J Periodontal Implant Sci.
2018 Feb;48(1):3-11. 10.5051/jpis.2018.48.1.3.
Trends in the utilization of dental outpatient services affected by the expansion of health care benefits in South Korea to include scaling: a 6-year interrupted time-series study
- Affiliations
-
- 1Department of Dental Hygiene, Kangwon National University College of Health Science, Samcheok, Korea.
- 2Department of Health Policy and Management, Korea University College of Health Sciences, Seoul, Korea. junhlee@korea.ac.kr
- 3BK21 PLUS Program in Embodiment: Health-Society Interaction, Department of Public Health Sciences, Korea University Graduate School, Seoul, Korea.
- 4Department of Periodontology, Seoul National University School of Dentistry, Seoul, Korea.
- KMID: 2405405
- DOI: http://doi.org/10.5051/jpis.2018.48.1.3
Abstract
- PURPOSE
This study utilized a strong quasi-experimental design to test the hypothesis that the implementation of a policy to expand dental care services resulted in an increase in the usage of dental outpatient services.
METHODS
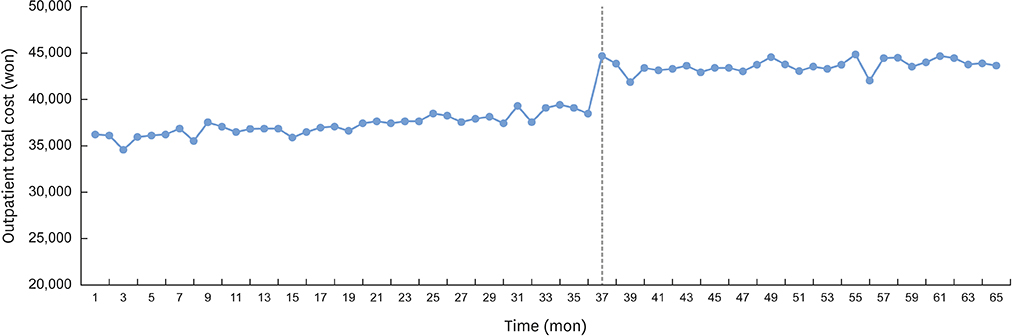
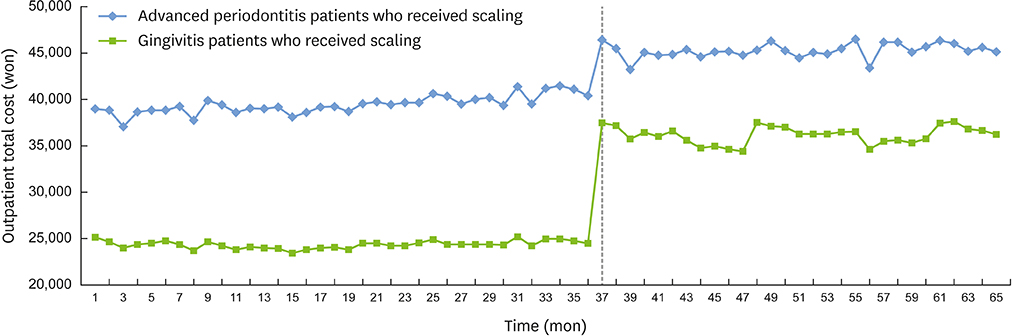
A total of 45,650,000 subjects with diagnoses of gingivitis or advanced periodontitis who received dental scaling were selected and examined, utilizing National Health Insurance claims data from July 2010 through November 2015. We performed a segmented regression analysis of the interrupted time-series to analyze the time-series trend in dental costs before and after the policy implementation, and assessed immediate changes in dental costs.
RESULTS
After the policy change was implemented, a statistically significant 18% increase occurred in the observed total dental cost per patient, after adjustment for age, sex, and residence area. In addition, the dental costs of outpatient gingivitis treatment increased immediately by almost 47%, compared with a 15% increase in treatment costs for advanced periodontitis outpatients. This policy effect appears to be sustainable.
CONCLUSIONS
The introduction of the new policy positively impacted the immediate and long-term outpatient utilization of dental scaling treatment in South Korea. While the policy was intended to entice patients to prevent periodontal disease, thus benefiting the insurance system, our results showed that the policy also increased treatment accessibility for potential periodontal disease patients and may improve long-term periodontal health in the South Korean population.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of scaling rate data of Community Health Survey and National Health Insurance Service
Young-Eun Jang, Kang-Ju Son, Chun-Bae Kim, Nam-Hee Kim
J Korean Acad Oral Health. 2019;43(1):26-32. doi: 10.11149/jkaoh.2019.43.1.26.
Reference
-
1. Korean Statistical Information Service. Outpatient disease statistics [Internet]. Daejeon: Statistics Korea;2016. cited 2016 Jun 26. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=350&tblId=DT_35007_N149&conn_path=I2.2. Lee MY, Chang SJ, Kim CB, Chung WG, Choi EM, Kim NH. Community periodontal treatment needs in South Korea. Int J Dent Hyg. 2015; 13:254–260.
Article3. Park HJ, Lee JH, Park S, Kim TI. Changes in dental care access upon health care benefit expansion to include scaling. J Periodontal Implant Sci. 2016; 46:405–414.
Article4. Lee JH, Oh JY, Choi JK, Kim YT, Park YS, Jeong SN, et al. Trends in the incidence of tooth extraction due to periodontal disease: results of a 12-year longitudinal cohort study in South Korea. J Periodontal Implant Sci. 2017; 47:264–272.
Article5. Jang YE, Kim CB, Kim NH. Utilization of preventive dental services before and after health insurance covered dental scaling in Korea. Asia Pac J Public Health. 2017; 29:70–80.
Article6. Lee JH, Lee JS, Choi JK, Kweon HI, Kim YT, Choi SH. National dental policies and socio-demographic factors affecting changes in the incidence of periodontal treatments in Korean: a nationwide population-based retrospective cohort study from 2002–2013. BMC Oral Health. 2016; 16:118.
Article7. Singhal A, Caplan DJ, Jones MP, Momany ET, Kuthy RA, Buresh CT, et al. Eliminating medicaid adult dental coverage in California led to increased dental emergency visits and associated costs. Health Aff (Millwood). 2015; 34:749–756.
Article8. Pande AH, Ross-Degnan D, Zaslavsky AM, Salomon JA. Effects of healthcare reforms on coverage, access, and disparities: quasi-experimental analysis of evidence from Massachusetts. Am J Prev Med. 2011; 41:1–8.9. Wagner AK, Soumerai SB, Zhang F, Ross Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002; 27:299–309.
Article10. Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999; 4:1–6.
Article11. Han E, Chae SM, Kim NS, Park S. Effects of pharmaceutical cost containment policies on doctors' prescribing behavior: focus on antibiotics. Health Policy. 2015; 119:1245–1254.
Article12. Decker SL, Lipton BJ. Do medicaid benefit expansions have teeth? The effect of medicaid adult dental coverage on the use of dental services and oral health. J Health Econ. 2015; 44:212–225.
Article13. Choi MK. The impact of Medicaid insurance coverage on dental service use. J Health Econ. 2011; 30:1020–1031.
Article14. Nasseh K, Vujicic M. The impact of medicaid reform on children's dental care utilization in Connecticut, Maryland, and Texas. Health Serv Res. 2015; 50:1236–1249.
Article15. Buchwald S, Kocher T, Biffar R, Harb A, Holtfreter B, Meisel P. Tooth loss and periodontitis by socio-economic status and inflammation in a longitudinal population-based study. J Clin Periodontol. 2013; 40:203–211.
Article16. Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005; 366:1809–1820.
Article17. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2015: Korea National Health and Nutrition Examination Survey (KNHANES VI-3). Cheongju: Korea Centers for Disease Control and Prevention;2016.18. Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH. Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes. 2010; 8:126.
Article19. Gift HC, Atchison KA, Dayton CM. Conceptualizing oral health and oral health-related quality of life. Soc Sci Med. 1997; 44:601–608.
Article20. Bernabé E, Marcenes W. Periodontal disease and quality of life in British adults. J Clin Periodontol. 2010; 37:968–972.
Article21. Matuliene G, Studer R, Lang N, Schmidlin K, Pjetursson B, Salvi G, et al. Significance of periodontal risk assessment in the recurrence of periodontitis and tooth loss. J Clin Periodontol. 2010; 37:191–199.
Article22. Worthington HV, Clarkson JE, Bryan G, Beirne PV. Routine scale and polish for periodontal health in adults. Cochrane Database Syst Rev. 2013; CD004625.
Article23. Andersen RM, Davidson PL. Ethnicity, aging, and oral health outcomes: a conceptual framework. Adv Dent Res. 1997; 11:203–209.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in dental care access upon health care benefit expansion to include scaling
- Evaluation of the effectiveness of the policy to expand the scope of national health insurance dental scaling service benefits
- The Effect of Outpatient Cost Sharing on Health Care Utilization of the Elderly
- Current and Future Trends in Hospital Utilization of Patients With Schizophrenia in Korea: A Time Series Analysis Using National Health Insurance Data
- Disparities in High-cost Outpatient Imaging Test Utilization between Private Health Insurance Subscribers and Non-subscribers: Changes Following the National Health Insurance Benefit Expansion Policy