Clin Endosc.
2016 Sep;49(5):475-478. 10.5946/ce.2016.002.
Non-Exposed Endoscopic Wall-Inversion Surgery for Gastrointestinal Stromal Tumor of the Stomach: First Case Report in Korea
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea. gastro@catholic.ac.kr
- 2Department of General Surgery, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea.
- KMID: 2356056
- DOI: http://doi.org/10.5946/ce.2016.002
Abstract
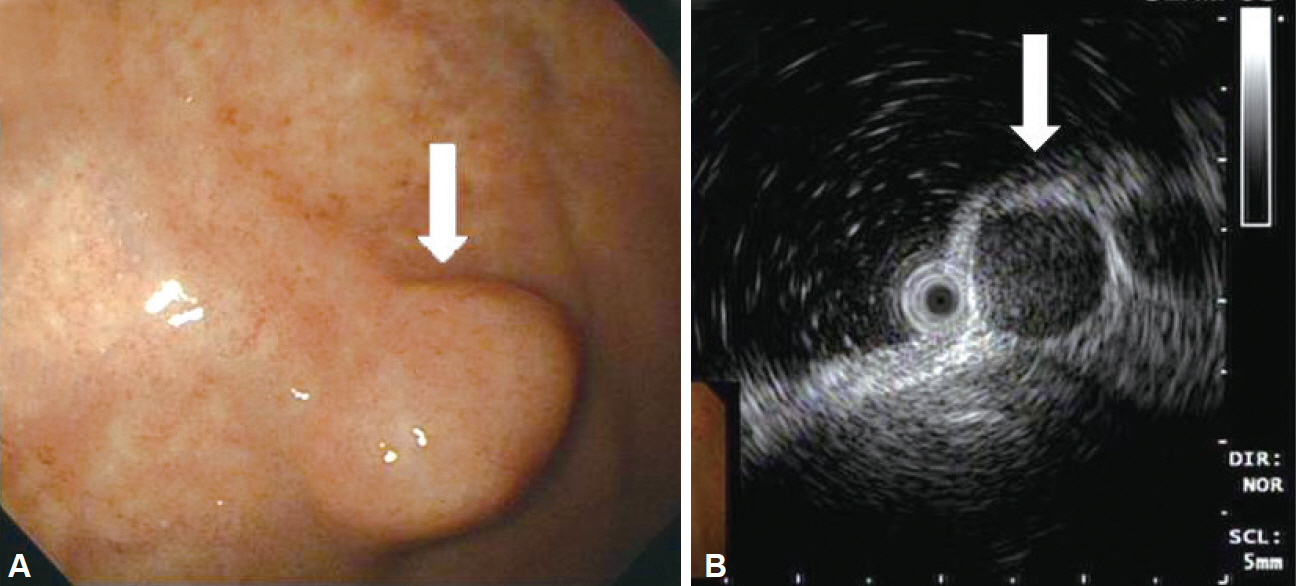
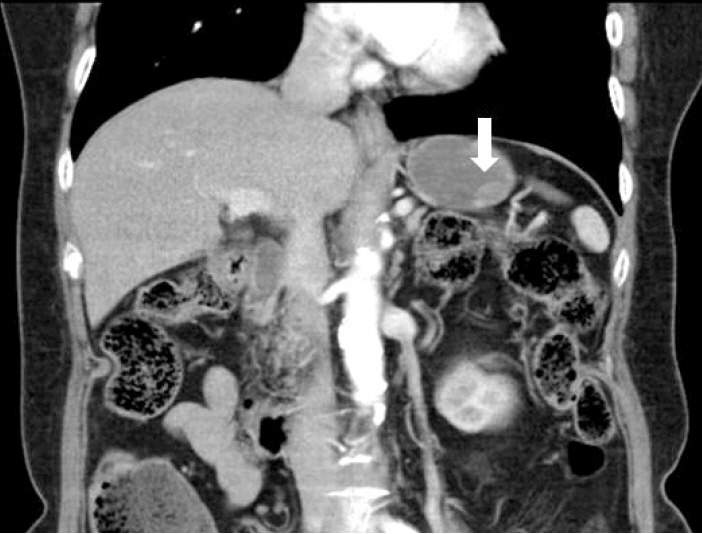
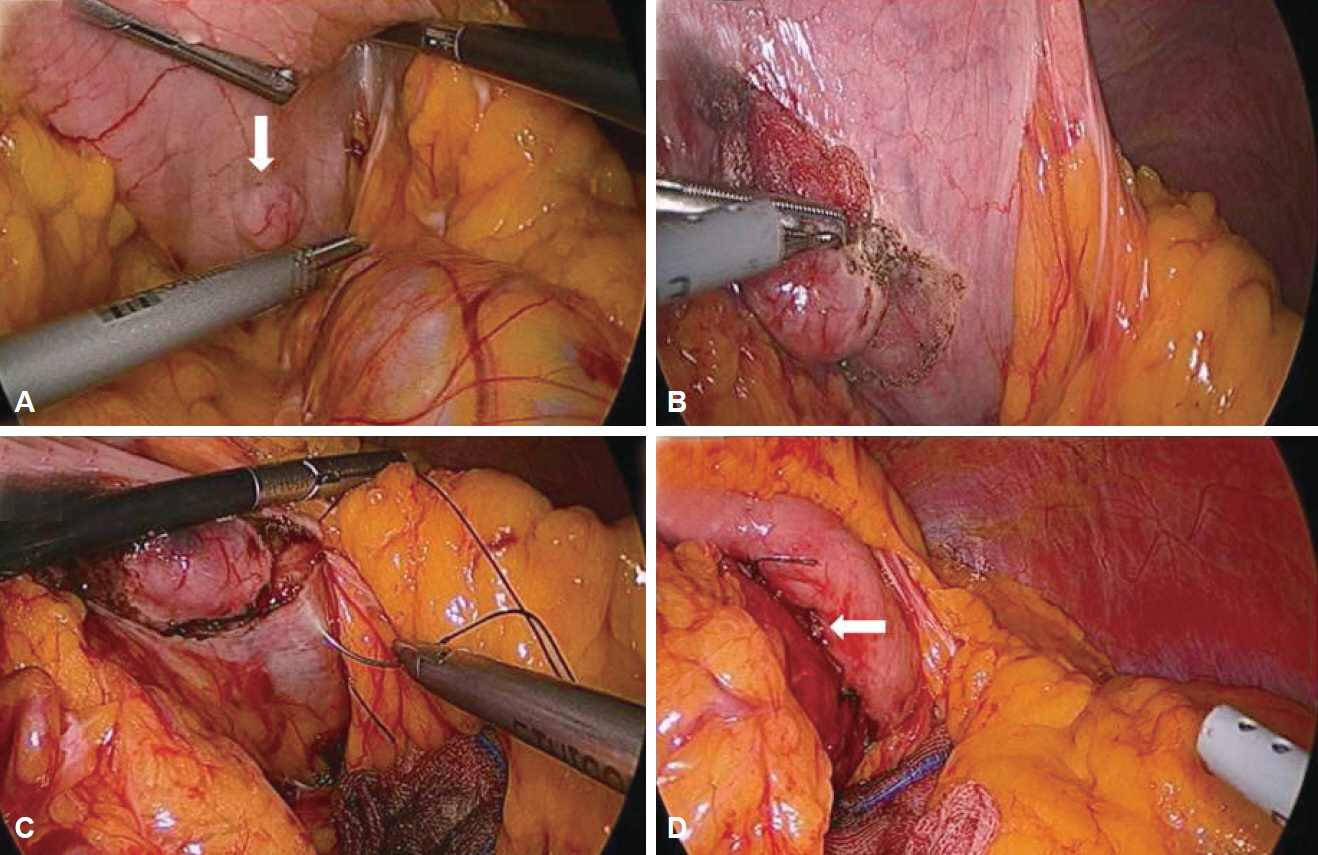
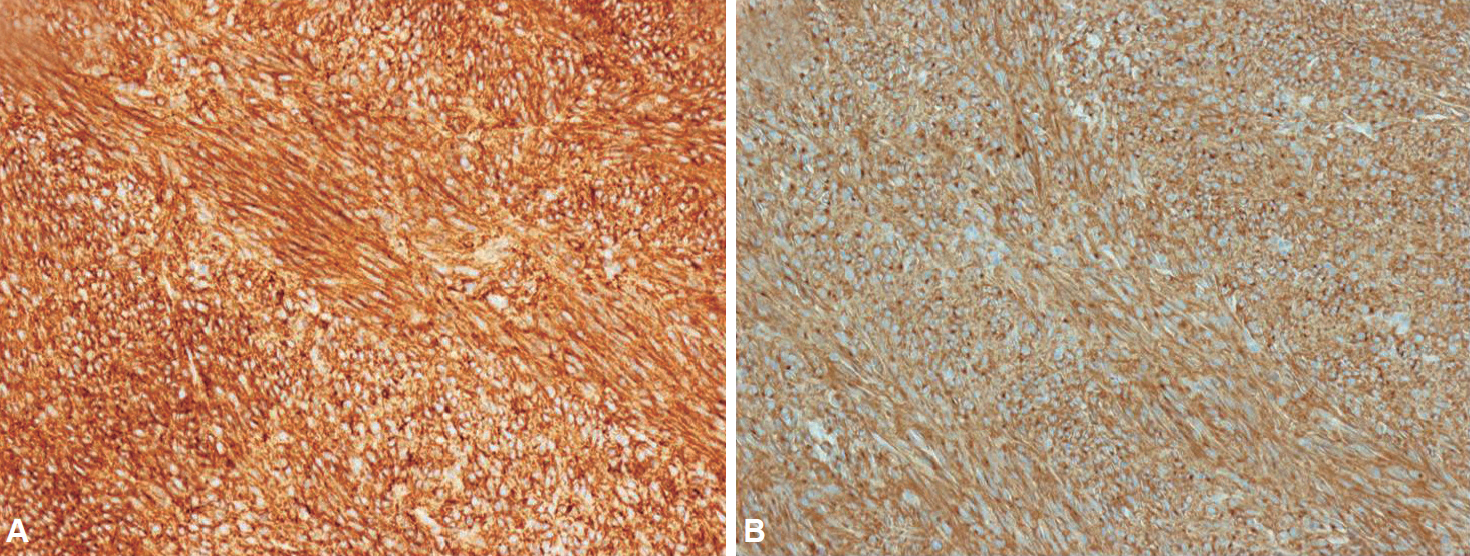
- Laparoscopic wedge resection of the stomach is a widely accepted treatment for primary resectable gastrointestinal stromal tumors (GISTs). However, it is difficult to determine the appropriate incision line from outside of the stomach, and many attempts have been made to avoid unnecessary resection of unaffected gastric tissues. Recently a technique called non-exposed endoscopic wall-inversion surgery (NEWS) was introduced to avoid exposure of GIST to the peritoneum. Here, we describe the first published case of NEWS for GIST of the stomach practiced in Korea.
Figure
Cited by 1 articles
-
Non-Exposure Endoscopic-Laparoscopic Cooperative Surgery for Stomach Tumors: First Experience from the Czech Republic
Jan Hajer, Lukáš Havlůj, Adam Whitley, Robert Gürlich
Clin Endosc. 2018;51(2):167-173. doi: 10.5946/ce.2017.076.
Reference
-
1. Demetri GD, Benjamin RS, Blanke CD, et al. NCCN Task Force report: management of patients with gastrointestinal stromal tumor (GIST): update of the NCCN clinical practice guidelines. J Natl Compr Canc Netw. 2007; 5 Suppl 2:S1–S29.2. Hiki N, Nunobe S, Matsuda T, Hirasawa T, Yamamoto Y, Yamaguchi T. Laparoscopic endoscopic cooperative surgery. Dig Endosc. 2015; 27:197–204.
Article3. Goto O, Mitsui T, Fujishiro M, et al. New method of endoscopic full-thickness resection: a pilot study of non-exposed endoscopic wall-inversion surgery in an ex vivo porcine model. Gastric Cancer. 2011; 14:183–187.
Article4. Inoue H, Ikeda H, Hosoya T, et al. Endoscopic mucosal resection, endoscopic submucosal dissection, and beyond: full-layer resection for gastric cancer with nonexposure technique (CLEAN-NET). Surg Oncol Clin N Am. 2012; 21:129–140.
Article5. Mitsui T, Niimi K, Yamashita H, et al. Non-exposed endoscopic wall-inversion surgery as a novel partial gastrectomy technique. Gastric Cancer. 2014; 17:594–599.
Article6. Goto O, Takeuchi H, Kawakubo H, et al. First case of non-exposed endoscopic wall-inversion surgery with sentinel node basin dissection for early gastric cancer. Gastric Cancer. 2015; 18:434–439.
Article7. Ye LP, Zhang Y, Mao XL, et al. Submucosal tunnelling endoscopic resection for the treatment of esophageal submucosal tumours originating from the muscularis propria layer: an analysis of 15 cases. Dig Liver Dis. 2013; 45:119–123.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Full-thickness Resection for Gastric Tumor
- Non-Exposure Endoscopic-Laparoscopic Cooperative Surgery for Stomach Tumors: First Experience from the Czech Republic
- Two Cases of Advanced Gastric Carcinoma Mimicking a Malignant Gastrointestinal Stromal Tumor
- A case of huge Gastrointestinal stromal tumor masquerading as an ovarian malignancy
- A Case of Epithelioid Type Gastric Gastrointestinal Stromal Tumor with Gastrointestinal Bleeding