Brain Tumor Res Treat.
2016 Oct;4(2):133-137. 10.14791/btrt.2016.4.2.133.
A Stable Secondary Gliosarcoma with Extensive Systemic Metastases: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Kwangju Christian Hospital, Gwangju, Korea.
- 2Department of Neurosurgery, Chonnam National University Hwasun Hospital & Medical School, Gwangju, Korea. jung-ty@chonnam.ac.kr
- 3Department of Pathology, Chonnam National University Research Institute of Medical Sciences, Chonnam National University Hwasun Hospital & Medical School, Gwangju, Korea.
- KMID: 2356983
- DOI: http://doi.org/10.14791/btrt.2016.4.2.133
Abstract
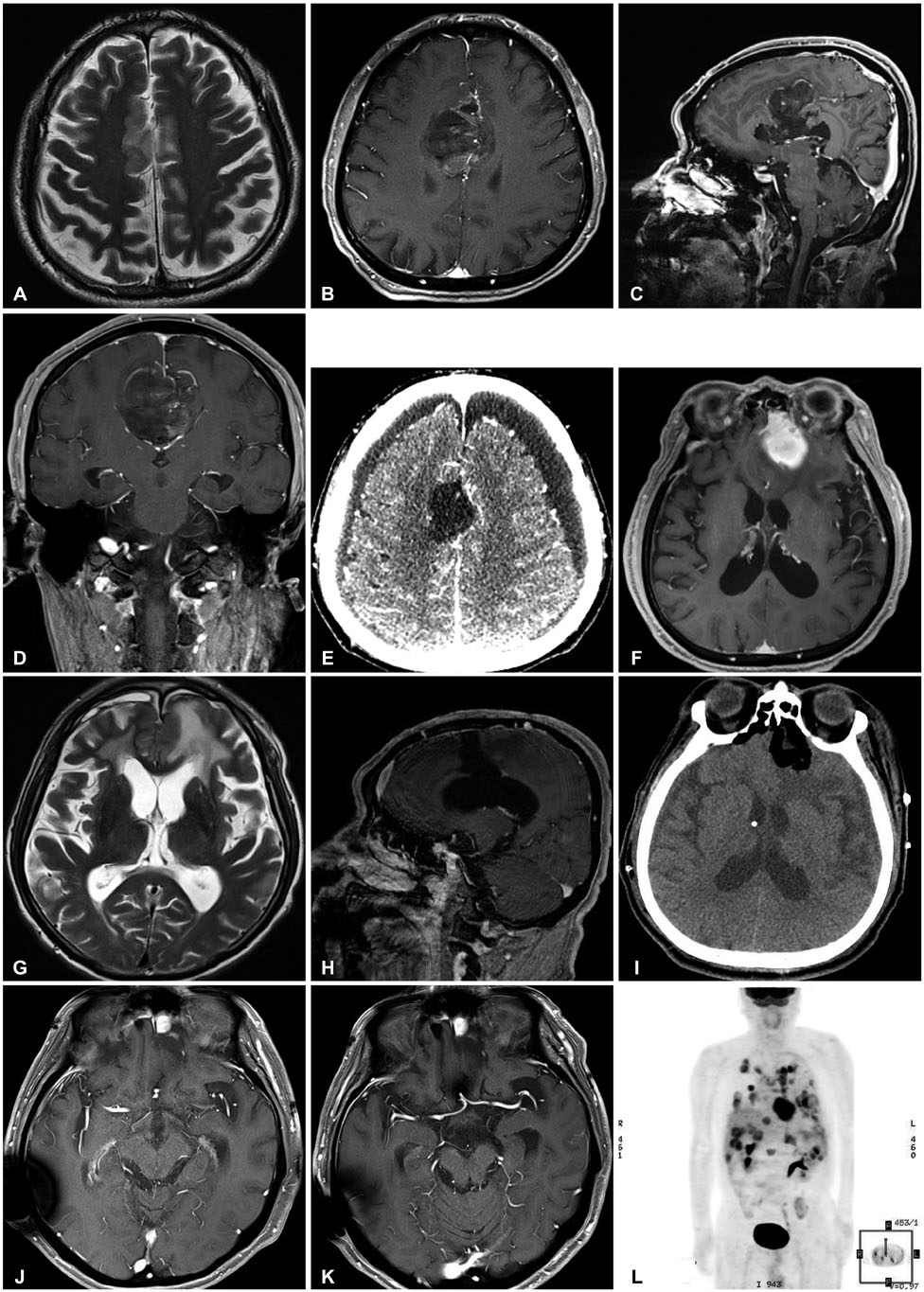
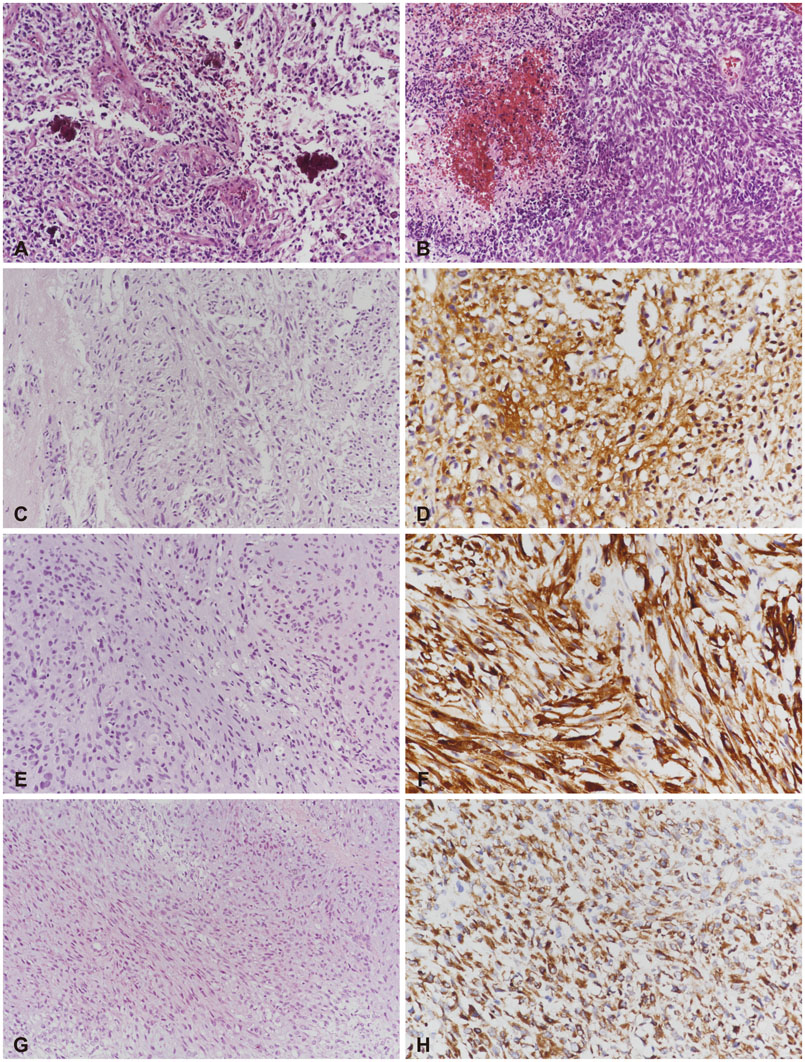
- A 63-year-old man complained of intermittent motor weakness of his arm. The magnetic resonance image (MRI) of his brain displayed a high signal lesion in right cingulate gyrus on T2 weighted image. One year later, he showed a stuporous mental status with repeated seizures, and the follow-up brain MRI showed heterogeneously enhanced mass associated with bleeding. He was treated with surgery and radiotherapy for secondary glioblastomas in right cingulate gyrus. One year more later, a mass recurred on the left frontal base, and gliosarcoma was diagnosed. After tumor resection, ventriculoperitoneal shunt, chemotherapy, and re-radiation therapy, all brain lesions were stable. Fourteen months after the diagnosis of gliosarcoma, he complained of dyspnea and back pain. Torso positron emission tomography/computed tomography revealed multiple metastatic lesions in both lungs, pericardium, pleura, liver, lymph nodes, and bones, and metastatic gliosarcoma was diagnosed. One month later, the patient died because of the systemic metastases. We present an unusual case of secondary gliosarcoma with stable brain lesions and extensive systemic metastases.
MeSH Terms
Figure
Reference
-
1. Ben Nsir A, Thai QA, Kassar AZ, Ben Said I, Jemel H. Primary cerebellar gliosarcoma with extracranial metastases: an orphan differential diagnosis. World Neurosurg. 2015; 84:2076.e13-7.
Article2. Rapp M, Felsberg J, Sorg RV, Gerharz CD, Sabel M. Case report: extracranial metastasis from gliosarcoma--the influence of immune system. Br J Neurosurg. 2011; 25:286–288.
Article3. Andaloussi-Saghir K, Oukabli M, El Marjany M, Sifat H, Hadadi K, Mansouri H. Secondary gliosarcoma after the treatment of primary glioblastoma multiforme. N Am J Med Sci. 2011; 3:527–530.
Article4. Rizvi S, Asghar AH, Mehboob J. Gliosarcoma: a rare variant of glioblastoma multiforme. J Pak Med Assoc. 2010; 60:773–775.5. Mason A, Villavicencio AT, Nelson EL, Forsythe RC, Burneikiene S. Post-treatment gliosarcoma extension into the pterygomaxillary fossa: literature review and case report. Cureus. 2016; 8:e700.
Article6. Dawar R, Fabiano AJ, Qiu J, Khushalani NI. Secondary gliosarcoma with extra-cranial metastases: a report and review of the literature. Clin Neurol Neurosurg. 2013; 115:375–380.
Article7. Lun M, Lok E, Gautam S, Wu E, Wong ET. The natural history of extracranial metastasis from glioblastoma multiforme. J Neurooncol. 2011; 105:261–273.
Article