Clin Exp Otorhinolaryngol.
2016 Dec;9(4):346-351. 10.21053/ceo.2015.01984.
Upper Airway Variation and Frequent Alcohol Consumption Can Affect Compliance With Continuous Positive Airway Pressure
- Affiliations
-
- 1Department of Otolaryngology, Keimyung University School of Medicine, Daegu, Korea.
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. siamkhy@gmail.com
- KMID: 2360766
- DOI: http://doi.org/10.21053/ceo.2015.01984
Abstract
OBJECTIVES
Compliance with continuous positive airway pressure (CPAP) treatment remains a primary concern for improving treatment outcomes of obstructive sleep apnea. There are few studies that have considered the role of upper airway anatomy on the compliance with CPAP. We hypothesized that upper airway anatomy would influence the compliance with CPAP.
METHODS
One hundred out of 161 consecutive patients were enrolled in this study. The following possible determinants were tested against CPAP use: demographic and anthropometric data, minimal cross-sectional area on acoustic rhinometry, cephalometric and polysomnographic data, questionnaires of Epworth sleepiness scale and Beck depression index, and histories of previous upper airway surgery, degree of nasal obstruction, daily cigarette consumption, and weekly frequency of alcohol intake.
RESULTS
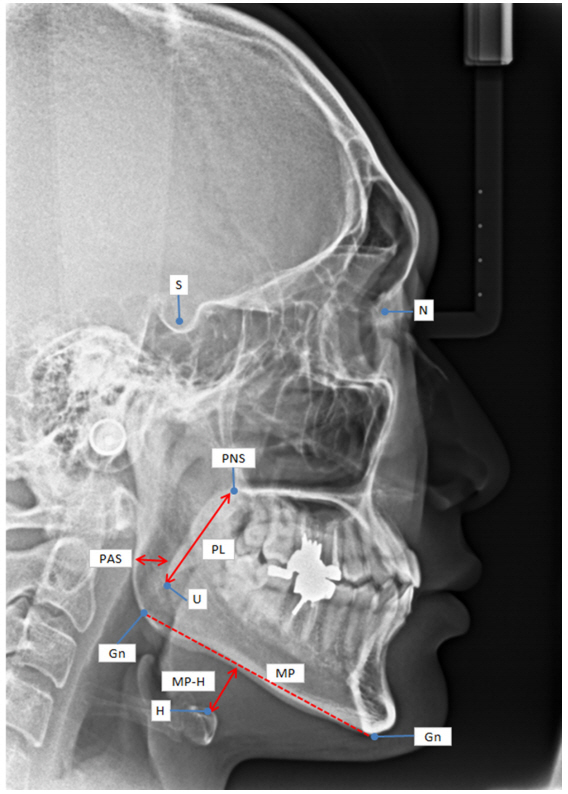
Univariate analysis showed that histories of previous upper airway surgery and less frequent alcohol consumption, and longer mandibular plane-hyoid length (MP-H) on cephalometry were associated with longer average daily CPAP use. After adjustment for the confounding factors with multiple linear regression analysis, alcohol consumption and MP-H were still associated with the compliance with CPAP significantly.
CONCLUSION
To improve compliance with CPAP, careful evaluations of upper airway problems and life style are important before initiating CPAP.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim J, In K, Kim J, You S, Kang K, Shim J, et al. Prevalence of sleepdisordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004; Nov. 170(10):1108–13.
Article2. Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006; Mar. 29(3):375–80.
Article3. Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006; Jul. (3):CD001106.4. Indications and standards for use of nasal continuous positive airway pressure (CPAP) in sleep apnea syndromes. American Thoracic Society. Official statement adopted March 1944. Am J Respir Crit Care Med. 1994; Dec. 150(6 Pt 1):1738–45.5. Alves C, Caminha JM, da Silva AM, Mendonca D. Compliance to continuous positive airway pressure therapy in a group of Portuguese patients with obstructive sleep apnea syndrome. Sleep Breath. 2012; Jun. 16(2):555–62.
Article6. Bakker JP, Marshall NS. Flexible pressure delivery modification of continuous positive airway pressure for obstructive sleep apnea does not improve compliance with therapy: systematic review and meta-analysis. Chest. 2011; Jun. 139(6):1322–30.7. Zozula R, Rosen R. Compliance with continuous positive airway pressure therapy: assessing and improving treatment outcomes. Curr Opin Pulm Med. 2001; Nov. 7(6):391–8.
Article8. Friedman M, Ibrahim H, Joseph NJ. Staging of obstructive sleep apnea/hypopnea syndrome: a guide to appropriate treatment. Laryngoscope. 2004; Mar. 114(3):454–9.
Article9. Kim HY, Min JY, Cho DY, Chung SK, Dhong HJ. Influence of upper airway narrowing on the effective continuous positive airway pressure level. Laryngoscope. 2007; Jan. 117(1):82–5.
Article10. Kim HY, Dhong HJ, Hong SD, Lee HJ, Cho HJ, Chung SK. Paradoxical nasal obstruction: analysis of characteristics using acoustic rhinometry. Am J Rhinol. 2007; Jul-Aug. 21(4):408–11.
Article11. Friedman M, Soans R, Joseph N, Kakodkar S, Friedman J. The effect of multilevel upper airway surgery on continuous positive airway pressure therapy in obstructive sleep apnea/hypopnea syndrome. Laryngoscope. 2009; Jan. 119(1):193–6.
Article12. Li HY, Wang PC, Chen YP, Lee LA, Fang TJ, Lin HC. Critical appraisal and meta-analysis of nasal surgery for obstructive sleep apnea. Am J Rhinol Allergy. 2011; Jan-Feb. 25(1):45–9.
Article13. Sufioglu M, Ozmen OA, Kasapoglu F, Demir UL, Ursavas A, Erisen L, et al. The efficacy of nasal surgery in obstructive sleep apnea syndrome: a prospective clinical study. Eur Arch Otorhinolaryngol. 2012; Feb. 269(2):487–94.
Article14. Bachour A, Maasilta P. Mouth breathing compromises adherence to nasal continuous positive airway pressure therapy. Chest. 2004; Oct. 126(4):1248–54.
Article15. Friedman M, Tanyeri H, Lim JW, Landsberg R, Vaidyanathan K, Caldarelli D. Effect of improved nasal breathing on obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000; Jan. 122(1):71–4.
Article16. Han F, Song W, Li J, Zhang L, Dong X, He Q. Influence of UPPP surgery on tolerance to subsequent continuous positive airway pressure in patients with OSAHS. Sleep Breath. 2006; Mar. 10(1):37–42.
Article17. Mortimore IL, Bradley PA, Murray JA, Douglas NJ. Uvulopalatopharyngoplasty may compromise nasal CPAP therapy in sleep apnea syndrome. Am J Respir Crit Care Med. 1996; Dec. 154(6 Pt 1):1759–62.
Article18. Chandrashekariah R, Shaman Z, Auckley D. Impact of upper airway surgery on CPAP compliance in difficult-to-manage obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2008; Sep. 134(9):926–30.
Article19. Hong SD, Kim HY, Cho HJ, Jang MS, Dhong HJ, Chung SK. Effect of uvulopalatopharyngoplasty on CPAP compliance. Eur Arch Otorhinolaryngol. 2015; Jun. 272(6):1437–42.
Article20. Eccles R, Tolley NS. The effect of alcohol ingestion upon nasal airway resistance. Rhinology. 1987; Dec. 25(4):245–8.21. Mitler MM, Dawson A, Henriksen SJ, Sobers M, Bloom FE. Bedtime ethanol increases resistance of upper airways and produces sleep apneas in asymptomatic snorers. Alcohol Clin Exp Res. 1988; Dec. 12(6):801–5.
Article22. Series F, Cormier FY, Desmeules M. Alcohol and the response of upper airway resistance to a changing respiratory drive in normal man. Respir Physiol. 1990; Aug. 81(2):153–63.23. McArdle N, Devereux G, Heidarnejad H, Engleman HM, Mackay TW, Douglas NJ. Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1999; Apr. 159(4 Pt 1):1108–14.
Article24. Russo-Magno P, O’Brien A, Panciera T, Rounds S. Compliance with CPAP therapy in older men with obstructive sleep apnea. J Am Geriatr Soc. 2001; Sep. 49(9):1205–11.
Article25. Wild MR, Engleman HM, Douglas NJ, Espie CA. Can psychological factors help us to determine adherence to CPAP? A prospective study. Eur Respir J. 2004; Sep. 24(3):461–5.
Article26. Kim SJ, Choi JH, Kim EJ, Lee SK, Lee SH, Jun YJ, et al. A prospective population-based study of total nasal resistance in Korean subjects. Clin Exp Otorhinolaryngol. 2012; Mar. 5(1):39–43.
Article27. Bollig SM. Encouraging CPAP adherence: it is everyone’s job. Respir Care. 2010; Sep. 55(9):1230–9.28. Ball EM, Banks MB. Determinants of compliance with nasal continuous positive airway pressure treatment applied in a community setting. Sleep Med. 2001; May. 2(3):195–205.
Article29. Lewis KE, Seale L, Bartle IE, Watkins AJ, Ebden P. Early predictors of CPAP use for the treatment of obstructive sleep apnea. Sleep. 2004; Feb. 27(1):134–8.
Article30. Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002; Feb. 121(2):430–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improving Compliance for Continuous Positive Airway Pressure Compliance and Possible Influencing Factors
- Treatment of Obstructive Sleep Apnea with Positive Pressure Ventilation
- The Impact of Depressive Symptom on Efficacy and Compliance of Positive Airway Pressure in Obstructive Sleep Apnea
- Effectiveness of applying continuous positive airway pressure in a patient with paradoxical vocal fold movement after endotracheal extubation: a case report
- Two Cases of Postobstructive Pulmonary Edema