Korean J Ophthalmol.
2016 Feb;30(1):48-52. 10.3341/kjo.2016.30.1.48.
Comparison of Postoperative Exodrift after First Unilateral and Second Contralateral Lateral Rectus Recession in Recurrent Exotropia
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Uijeongbu St. Mary's Hospital, The Catholic University of Korea College of Medicine, Uijeongbu, Korea. yclee@cmcnu.or.kr
- 2Department of Ophthalmology, St. Vincet's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea.
- 3Department of Ophthalmology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- KMID: 2363890
- DOI: http://doi.org/10.3341/kjo.2016.30.1.48
Abstract
- PURPOSE
To compare postoperative exodrift of the first unilateral lateral rectus (ULR) muscle recession with the exodrift of the second contralateral ULR muscle recession in patients with recurrent small-angle exotropia (XT).
METHODS
We evaluated the results of a second ULR muscle recession in 19 patients with recurrent XT with deviation angles under 25 prism diopter (PD), following a first procedure of ULR muscle recession for small-angle XT. Recession of the lateral rectus muscle ranged from 8 to 9 mm. The postoperative motor alignment and degree of exodrift were investigated after the first ULR muscle recession and the second ULR muscle recession in the same patients.
RESULTS
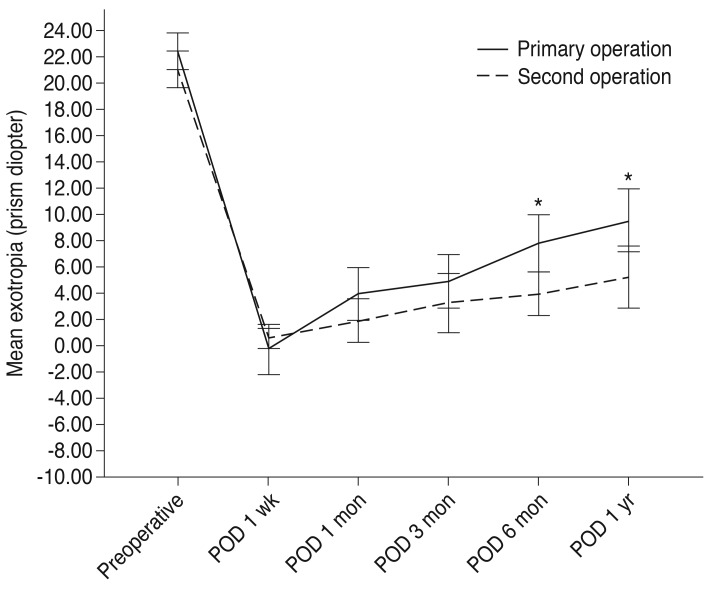
Observed differences in postoperative ocular alignment between the first ULR muscle recession and the second ULR muscle recession were statistically significant at follow-up periods of six months (7.84 +/- 4.43 vs. 3.89 +/- 3.47 PD), one year (9.58 +/- 4.97 vs. 5.21 +/- 4.94 PD), and at a final follow-up (21.11 +/- 2.98 vs. 7.52 +/- 4.06 PD) after surgery (p = 0.006, 0.013, and 0.000). Postoperative exodrift was statistically different between the first and second ULR muscle recessions at three to six months (2.89 +/-3.75 vs. 0.63 +/- 3.45 PD) and one year to final follow-up (11.52 +/- 5.50 vs. 2.32 +/- 3.53 PD) (p = 0.034 and 0.000). All of the first ULR muscle recession patients showed XT with deviation angles of more than 15 PD at the final follow-up. Regardless, the surgical success rate (<8 PD) after the second ULR recession was 63.16% (12 patients) among the total amount of patients with recurrent XT.
CONCLUSIONS
This study shows that changes in exodrift after a second ULR muscle recession are less than changes after the first URL muscle recession among patients with recurrent XT. A second ULR muscle recession may be a useful surgery for small-angle XT patients with deviation angles of 25 PD or less after a first ULR muscle recession.
MeSH Terms
Figure
Reference
-
1. Pukrushpan P, Isenberg SJ. Drift of ocular alignment following strabismus surgery. Part 1: using fixed scleral sutures. Br J Ophthalmol. 2009; 93:439–442. PMID: 18617540.
Article2. Weakley DR Jr, Stager DR. Unilateral lateral rectus recessions in exotropia. Ophthalmic Surg. 1993; 24:458–460. PMID: 8351092.
Article3. Olitsky SE. Early and late postoperative alignment following unilateral lateral rectus recession for intermittent exotropia. J Pediatr Ophthalmol Strabismus. 1998; 35:146–148. PMID: 9627874.
Article4. Wang L, Nelson LB. One muscle strabismus surgery. Curr Opin Ophthalmol. 2010; 21:335–340. PMID: 20531188.
Article5. Spierer O, Spierer A, Glovinsky J, Ben-Simon GJ. Moderate-angle exotropia: a comparison of unilateral and bilateral rectus muscle recession. Ophthalmic Surg Lasers Imaging. 2010; 41:355–359. PMID: 20507021.
Article6. Deutsch JA, Nelson LB, Sheppard RW, Burke MJ. Unilateral lateral rectus recession for the treatment of exotropia. Ann Ophthalmol. 1992; 24:111–113. PMID: 1570925.7. Sohn JH, Chang BL. Management for reoperation in recurrent exotropia. J Korean Ophthalmol Soc. 1994; 35:580–584.8. Wolff SM, Loupe DN. In : Campos EC, editor. Binocularity after surgery for intermittent exotropia. Strabismus and ocular motility disorder: proceedings of the 6th meeting of the International Strabismological Association; 1990; Surfers Paradise, Australia. Hampshire: Macmillan Press;1990. p. 375.9. von Noorden GK. Some aspects of exotropia. In : Proceedings of Wilmer Resident's Association Meeting; 1966; Baltimore, USA. Baltimore: Wilmer Resident's Association;1966.10. Kim SJ, Lee WS. Clinical analysis of surgical results in exodeviation. J Korean Ophthalmol Soc. 1992; 33:724–732.11. Jeong TS, You IC, Park SW, Park YG. Factors of surgical success with unilateral recession and resection in intermittent exotropia. J Korean Ophthalmol Soc. 2006; 47:1987–1992.12. Wang L, Nelson LB. Outcome study of unilateral lateral rectus recession for small to moderate angle intermittent exotropia in children. J Pediatr Ophthalmol Strabismus. 2010; 47:242–247. PMID: 19873943.
Article13. Lee K, Shin KS, Kim Y, Choi MY. Comparison of outcomes of unilateral lateral rectus recession for exotropia between first and second operations. Korean J Ophthalmol. 2011; 25:329–333. PMID: 21976940.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Analysis after Reoperation for Recurrent Intermittent Exotropia
- Comparison of Exodrift between Natural Group and Postoperative Group in Intermittent Exotropia Patients
- Comparison of Surgical Results Between Bilateral Recession and Unilateral Resection-Recession in Intermittent Exotropia
- Surgical Results in Basic Exotropia of Moderate Degree
- Postoperative Exodrift Patterns after Bilateral or Unilateral Lateral Rectus Recession in 20 Prism-diopter Intermittent Exotropia