Anesth Pain Med.
2016 Oct;11(4):345-348. 10.17085/apm.2016.11.4.345.
Ultrasound-guided superficial cervical plexus block for carotid endarterectomy in a patient with Lemierre syndrome: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Jeju National University Hospital, Jeju, Korea.
- 2Department of Anesthesiology and Pain Medicine, Gachon University Gil Medical Center, Incheon, Korea. mikeum2@gilhospital.com
- KMID: 2358328
- DOI: http://doi.org/10.17085/apm.2016.11.4.345
Abstract
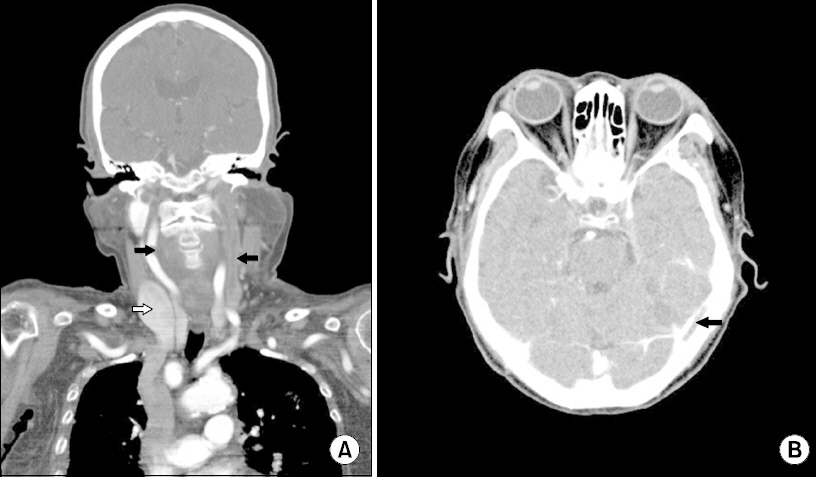
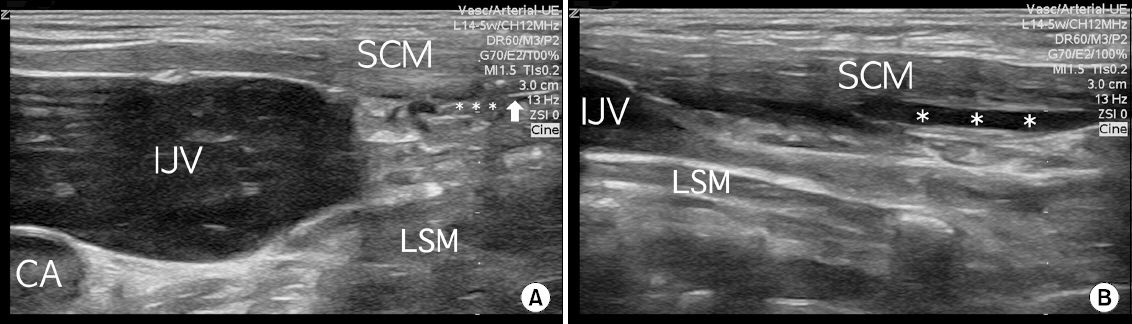
- A 70-year-old woman with an infectious thrombus in her left internal jugular vein (IJV) underwent carotid endarterectomy for stenosis and a highly movable plaque in her right carotid artery. She had been treated with antibiotics for four weeks before surgery due to Lemierre syndrome, a rare septic thrombophlebitis in the IJV secondary to an oropharyngeal infection. The right IJV was in a two-fold dilated state due to compensation for a thrombotic left IJV. Accordingly, superficial cervical plexus block was performed under ultrasound guidance to ensure safety and accuracy. During surgery, the alertness was maintained and the patient did not complain of pain in the absence of additional analgesics. No block-related complications were encountered. The authors report for the first time their regional anesthetic experiences in a patient with Lemierre syndrome.
MeSH Terms
Figure
Reference
-
1. Westhout F, Hasso A, Jalili M, Afghani B, Armstrong W, Nwagwu C, et al. Lemierre syndrome complicated by cavernous sinus thrombosis, the development of subdural empyemas, and internal carotid artery narrowing without cerebral infarction. Case report. J Neurosurg. 2007; 106(1 Suppl):53–6. PMID: 17233314.2. Chirinos JA, Lichtstein DM, Garcia J, Tamariz LJ. The evolution of Lemierre syndrome: report of 2 cases and review of the literature. Medicine (Baltimore). 2002; 81:458–65. DOI: 10.1097/00005792-200211000-00006.3. Syed MI, Baring D, Addidle M, Murray C, Adams C. Lemierre syndrome: two cases and a review. Laryngoscope. 2007; 117:1605–10. DOI: 10.1097/MLG.0b013e318093ee0e. PMID: 17762792.
Article4. Asnani J, Jones S. Case review. Lemierre's syndrome. J Fam Pract. 2014; 63:193–6. PMID: 24905121.5. Schubert AD, Hotz MA, Caversaccio MD, Arnold A. Septic thrombosis of the internal jugular vein: Lemierre's syndrome revisited. Laryngoscope. 2015; 125:863–8. DOI: 10.1002/lary.24995. PMID: 25387698.
Article6. Marulasiddappa V, Tejesh CA. Lemierre's syndrome presenting with septic shock. Indian J Crit Care Med. 2013; 17:382–4. DOI: 10.4103/0972-5229.123460. PMID: 24501493. PMCID: PMC3902576.
Article7. Herring AA, Stone MB, Frenkel O, Chipman A, Nagdev AD. The ultrasound-guided superficial cervical plexus block for anesthesia and analgesia in emergency care settings. Am J Emerg Med. 2012; 30:1263–7. DOI: 10.1016/j.ajem.2011.06.023. PMID: 22030184.
Article8. Zurawska U, Parasuraman S, Goldhaber SZ. Prevention of pulmonary embolism in general surgery patients. Circulation. 2007; 115:e302–7. DOI: 10.1161/CIRCULATIONAHA.106.674663. PMID: 17339555.
Article9. Guay J. Regional or general anesthesia for carotid endarterectomy? Evidence from published prospective and retrospective studies. J Cardiothorac Vasc Anesth. 2007; 21:127–32. DOI: 10.1053/j.jvca.2006.07.022. PMID: 17289496.
Article10. Schechter MA, Shortell CK, Scarborough JE. Regional versus general anesthesia for carotid endarterectomy: the American College of Surgeons National Surgical Quality Improvement Program perspective. Surgery. 2012; 152:309–14. DOI: 10.1016/j.surg.2012.05.008. PMID: 22749369.
Article11. Stoneham MD, Stamou D, Mason J. Regional anaesthesia for carotid endarterectomy. Br J Anaesth. 2015; 114:372–83. DOI: 10.1093/bja/aeu304. PMID: 25173766.
Article12. Sternbach Y, Illig KA, Zhang R, Shortell CK, Rhodes JM, Davies MG, et al. Hemodynamic benefits of regional anesthesia for carotid endarterectomy. J Vasc Surg. 2002; 35:333–9. DOI: 10.1067/mva.2002.121579. PMID: 11854732.
Article13. Yun SH, Park SH. Hyperacute hyperperfusion intracerebral hemorrhage complicating carotid endarterectomy. Anesth Pain Med. 2011; 6:357–61.14. Pandit JJ, Satya-Krishna R, Gration P. Superficial or deep cervical plexus block for carotid endarterectomy: a systematic review of complications. Br J Anaesth. 2007; 99:159–69. DOI: 10.1093/bja/aem160. PMID: 17576970.15. List F, Kessler P, Volk T. Regional anesthesia in patients with pre-existing infections or immunosuppression. Anaesthesist. 2013; 62:175–82. DOI: 10.1007/s00101-012-2097-y. PMID: 23515533.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthetic Management of Carotid Endarterectomy under Cervical Plexus Block
- Ultrasound-guided superficial cervical plexus block under dexmedetomidine sedation versus general anesthesia for carotid endarterectomy: a retrospective pilot study
- Bilateral variant locations of the musculocutaneous nerve during ultrasound-guided bilateral axillary brachial plexus block: A case report
- Ultrasound Guided Supraclavicular Brachial Plexus Block for Humerus Fracture in a Patient with Eisenmenger Syndrome
- A Comparison of Combined Superficial Cervical Plexus Block and Interscalene Brachial Plexus Block with General Anesthesia for Clavicle Surgery: Pilot Trial