Yeungnam Univ J Med.
2018 Jun;35(1):45-53. 10.12701/yujm.2018.35.1.45.
Ultrasound-guided superficial cervical plexus block under dexmedetomidine sedation versus general anesthesia for carotid endarterectomy: a retrospective pilot study
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, Pusan National University, School of Medicine, Busan, Korea. archo@pusan.ac.kr
- 2Department of Dental Anesthesia and Pain Medicine, Pusan National University Dental Hospital, Dental Research Institute, Yangsan, Korea.
- KMID: 2415733
- DOI: http://doi.org/10.12701/yujm.2018.35.1.45
Abstract
- BACKGROUND
Carotid endarterectomy (CEA) has been performed under regional and general anesthesia (GA). The general anesthesia versus local anesthesia for carotid surgery study compared the two techniques and concluded that there was no difference in perioperative outcomes. However, since this trial, new sedative agents have been introduced and devices that improve the delivery of regional anesthesia (RA) have been developed. The primary purpose of this pilot study was to compare intraoperative hemodynamic stability and postoperative outcomes between GA and ultrasound-guided superficial cervical plexus block (UGSCPB) under dexmedetomidine sedation for CEA.
METHODS
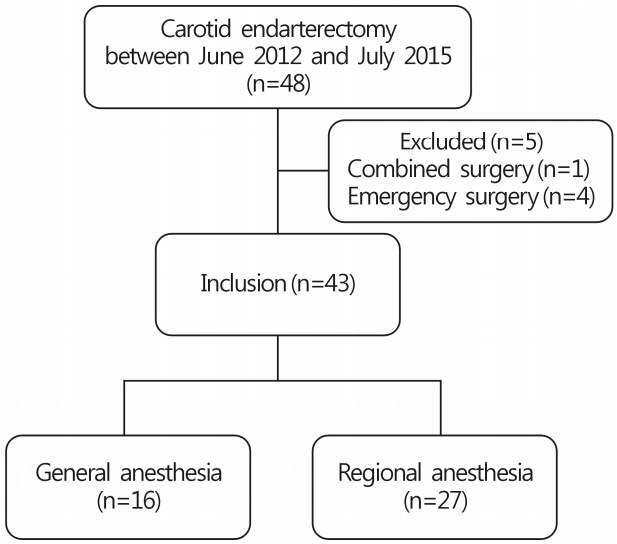
Medical records from 43 adult patients who underwent CEA were retrospectively reviewed, including 16 in the GA group and 27 in the RA group. GA was induced with propofol and maintained with sevoflurane. The UGSCPB was performed with ropivacaine under dexmedetomidine sedation. We compared the intraoperative requirement for vasoactive drugs, postoperative complications, pain scores using the numerical rating scale, and the duration of hospital stay.
RESULTS
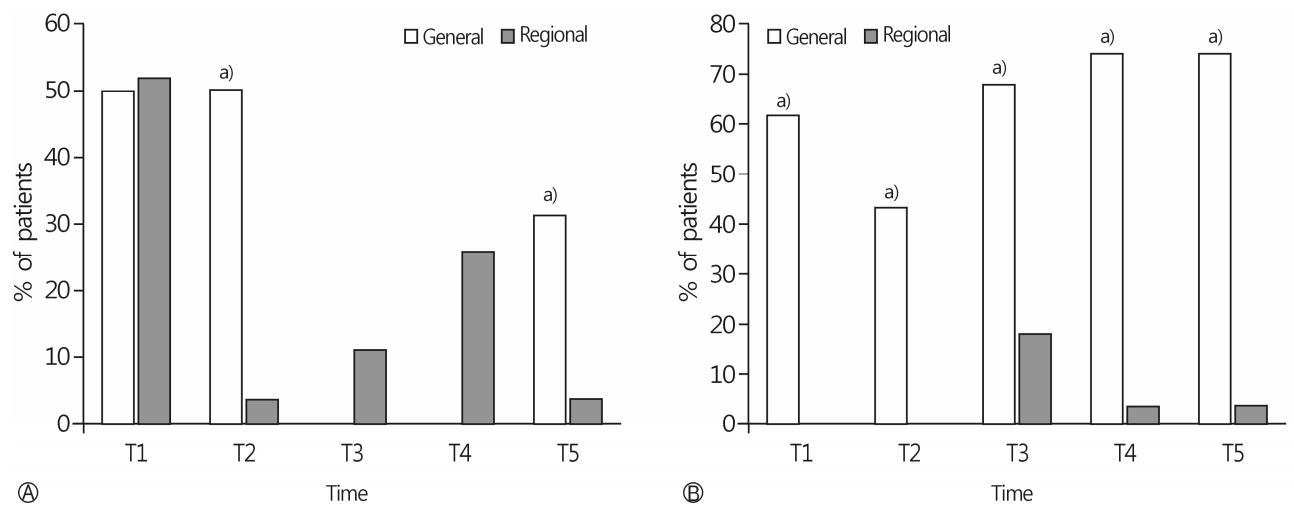
There was no difference between groups in the use of intraoperative antihypertensive drugs. However, intraoperative inotropic and vasopressor agents were more frequently required in the GA group (p < 0.0001). In the GA group, pain scores were significantly higher during the first 24 h after surgery (p < 0.0001 between 0-6 h, p < 0.004 between 6-12 h, and p < 0.001 between 12-24 h). The duration of hospital stay was significantly more in the GA group (13.3±4.6 days in the GA group vs. 8.5±2.4 days in the RA group, p < 0.001).
CONCLUSION
In this pilot study, intraoperative hemodynamic stability and postoperative outcomes were better in the RA compared to the GA group.
Keyword
MeSH Terms
-
Adult
Anesthesia, Conduction
Anesthesia, General*
Anesthesia, Local
Antihypertensive Agents
Cervical Plexus Block*
Cervical Plexus*
Dexmedetomidine*
Endarterectomy, Carotid*
Hemodynamics
Humans
Length of Stay
Medical Records
Pilot Projects*
Postoperative Complications
Propofol
Retrospective Studies*
Ultrasonography
Vasoconstrictor Agents
Antihypertensive Agents
Dexmedetomidine
Propofol
Vasoconstrictor Agents
Figure
Reference
-
1. GALA Trial Collaborative Group, Lewis SC, Warlow CP, Bodenham AR, Colam B, Rothwell PM, et al. General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet. 2008; 372:2132–42.
Article2. Guay J. Regional anesthesia for carotid surgery. Curr Opin Anaesthesiol. 2008; 21:638–44.
Article3. Martusevicius R, Swiatek F, Joergensen LG, Nielsen HB. Ultrasound-guided locoregional anaesthesia for carotid endarterectomy: a prospective observational study. Eur J Vasc Endovasc Surg. 2012; 44:27–30.
Article4. Sidorowicz M, Owczuk R, Kwiecińska B, Wujtewicz MA, Wojciechowski J, Wujtewicz M. Dexmedetomidine sedation for carotid endarterectomy. Anestezjol Intens Ter. 2009; 41:78–83.5. Bekker AY, Basile J, Gold M, Riles T, Adelman M, Cuff G, et al. Dexmedetomidine for awake carotid endarterectomy: efficacy, hemodynamic profile, and side effects. J Neurosurg Anesthesiol. 2004; 16:126–35.
Article6. McCutcheon CA, Orme RM, Scott DA, Davies MJ, McGlade DP. A comparison of dexmedetomidine versus conventional therapy for sedation and hemodynamic control during carotid endarterectomy performed under regional anesthesia. Anesth Analg. 2006; 102:668–75.
Article7. Tangkanakul C, Counsell CE, Warlow CP. Local versus general anaesthesia in carotid endarterectomy: a systematic review of the evidence. Eur J Vasc Endovasc Surg. 1997; 13:491–9.
Article8. Vaniyapong T, Chongruksut W, Rerkasem K. Local versus general anaesthesia for carotid endarterectomy. Cochrane Database Syst Rev. 2013; (12):CD000126.
Article9. Lirk P, Picardi S, Hollmann MW. Local anaesthetics: 10 essentials. Eur J Anaesthesiol. 2014; 31:575–85.10. Pandit JJ, Satya-Krishna R, Gration P. Superficial or deep cervical plexus block for carotid endarterectomy: a systematic review of complications. Br J Anaesth. 2007; 99:159–69.11. Hadzic A. Hadzic’s peripheral nerve blocks and anatomy for ultrasound-guided regional anesthesia. 2nd ed. New York: McGraw-Hill Medical;2012. p. 346–51.12. Marhofer P, Harrop-Griffiths W, Kettner SC, Kirchmair L. Fifteen years of ultrasound guidance in regional anaesthesia: part 1. Br J Anaesth. 2010; 104:538–46.
Article13. Demirel S, Celi de la Torre JA, Bruijnen H, Martin E, Popp E, Böckler D, et al. Effect of Superficial Cervical Plexus Block on Baroreceptor Sensitivity in Patients Undergoing Carotid Endarterectomy. J Cardiothorac Vasc Anesth. 2016; 30:309–16.
Article14. Merle JC, Mazoit JX, Desgranges P, Abhay K, Rezaiguia S, Dhonneur G, et al. A comparison of two techniques for cervical plexus blockade: evaluation of efficacy and systemic toxicity. Anesth Analg. 1999; 89:1366–70.
Article15. de Sousa AA, Filho MA, Faglione W Jr, Carvalho GT. Superficial vs combined cervical plexus block for carotid endarterectomy: a prospective, randomized study. Surg Neurol. 2005; 63(Suppl 1):S22–5.
Article16. Michenfelder JD, Sundt TM, Fode N, Sharbrough FW. Isoflurane when compared to enflurane and halothane decreases the frequency of cerebral ischemia during carotid endarterectomy. Anesthesiology. 1987; 67:336–40.
Article17. Umbrain V, Keeris J, D'Haese J, Verborgh C, Debing E, Van den Brande P, et al. Isoflurane, desflurane and sevoflurane for carotid endarterectomy. Anaesthesia. 2000; 55:1052–7.
Article18. Hartsell PA, Calligaro KD, Syrek JR, Dougherty MJ, Raviola CA. Postoperative blood pressure changes associated with cervical block versus general anesthesia following carotid endarterectomy. Ann Vasc Surg. 1999; 13:104–8.
Article19. Gassner M, Bauman Z, Parish S, Koenig C, Martin J, Hans S. Hemodynamic changes in patients undergoing carotid endarterectomy under cervical block and general anesthesia. Ann Vasc Surg. 2014; 28:1680–5.
Article20. McKevitt FM, Sivaguru A, Venables GS, Cleveland TJ, Gaines PA, Beard JD, et al. Effect of treatment of carotid artery stenosis on blood pressure: a comparison of hemodynamic disturbances after carotid endarterectomy and endovascular treatment. Stroke. 2003; 34:2576–81.
Article21. McCleary AJ, Dearden NM, Dickson DH, Watson A, Gough MJ. The differing effects of regional and general anaesthesia on cerebral metabolism during carotid endarterectomy. Eur J Vasc Endovasc Surg. 1996; 12:173–81.
Article22. Gottlieb A, Satariano-Hayden P, Schoenwald P, Ryckman J, Piedmonte M. The effects of carotid sinus nerve blockade on hemodynamic stability after carotid endarterectomy. J Cardiothorac Vasc Anesth. 1997; 11:67–71.
Article23. Hoefer J, Pierer E, Rantner B, Stadlbauer KH, Fraedrich G, Fritz J, et al. Ultrasound-guided regional anesthesia for carotid endarterectomy induces early hemodynamic and stress hormone changes. J Vasc Surg. 2015; 62:57–67.
Article24. Piascik MT, Soltis EE, Piascik MM, Macmillan LB. Alphaadrenoceptors and vascular regulation: molecular, pharmacologic and clinical correlates. Pharmacol Ther. 1996; 72:215–41.25. Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000; 93:382–94.
Article26. Jamil M, Usman R, Ghaffar S. Advantages of selective use of intraluminal shunt in carotid endarterectomy: a study of 122 cases. Ann Vasc Dis. 2016; 9:285–8.
Article27. Kong J, Li J, Ye Z, Fan X, Wen J, Zhang J, et al. Carotid endarterectomy with routine shunt for patients with contralateral carotid occlusion. Ann Thorac Cardiovasc Surg. 2017; 23:227–32.
Article28. Khattar NK, Friedlander RM, Chaer RA, Avgerinos ED, Kretz ES, Balzer JR, et al. Perioperative stroke after carotid endarterectomy: etiology and implications. Acta Neurochir (Wien). 2016; 158:2377–83.
Article29. Shin SW, Cho AR, Lee HJ, Kim HJ, Byeon GJ, Yoon JW, et al. Maintenance anaesthetics during remifentanil-based anaesthesia might affect postoperative pain control after breast cancer surgery. Br J Anaesth. 2010; 105:661–7.30. Dakour Aridi H, Paracha N, Nejim B, Locham S, Malas MB. Anesthetic type and hospital outcomes after carotid endarterectomy from the Vascular Quality Initiative database. J Vasc Surg. 2018; 67:1419–28.
Article31. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39:175–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-guided superficial cervical plexus block for carotid endarterectomy in a patient with Lemierre syndrome: A case report
- A Comparison of Combined Superficial Cervical Plexus Block and Interscalene Brachial Plexus Block with General Anesthesia for Clavicle Surgery: Pilot Trial
- Anesthetic Management of Carotid Endarterectomy under Cervical Plexus Block
- Dexamethasone or Dexmedetomidine as Local Anesthetic Adjuvants for Ultrasound-guided Axillary Brachial Plexus Blocks with Nerve Stimulation
- Pectoral nerve block (Pecs block) with sedation for breast conserving surgery without general anesthesia