myalgia and aggravation in the lower back arose. However, a paraspinal infection was not detected in a non-enhanced MRI. One day after admission, the patient showed signs of meningeal irritation signs and the the patient's mental state suddenly deteriorated. An emergency cerebrospinal fluid analysis showed typical findings of bacterial meningitis. An enhanced MRI of the brain showed pachymeningeal enhancement. An enhanced MRI of the spine showed a small abscess formation on the left paravertebral back muscle, and bilateral psoas muscle.
RESULTS
Serrtia marcescens was identified on blood cultures obtained upon admission. Since antibiotics were used to treat Serratia marcescens, the fever subsided, and the patient's mental status returned to normal.
CONCLUSIONS
For patients with a history of repetitive procedural treatments of the spine, a fever should be acknowledged as a symptom in meningitis or other infectious conditions.
Keyword
MeSH Terms
Figure
Reference
-
1. Choi IH, Lee HK. Treatment of non-tuberculous infection of the spine. J Korean Orthop Assoc. 1984; 19:472–82.2. Goodman BS, Posecion LW, Mallempati S, et al. Complications and pitfalls of lumbar interlaminar and transforaminal epidural injections. Curr Rev Musculoskelet Med. 2008; 1:212–22.
Article3. Cherubin CE, Corrado ML, Nair SR, et al. Treatment of Gram-negative bacillary meningitis: role of the new cephalosporin antibiotics. Rev Infect Dis. 1982; 4:453–64.
Article4. Landesman SH, Corrado ML, Shah PM, et al. Past and current roles for cephalosporin antibiotics in treatment of meningitis. AmY Med. 1981; 71:693–703.
Article5. Olson DA, Hoeprich PD, Nolan SM, et al. Successful treatment of Gram-negative bacillary meningitis with Moxa-lactam. Ann Intern Med. 1981; 95:302–5.
Article6. Stratton CW. Serratia marcescens. Infect Control. 1983; 4:469–71.7. Chang CJ, Ye JJ, Yang CC, et al. Influence of Third-generation Cephalosporin Resistance on Adult In-hospital Mortality From Post-neurosurgical Bacterial Meningitis. J Microbiol Immunol Infect. 2010; 43:301–9.
Article8. Wu YM, Hsu PC, Yang CC, et al. Serratia marcescens meningitis: Epidemiology, prognostic factors and treatment outcomes. J Microbiol Immunol Infect. 2013; 46:259–65.
Article9. Durand ML, Calderwood SB, Weber DJ, et al. Acute bacterial meningitis in adults: a review of 493 episodes. N Engl J Med. 1993; 328:21–8.10. Sigurardottir B, Bjornsson OM, Jonsdottir KE, et al. Acute bacterial meningitis in adults: a 20-year overview. Arch Intern Med. 1997; 157:425–30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Streptococcus viridans Meningitis After Epidural Nerve Block
- Gas-Containing Cervical Epidural Abscess Accompanying Bacterial Meningitis in an Adult
- Postoperative Meningitis in Patients with Cervical Cord Tumor: A Case Report
- Unusual Fatal Infections after Anterior Cervical Spine Surgeries
- Recurrent Bacterial Meningitis Accompanied by A Spinal Intramedullary Abscess