J Cerebrovasc Endovasc Neurosurg.
2016 Sep;18(3):239-246. 10.7461/jcen.2016.18.3.239.
The Efficacy of Single Barrel Superficial Temporal Artery-middle Cerebral Artery Bypass in Treatment of Adult Patients with Ischemic-type Moyamoya Disease
- Affiliations
-
- 1Department of Neurosurgery, Medical Research Institute, Pusan National University Hospital, Busan, Korea. redcheek09@naver.com
- 2Department of Neurosurgery, Medical Research Institute, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2355648
- DOI: http://doi.org/10.7461/jcen.2016.18.3.239
Abstract
OBJECTIVE
So far, there is no study answering the question of which type of surgical technique is practically the most useful in the treatment of adult patients with ischemic type moyamoya disease (MMD). We evaluated the efficacy of single barrel superficial temporal artery (STA)-middle cerebral artery (MCA) bypass in the treatment of adult patients with ischemic type MMD by retrospectively collecting clinical and radiological data.
MATERIALS AND METHODS
A retrospective review identified 31 adult patients who underwent 43 single barrel STA-MCA bypass procedures performed for treatment of ischemic-type MMD between 2006 and 2014. The male to female ratio was 17:14 and the mean age was 41 years (range, 21-65 years). Peri-operative complications, angiographic and clinical outcomes were analyzed retrospectively.
RESULTS
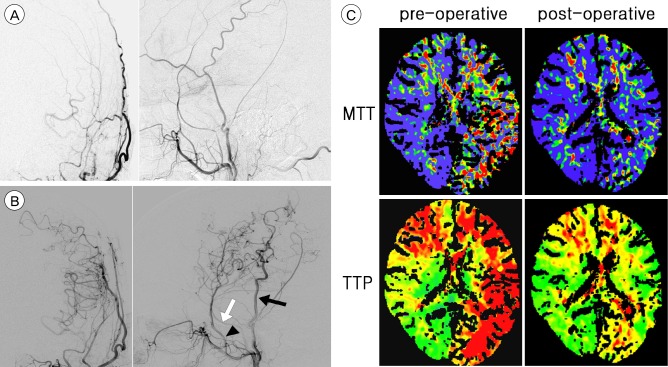
The permanent neurological morbidity and mortality rates were 2.3% and 0%, respectively. During the observation period of a mean of 35 months (range, 12-73 months), 29 patients (93.5%) had no further cerebrovascular events and transient ischemic attack occurred in two patients (6.5%), resulting in an annual stroke risk of 2.2%. Follow-up computed tomography perfusion (CTP) (mean, 18.4 months after surgery) documented improved cerebral hemodynamics in the revascularized hemispheres (p < 0.001). Post-operative patency was clearly verified in 38 bypasses (88.4%) of 43 bypasses on follow-up imaging (mean, 16.5 months).
CONCLUSION
Our results suggest that single barrel STA-MCA bypass with wide dural opening is safe and durable method of cerebral revascularization in adult patients with ischemic type MMD and can be considered as a potential treatment option for adult patients with ischemic type MMD.
Keyword
MeSH Terms
Figure
Reference
-
1. Bang JS, Kwon OK, Kim JE, Kang HS, Park H, Cho SY, et al. Quantitative angiographic comparison with the OSIRIS program between the direct and indirect revascularization modalities in adult moyamoya disease. Neurosurgery. 2012; 3. 70(3):625–632. discussion 632-3. PMID: 21866061.
Article2. Cho WS, Kim JE, Kim CH, Ban SP, Kang HS, Son YJ, et al. Long-term outcomes after combined revascularization surgery in adult moyamoya disease. Stroke. 2014; 10. 45(10):3025–3031. PMID: 25184359.
Article3. Czabanka M, Pena-Tapia P, Scharf J, Schubert GA, Munch E, Horn P, et al. Characterization of direct and indirect cerebral revascularization for the treatment of European patients with moyamoya disease. Cerebrovasc Dis. 2011; 32(4):361–369. PMID: 21921600.
Article4. Czabanka M, Vajkoczy P, Schmiedek P, Horn P. Age-dependent revascularization patterns in the treatment of moyamoya disease in a European patient population. Neurosurg Focus. 2009; 4. 26(4):E9.
Article5. Fujimura M, Kaneta T, Shimizu H, Tominaga T. Cerebral ischemia owing to compression of the brain by swollen temporal muscle used for encephalo-myo-synangiosis in moyamoya disease. Neurosurg Rev. 2009; 4. 32(2):245–249. discussion 249. PMID: 19159959.
Article6. Fujimura M, Shimizu H, Inoue T, Mugikura S, Saito A, Tominaga T. Significance of focal cerebral hyperperfusion as a cause of transient neurologic deterioration after extracranial-intracranial bypass for moyamoya disease: comparative study with non-moyamoya patients using N-isopropyl-p-[(123)I]iodoamphetamine single-photon emission computed tomography. Neurosurgery. 2011; 4. 68(4):957–964. discussion 964-5. PMID: 21221039.
Article7. Hayashi K, Horie N, Izumo T, Nagata I. A nationwide survey on unilateral moyamoya disease in Japan. Clin Neurol Neurosurg. 2014; 9. 124:1–5. PMID: 24976021.
Article8. Ishikawa T, Kamiyama H, Kuroda S, Yasuda H, Nakayama N, Takizawa K. Simultaneous superficial temporal artery to middle cerebral or anterior cerebral artery bypass with pan-synangiosis for Moyamoya disease covering both anterior and middle cerebral artery territories. Neurol Med Chir (Tokyo). 2006; 9. 46(9):462–468. PMID: 16998283.9. Jang DK, Lee KS, Rha HK, Huh PW, Yang JH, Park IS, et al. Clinical and angiographic features and stroke types in adult moyamoya disease. AJNR Am J Neuroradiol. 2014; 6. 35(6):1124–1131. PMID: 24384121.
Article10. Jiang H, Ni W, Xu B, Lei Y, Tian Y, Xu F, et al. Outcome in adult patients with hemorrhagic moyamoya disease after combined extracranial-intracranial bypass. J Neurosurg. 2014; 11. 121(5):1048–1055. PMID: 25127415.
Article11. Kazumata K, Ito M, Tokairin K, Ito Y, Houkin K, Nakayama N, et al. The frequency of postoperative stroke in moyamoya disease following combined revascularization: a single-university series and systematic review. J Neurosurg. 2014; 8. 121(2):432–440. PMID: 24605834.
Article12. Kim DS, Kang SG, Yoo DS, Huh PW, Cho KS, Park CK. Surgical results in pediatric moyamoya disease: angiographic revascularization and the clinical results. Clin Neurol Neurosurg. 2007; 2. 109(2):125–131. PMID: 16872739.
Article13. Kim SK, Cho BK, Phi JH, Lee JY, Chae JH, Kim KJ, et al. Pediatric moyamoya disease: An analysis of 410 consecutive cases. Ann Neurol. 2010; 7. 68(1):92–101. PMID: 20582955.
Article14. Liu X, Zhang D, Shuo W, Zhao Y, Wang R, Zhao J. Long term outcome after conservative and surgical treatment of haemorrhagic moyamoya disease. J Neurol Neurosurg Psychiatry. 2013; 3. 84(3):258–265. PMID: 23012444.
Article15. Mizoi K, Kayama T, Yoshimoto T, Nagamine Y. Indirect revascularization for moyamoya disease: is there a beneficial effect for adult patients. Surg Neurol. 1996; 6. 45(6):541–548. PMID: 8638240.
Article16. Powers WJ, Clarke WR, Grubb RL Jr, Videen TO, Adams HP Jr, Derdeyn CP, et al. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA. 2011; 11. 306(18):1983–1992. PMID: 22068990.17. Hashimoto N, Tominaga T, Miyamoto S, Nagata I, Houkin K, Suzuki N, et al. Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo). 2012; 52(5):245–266. PMID: 22870528.18. Ryan RW, Chowdhary A, Britz GW. Hemorrhage and risk of further hemorrhagic strokes following cerebral revascularization in Moyamoya disease: A review of the literature. Surg Neurol Int. 2012; 3:72. PMID: 22937473.
Article19. Scott RM, Smith JL, Robertson RL, Madsen JR, Soriano SG, Rockoff MA. Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg. 2004; 2. 100(2 Suppl Pediatrics):142–149. PMID: 14758941.
Article20. Sim YW, Lee MS, Kim YG, Kim DH. Unpredictable postoperative global cerebral infarction in the patient of williams syndrome accompanying moyamoya disease. J Korean Neurosurg Soc. 2011; 9. 50(3):256–259. PMID: 22102960.
Article21. Starke RM, Komotar RJ, Hickman ZL, Paz YE, Pugliese AG, Otten ML, et al. Clinical features, surgical treatment, and long-term outcome in adult patients with moyamoya disease. J Neurosurg. 2009; 11. 111(5):936–942. PMID: 19374496.
Article22. Uchino H, Kuroda S, Hirata K, Shiga T, Houkin K, Tamaki N. Predictors and clinical features of postoperative hyperperfusion after surgical revascularization for moyamoya disease: a serial single photon emission CT/positron emission tomography study. Stroke. 2012; 10. 43(10):2610–2616. PMID: 22871684.23. Xie A, Luo L, Ding Y, Li G. Ischemic and hemorrhagic moyamoya disease in adults: CT findings. Int J Clin Exp Med. 2015; 11. 8(11):21351–21357. PMID: 26885076.24. Xu B, Song DL, Mao Y, Gu YX, Xu H, Liao YJ, et al. Superficial temporal artery-middle cerebral artery bypass combined with encephalo-duro-myo-synangiosis in treating moyamoya disease: surgical techniques, indications and midterm follow-up results. Chin Med J (Engl). 2012; 12. 125(24):4398–4405. PMID: 23253709.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Middle Cerebral Artery AneurysmOriginating Near the Site of Anastomosis after Superficial Temporal Artery-Middle Cerebral Artery Bypass: Case Report
- Effect of Direct Revascularization in Ischemic Type of Adult Moyamoya Disease
- Clinical Analysis of Surgically Treated Moyamoya Diseases
- Development of Brain Infarction after Extracranial-Intracranial Bypass Surgery in a Patient with Moyamoya Disease: A case report
- Off-Pump Coronary Artery Bypass Grafting in Moyamoya Disease