Anesth Pain Med.
2016 Oct;11(4):375-379. 10.17085/apm.2016.11.4.375.
Optimal transducer levels for central venous pressure and pulmonary artery occlusion pressure monitoring in supine and prone positions in pediatric patients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea. jintae73@gmail.com
- KMID: 2358334
- DOI: http://doi.org/10.17085/apm.2016.11.4.375
Abstract
- BACKGROUND
This study was performed to investigate optimal central venous pressure (CVP) or pulmonary artery occlusion pressure (PAOP) transducer levels in supine and prone positions in pediatric patients.
METHODS
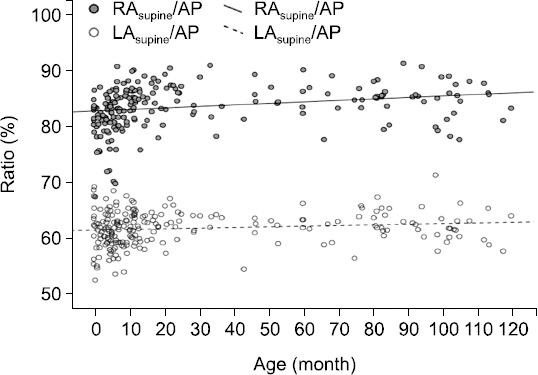
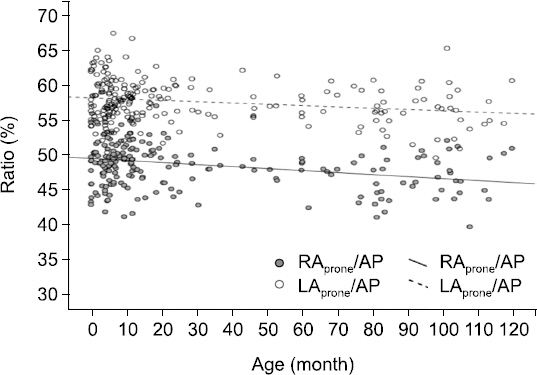
Chest tomography images of 213 children aged ≤ 10 years were reviewed. Distances from the back to the uppermost blood level of both atria and their ratios to the largest anteroposterior (AP) diameter of the thorax were calculated for the supine position. For the prone position, same distances and ratios were calculated from the anterior chest. Subgroup analysis was performed to evaluate if there were significant differences in each ratio according to age.
RESULTS
In the supine position, the ratio of the uppermost blood level of the right atrium (RA) and left atrium (LA) to the largest AP diameter of the thorax was 80-85% and 60-65%, respectively. The ratio of the most posterior blood level of the RA and LA to largest AP diameter of thorax was 45-50% and 55-60%, respectively, from the anterior chest in the prone position. Subgroup differences in each ratio were within the range of 5%.
CONCLUSIONS
In pediatric patients, CVP and PAOP transducers should be differently placed according to supine and prone positions. The influence of age was minimal on the level of each transducer.
Keyword
MeSH Terms
Figure
Reference
-
1. Courtois M, Fattal PG, Kovács SJ Jr, Tiefenbrunn AJ, Ludbrook PA. Anatomically and physiologically based reference level for measurement of intracardiac pressures. Circulation. 1995; 92:1994–2000. DOI: 10.1161/01.CIR.92.7.1994. PMID: 7671382.
Article2. Mueller HS, Chatterjee K, Davis KB, Fifer MA, Franklin C, Greenberg MA, et al. ACC expert consensus document. Present use of bedside right heart catheterization in patients with cardiac disease. American College of Cardiology. J Am Coll Cardiol. 1998; 32:840–64. DOI: 10.1016/S0735-1097(98)00327-1.3. Pittman JA, Ping JS, Mark JB. Arterial and central venous pressure monitoring. Int Anesthesiol Clin. 2004; 42:13–30. DOI: 10.1097/00004311-200404210-00004. PMID: 14716195.
Article4. Figg KK, Nemergut EC. Error in central venous pressure measurement. Anesth Analg. 2009; 108:1209–11. DOI: 10.1213/ane.0b013e318196482c. PMID: 19299788.
Article5. Kee LL, Simonson JS, Stotts NA, Skov P, Schiller NB. Echocardiographic determination of valid zero reference levels in supine and lateral positions. Am J Crit Care. 1993; 2:72–80. PMID: 8353583.
Article6. Kovacs G, Avian A, Olschewski A, Olschewski H. Zero reference level for right heart catheterisation. Eur Respir J. 2013; 42:1586–94. DOI: 10.1183/09031936.00050713. PMID: 23794468.
Article7. Seo JH, Jung CW, Bahk JH. Uppermost blood levels of the right and left atria in the supine position: implication for measuring central venous pressure and pulmonary artery wedge pressure. Anesthesiology. 2007; 107:260–3. DOI: 10.1097/01.anes.0000270720.67307.fa. PMID: 17667570.8. Song IK, Park HS, Lee JH, Kim EH, Kim HS, Bahk JH, et al. Optimal level of the reference transducer for central venous pressure and pulmonary artery occlusion pressure monitoring in supine, prone, and sitting position. J Clin Monit Comput. 2016; Epub ahead of print. DOI: 10.1007/s10877-016-9864-2.
Article9. Chandraratna PA. Determination of zero reference level for left atrial pressure by echocardiography. Am Heart J. 1975; 89:159–62. DOI: 10.1016/0002-8703(75)90040-X.
Article10. Rauen CA, Makic MB, Bridges E. Evidence-based practice habits: transforming research into bedside practice. Crit Care Nurse. 2009; 29:46–59. DOI: 10.4037/ccn2009287. PMID: 19339447.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in the hemodynamic parameters between the prone and supine positions measured by an arterial pulse contour cardiac output monitoring system
- The changes of central venous pressure by body posture and positive end-expiratory pressure
- Change in Intraocular Pressure According to Sleeping Posture in Normal People
- Comparatives Study of Pulmonary Artery and Pulmonary Venous Wedge Pressure in Congenital Heart Disease
- Hydrothorax and Broken Catheters from Central Venous Catheterization