Ann Hepatobiliary Pancreat Surg.
2016 Nov;20(4):191-196. 10.14701/ahbps.2016.20.4.191.
Effect of polylactic film (Surgi-Wrap) on preventing postoperative ileus after major hepato-pancreato-biliary surgery
- Affiliations
-
- 1Department of Surgery, Dongguk University College of Medicine, Goyang, Korea. cardioman76@gmail.com
- KMID: 2362470
- DOI: http://doi.org/10.14701/ahbps.2016.20.4.191
Abstract
- BACKGROUNDS/AIMS
Major hepato-pancreato-biliary (HPB) surgery is usually performed via an open method rather than a laparoscopic method. Postoperative ileus (POI) is a classic complication after open surgery. The purpose of this study was to determine whether polylactic film is useful in the prevention of POI.
METHODS
A total of 179 patients who underwent major HPB surgery between 2005 and 2014, were retrospectively reviewed. A diagnosis of POI was made by a physical examination, laboratory, and radiological findings. Surgi-Wrap® polylactic film was preferentially used intraperitoneally by surgeons, just before wound closure.
RESULTS
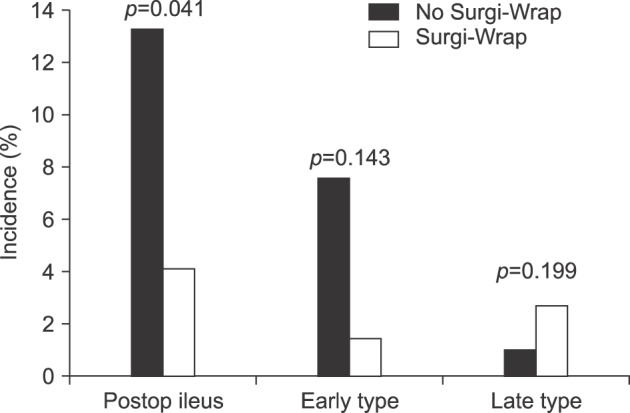
Major HPB surgery included pancreatoduodenectomy (n=48), distal or subtotal pancreatectomy (n=24), hepatectomy (n=67), other bile duct or gallbladder operations (n=35), and others (n=5). Although patients with polylactic film showed a significantly lower incidence of POI (n=3, 4.1% vs. n=14, 13.3%, p=0.041), they showed a significantly higher complication rate (n=20, 27.0% vs. n=19, 18.1%, p=0.004), particularly intra-abdominal fluid collection (n=7, 9.4% vs. n=2, 1.9%), and wound infections (n=6, 8.1% vs. n=3, 2.9%), than those who did not receive the film, respectively.
CONCLUSIONS
Although the polylactic film prevented POI, more complications other than POI were observed. Well-designed randomized controlled trials, using this anti-adhesive product, are needed to evaluate its effect on POI after major HPB surgery.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Metformin-loaded Citric Acid Cross-linked Agarose Films in the Prevention of Postoperative Abdominal Adhesion
Ji Hyun Moon, Jong Ho Park, Nak Song Sung, Young Gil Jeong, Ki Chang Song, Jong Pil Ahn, Nam-Seob Lee, Seung Yun Han, Ji Heun Jeong
Anat Biol Anthropol. 2019;32(4):129-139. doi: 10.11637/aba.2019.32.4.129.
Reference
-
1. Mattei P, Rombeau JL. Review of the pathophysiology and management of postoperative ileus. World J Surg. 2006; 30:1382–1391. PMID: 16850151.
Article2. Weibel MA, Majno G. Peritoneal adhesions and their relation to abdominal surgery. A postmortem study. Am J Surg. 1973; 126:345–353. PMID: 4580750.3. Menzies D, Ellis H. Intestinal obstruction from adhesions--how big is the problem? Ann R Coll Surg Engl. 1990; 72:60–63. PMID: 2301905.4. Robb WB, Mariette C. Strategies in the prevention of the formation of postoperative adhesions in digestive surgery: a systematic review of the literature. Dis Colon Rectum. 2014; 57:1228–1240. PMID: 25203381.5. Lee AL, Kim CB. The effect of erythromycin on gastrointestinal motility in subtotal gastrectomized patients. J Korean Surg Soc. 2012; 82:149–155. PMID: 22403748.
Article6. Ay AA, Kutun S, Ulucanlar H, Tarcan O, Demir A, Cetin A. Risk factors for postoperative ileus. J Korean Surg Soc. 2011; 81:242–249. PMID: 22111079.
Article7. Vather R, Trivedi S, Bissett I. Defining postoperative ileus: results of a systematic review and global survey. J Gastrointest Surg. 2013; 17:962–972. PMID: 23377782.
Article8. Beck DE, Cohen Z, Fleshman JW, Kaufman HS, van Goor H, Wolff BG. A prospective, randomized, multicenter, controlled study of the safety of Seprafilm adhesion barrier in abdominopelvic surgery of the intestine. Dis Colon Rectum. 2003; 46:1310–1319. PMID: 14530667.
Article9. Zeng Q, Yu Z, You J, Zhang Q. Efficacy and safety of Seprafilm for preventing postoperative abdominal adhesion: systematic review and meta-analysis. World J Surg. 2007; 31:2125–2131. PMID: 17899250.
Article10. Brochhausen C, Schmitt VH, Planck CN, Rajab TK, Hollemann D, Tapprich C, et al. Current strategies and future perspectives for intraperitoneal adhesion prevention. J Gastrointest Surg. 2012; 16:1256–1274. PMID: 22297658.
Article11. Kim JY, Cho WJ, Kim JH, Lim SH, Kim HJ, Lee YW, et al. Efficacy and safety of hyaluronate membrane in the rabbit cecum-abdominal wall adhesion model. J Korean Surg Soc. 2013; 85:51–57. PMID: 23908960.
Article12. Becker JM, Dayton MT, Fazio VW, Beck DE, Stryker SJ, Wexner SD, et al. Prevention of postoperative abdominal adhesions by a sodium hyaluronate-based bioresorbable membrane: a prospective, randomized, double-blind multicenter study. J Am Coll Surg. 1996; 183:297–306. PMID: 8843257.13. Diamond MP. Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL-F): a blinded, prospective, randomized, multicenter clinical study. Seprafilm Adhesion Study Group. Fertil Steril. 1996; 66:904–910. PMID: 8941053.14. Cohen Z, Senagore AJ, Dayton MT, Koruda MJ, Beck DE, Wolff BG, et al. Prevention of postoperative abdominal adhesions by a novel, glycerol/sodium hyaluronate/carboxymethylcellulose-based bioresorbable membrane: a prospective, randomized, evaluator-blinded multicenter study. Dis Colon Rectum. 2005; 48:1130–1139. PMID: 15868230.
Article15. Fazio VW, Cohen Z, Fleshman JW, van Goor H, Bauer JJ, Wolff BG, et al. Reduction in adhesive small-bowel obstruction by Seprafilm adhesion barrier after intestinal resection. Dis Colon Rectum. 2006; 49:1–11. PMID: 16320005.
Article16. Mabrut JY, Favre JP, Desrousseaux B, Chipponi J, Arnaud JP, Domergue J, et al. Safety and long-term outcome of a new concept for surgical adhesion-reduction strategies (Prevadh): a prospective, multicenter study. Hepatogastroenterology. 2008; 55:517–521. PMID: 18613399.17. Park CM, Lee WY, Cho YB, Yun HR, Lee WS, Yun SH, et al. Sodium hyaluronate-based bioresorbable membrane (Seprafilm) reduced early postoperative intestinal obstruction after lower abdominal surgery for colorectal cancer: the preliminary report. Int J Colorectal Dis. 2009; 24:305–310. PMID: 18953549.
Article18. van der Wal JB, Iordens GI, Vrijland WW, van Veen RN, Lange J, Jeekel J. Adhesion prevention during laparotomy: long-term follow-up of a randomized clinical trial. Ann Surg. 2011; 253:1118–1121. PMID: 21502860.19. Canis MJ, Triopon G, Daraï E, Madelenat P, LeVêque J, Panel P, et al. Adhesion prevention after myomectomy by laparotomy: a prospective multicenter comparative randomized single-blind study with second-look laparoscopy to assess the effectiveness of PREVADH™. Eur J Obstet Gynecol Reprod Biol. 2014; 178:42–47. PMID: 24841647.
Article20. Yamaoka T, Takahashi Y, Fujisato T, Lee CW, Tsuji T, Ohta T, et al. Novel adhesion prevention membrane based on a bioresorbable copoly(ester-ether) comprised of poly-L-lactide and Pluronic: in vitro and in vivo evaluations. J Biomed Mater Res. 2001; 54:470–479. PMID: 11426591.21. Avital S, Bollinger TJ, Wilkinson JD, Marchetti F, Hellinger MD, Sands LR. Preventing intra-abdominal adhesions with polylactic acid film: an animal study. Dis Colon Rectum. 2005; 48:153–157. PMID: 15690673.
Article22. Gruber-Blum S, Petter-Puchner AH, Brand J, Fortelny RH, Walder N, Oehlinger W, et al. Comparison of three separate anti-adhesive barriers for intraperitoneal onlay mesh hernia repair in an experimental model. Br J Surg. 2011; 98:442–449. PMID: 21254024.
Article23. Schreiber C, Boening A, Kostolny M, Pines E, Cremer J, Lange R, et al. European clinical experience with REPEL-CV. Expert Rev Med Devices. 2007; 4:291–295. PMID: 17488223.
Article24. Artinyan A, Nunoo-Mensah JW, Balasubramaniam S, Gauderman J, Essani R, Gonzalez-Ruiz C, et al. Prolonged postoperative ileus-definition, risk factors, and predictors after surgery. World J Surg. 2008; 32:1495–1500. PMID: 18305994.
Article25. Hayashi S, Takayama T, Masuda H, Kochi M, Ishii Y, Matsuda M, et al. Bioresorbable membrane to reduce postoperative small bowel obstruction in patients with gastric cancer: a randomized clinical trial. Ann Surg. 2008; 247:766–770. PMID: 18438113.26. Park JH, Jeong SH, Lee YJ, Choi SK, Hong SC, Jung EJ, et al. Current status of the use of antiadhesive agents for gastric cancer surgery: a questionnaire survey in South Korea. J Korean Surg Soc. 2013; 84:160–167. PMID: 23487148.
Article27. Park CS, Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, et al. A comparative study regarding the effect of an intraperitoneal anti-adhesive agent application in left-liver living donors. Korean J Hepatobiliary Pancreat Surg. 2014; 18:26–28. PMID: 26155243.
Article28. White TJ, Santos MC, Thompson JS. Factors affecting wound complications in repair of ventral hernias. Am Surg. 1998; 64:276–280. PMID: 9520825.29. Park JS, Lee DH, Jang JY, Han Y, Yoon DS, Kim JK, et al. Use of TachoSil(®) patches to prevent pancreatic leaks after distal pancreatectomy: a prospective, multicenter, randomized controlled study. J Hepatobiliary Pancreat Sci. 2016; 23:110–117. PMID: 26681272.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Polylactide Resorbable Film on the Epidural Fibrosis After Lumbar Laminotomy
- Surgical management of the postoperative complications of hepato-pancreato-biliary surgery
- Comparison of Single-Incision Robotic Cholecystectomy, Single-Incision Laparoscopic Cholecystectomy and 3-Port Laparoscopic Cholecystectomy -Postoperative Pain, Cosmetic Outcome and Surgeon's Workload
- Extracapsular excision of hepatic hemangioma: A single centre experience
- Safety and Feasibility of Single Incision Laparoscopic Spleen Preserving Distal Pancreatectomy