J Korean Ophthalmol Soc.
2016 Nov;57(11):1699-1705. 10.3341/jkos.2016.57.11.1699.
Fitting the Miniscleral Contact Lens in Patients with Corneal Abnormalities
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University School of Medicine, Busan, Korea. jiel75@hanmail.net
- 2Department of Ophthalmology, Kosin University College of Medicine, Busan, Korea.
- 3YK Eye Clinic, Seoul, Korea.
- 4Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2357724
- DOI: http://doi.org/10.3341/jkos.2016.57.11.1699
Abstract
- PURPOSE
To evaluate the clinical results of fitting the miniscleral contact lens (MSD; Happy Vision Corp., Anyang, Korea) in patients with corneal abnormalities.
METHODS
Thirty-eight patients (56 eyes) fitted with MSD lenses were recruited for this study. Clinical indication, visual acuity, degree of comfort, mean wearing time, parameters of the finally prescribed lenses, number of fittings with trial lenses, success rate with the first prescribed lens, and adverse events were evaluated.
RESULTS
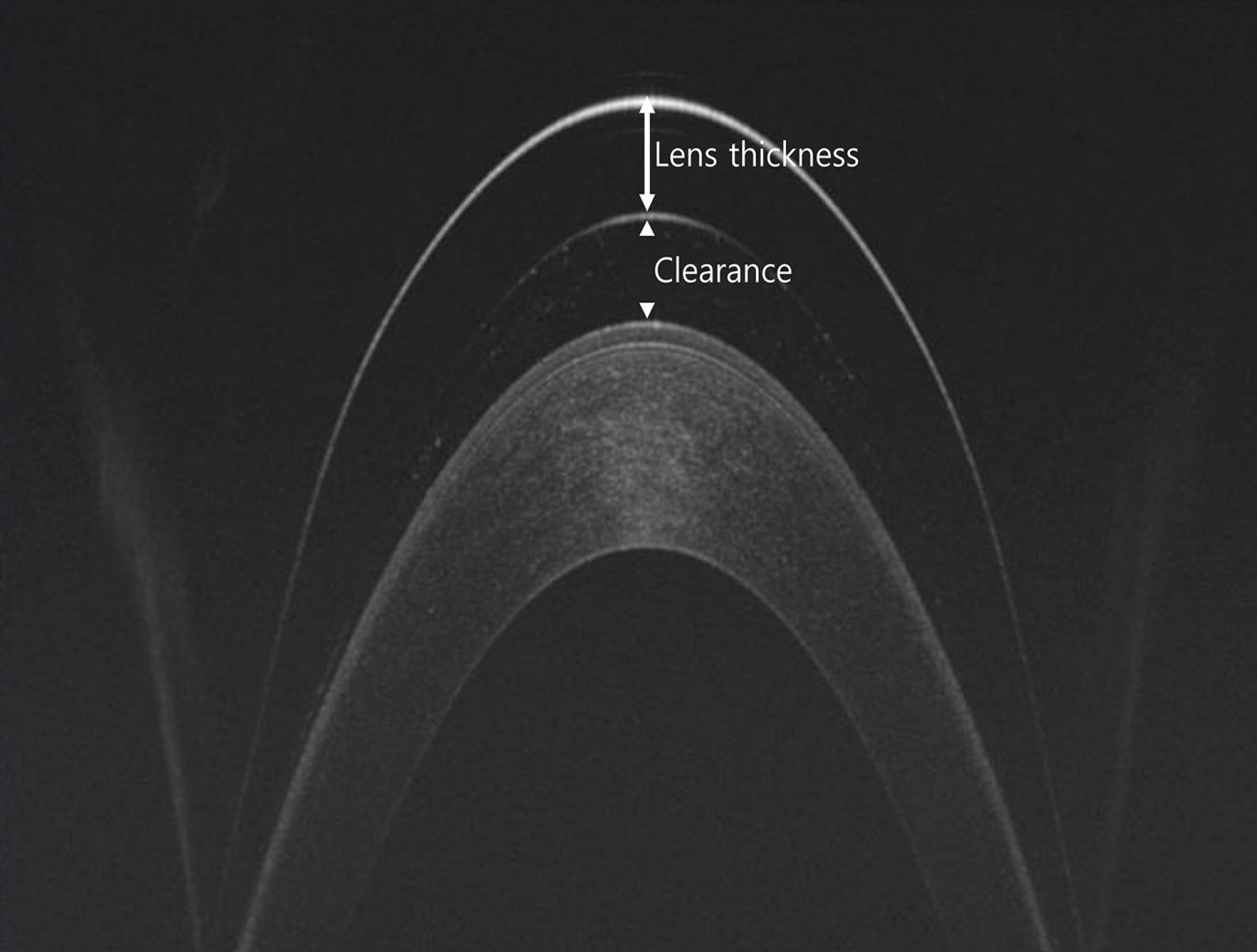
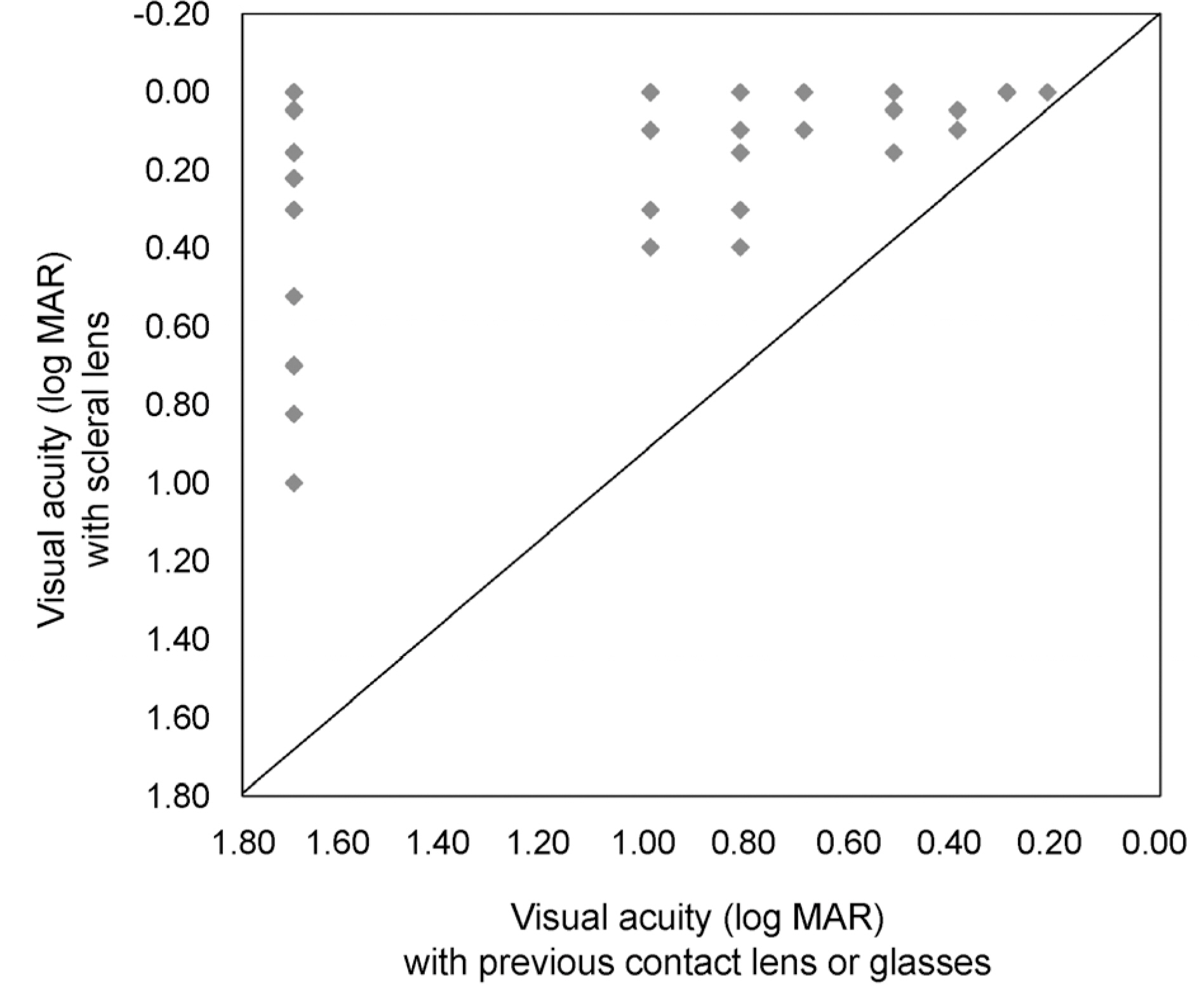
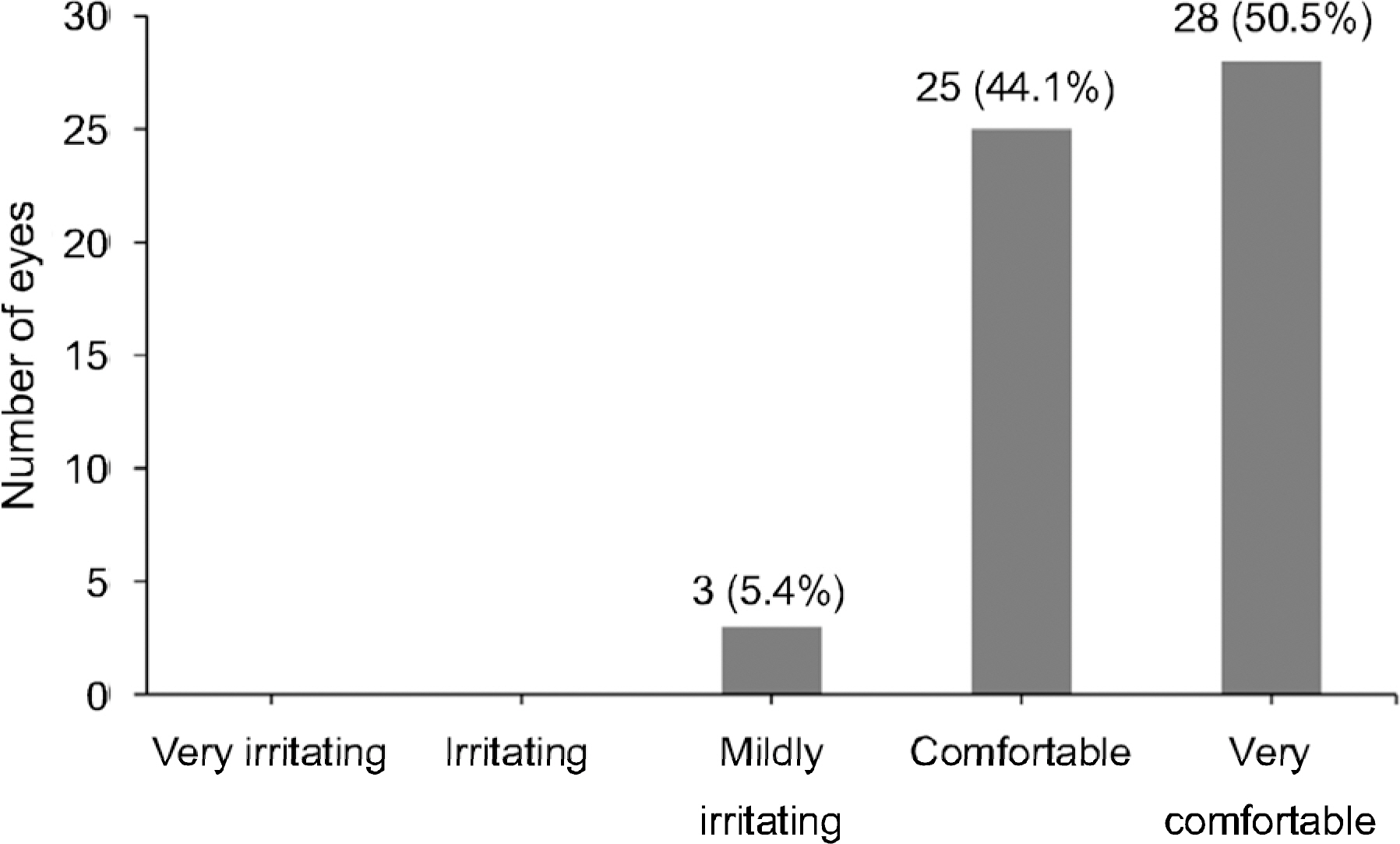
Forty-two (75%) of 56 eyes were enrolled in this study due to keratoconus. Other conditions included Stevens-Johnson syndrome (6 eyes, 11%), high postkeratoplasty astigmatism (3 eyes, 5%), corneal scarring (3 eyes, 5%), and ectasia after laser in situ keratomileusis (LASIK; 2 eyes, 4%). The mean log MAR visual acuity improved from 1.01 ± 0.64 to 0.13 ± 0.19 after wearing lenses (p= 0.0001). In 53 eyes (94.6%), patients reported the miniscleral contact lenses to be comfortable, and the mean daily wear time was 12.9 ± 2.5 hours. The mean sagittal depth of finally prescribed lenses was 4.67 ± 0.37 mm (3.7-5.4). An average of 3.3 ± 1.5 (1-7) trials were needed for the trial fitting, and the average number of re-prescriptions to achieve the optimal fitting was 1.5 ± 0.48 (1-3). One patient discontinued the lenses after 3 months due to discomfort.
CONCLUSIONS
Miniscleral contact lenses are a good alternative for patients with corneal abnormalities and result in both successful visual outcome and comfort.
MeSH Terms
Figure
Cited by 1 articles
-
The Therapeutic Effect of Sclerocorneal Lens in Coexisting Corneal Ectasia and Stevens-Johnson Syndrome
Jin Uk Baek, Chang Hyun Park, Kyung Sun Na, Hyun Seung Kim
J Korean Ophthalmol Soc. 2018;59(10):968-973. doi: 10.3341/jkos.2018.59.10.968.
Reference
-
References
1. Jupiter DG, Katz HR. Management of irregular astigmatism with rigid gas permeable contact lenses. CLAO J. 2000; 26:14–7.2. Rosenthal P, Croteau A. Fluid-ventilated, gas-permeable scleral contact lens is an effective option for managing severe ocular abdominal disease and many corneal disorders that would otherwise require penetrating keratoplasty. Eye Contact Lens. 2005; 31:130–4.3. Smiddy WE, Hamburg TR, Kracher GP, Stark WJ. Keratoconus. Contact lens or keratoplasty? Ophthalmology. 1988; 95:487–92.
Article4. Pecego M, Barnett M, Mannis MJ, Durbin-Johnson B. Jupiter Scleral Lenses: the UC Davis Eye Center experience. Eye Contact Lens. 2012; 38:179–82.5. Pullum KW, Whiting MA, Buckley RJ. Scleral contact lenses: the expanding role. Cornea. 2005; 24:269–77.6. Schornack MM, Patel SV. Relationship between corneal abdominal indices and scleral lens base curve. Eye Contact Lens. 2010; 36:330–3.7. Pullum KW. Scleral lenses. Bennett ES, Weissman BA, editors. Clinical contact lens practice. 2nd ed.Philadelphia: Lippincott Williams & Wilkins;2005. chap. 15.8. Kok JH, Visser R. Treatment of ocular surface disorders and dry eyes with high gas-permeable scleral lenses. Cornea. 1992; 11:518–22.
Article9. Visser ES, Visser R, van Lier HJ, Otten HM. Modern scleral lenses part II: patient satisfaction. Eye Contact Lens. 2007; 33:21–5.
Article10. Segal O, Barkana Y, Hourovitz D, et al. Scleral contact lenses may help where other modalities fail. Cornea. 2003; 22:308–10.
Article11. Schornack MM, Patel SV. Scleral lenses in the management of keratoconus. Eye Contact Lens. 2010; 36:39–44.
Article12. Romero-Rangel T, Stavrou P, Cotter J, et al. Gas-permeable scleral contact lens therapy in ocular surface disease. Am J Ophthalmol. 2000; 130:25–32.
Article13. Schornack MM, Baratz KH, Patel SV, Maguire LJ. Jupiter scleral lenses in the management of chronic graft versus host disease. Eye Contact Lens. 2008; 34:302–5.
Article14. Shah-Desai SD, Aslam SA, Pullum K, et al. Scleral contact lens usage in patients with complex blepharoptosis. Ophthal Plast Reconstr Surg. 2011; 27:95–8.
Article15. Jacobs DS. Update on scleral lenses. Curr Opin Ophthalmol. 2008; 19:298–301.
Article16. Severinsky B, Behrman S, Frucht-Pery J, Solomon A. Scleral abdominal lenses for visual rehabilitation after penetrating keratoplasty: long term outcomes. Cont Lens Anterior Eye. 2014; 37:196–202.17. Gemoules G. A novel method of fitting scleral lenses using high resolution optical coherence tomography. Eye Contact Lens. 2008; 34:80–3.
Article18. van der Worp E, Bornman D, Ferreira DL, et al. Modern scleral contact lenses: a review. Cont Lens Anterior Eye. 2014; 37:240–50.
Article19. Dalton K, Sorbara L. Fitting an MSD (mini scleral design) rigid contact lens in advanced keratoconus with INTACS. Cont Lens Anterior Eye. 2011; 34:274–81.
Article20. Lee JC, Chiu GB, Bach D, et al. Functional and visual abdominal with prosthetic replacement of the ocular surface ecosystem scleral lenses for irregular corneas. Cornea. 2013; 32:1540–3.21. Mandathara Sudharman P, Rathi V, Dumapati S. Rose K lenses for keratoconus-an Indian experience. Eye Contact Lens. 2010; 36:220–2.
Article22. Kang YS, Park YK, Lee JS, et al. The effect of the YK lens in keratoconus. Ophthalmic Physiol Opt. 2010; 30:267–73.
Article23. Betts AM, Mitchell GL, Zadnik K. Visual performance and abdominal with the Rose K lens for keratoconus. Optom Vis Sci. 2002; 79:493–501.