J Korean Med Sci.
2016 Dec;31(12):2020-2025. 10.3346/jkms.2016.31.12.2020.
Swallowing Function Defined by Videofluoroscopic Swallowing Studies after Anterior Cervical Discectomy and Fusion: a Prospective Study
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Chung-Ang University College of Medicine, Seoul, Korea. donkim21@gmail.com
- 2Department of Neurosurgery, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2355634
- DOI: http://doi.org/10.3346/jkms.2016.31.12.2020
Abstract
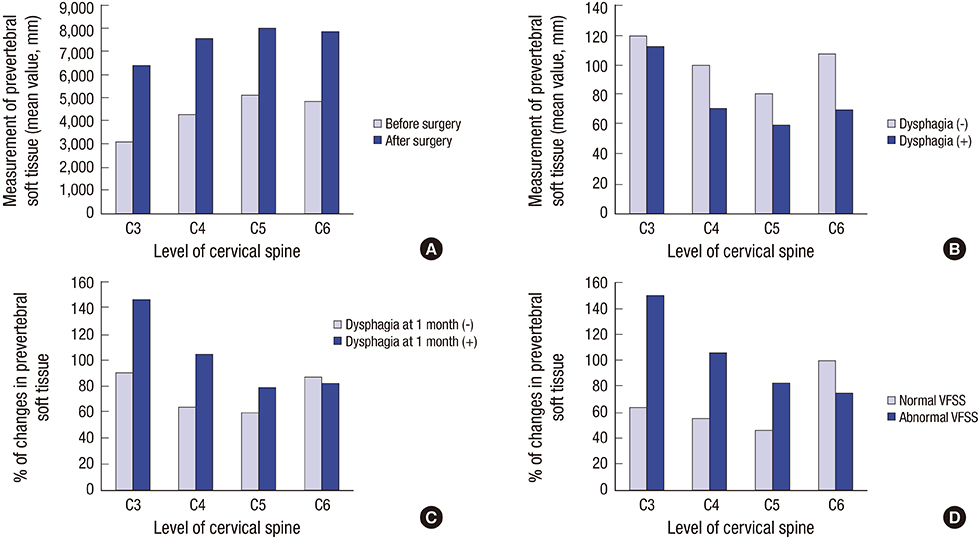
- This study evaluated factors related to swallowing dysfunction after anterior cervical discectomy and fusion (ACDF) using videofluoroscopic swallowing studies (VFSS). Preoperative and postoperative VFSSs were done with 5 mL diluted barium. Oral transit time, pharyngeal delay time, pharyngeal response time (PRT), and pharyngeal transit time were measured. Hyoid bone movement and upper esophageal sphincter (UES) diameter were measured serially. Thickness of prevertebral soft tissue was measured from digitized VFSS images. In results, 12 of 20 patients showed abnormal postoperative VFSS findings. PRT decreased significantly after surgery. Hyoid bone movement did not change significantly after surgery. The maximal distance of UES opening decreased significantly after surgery, and the higher the level of surgery (C3 > C4 > C5 > C6), the greater the decrease in maximal distance of the UES opening after surgery. The time to widest opening of the UES was prolonged significantly. At the C3 and C4 levels, the change in prevertebral soft tissue thickness of patients with VFSS abnormalities was significantly greater than those without abnormalities. In conclusion, patients after ADCF with their highest surgery level at C3 and C4 showed more abnormal VFSS findings, significantly increased soft tissue thickness, and decreased maximal distance of UES opening. VFSS provided objective data related with swallowing dysfunction after ACDF.
Keyword
MeSH Terms
Figure
Reference
-
1. Skeppholm M, Ingebro C, Engström T, Olerud C. The dysphagia short questionnaire: an instrument for evaluation of dysphagia: a validation study with 12 months’ follow-up after anterior cervical spine surgery. Spine. 2012; 37:996–1002.2. Frempong-Boadu A, Houten JK, Osborn B, Opulencia J, Kells L, Guida DD, Le Roux PD. Swallowing and speech dysfunction in patients undergoing anterior cervical discectomy and fusion: a prospective, objective preoperative and postoperative assessment. J Spinal Disord Tech. 2002; 15:362–368.3. Tervonen H, Niemelä M, Lauri ER, Back L, Juvas A, Räsänen P, Roine RP, Sintonen H, Salmi T, Vilkman SE, et al. Dysphonia and dysphagia after anterior cervical decompression. J Neurosurg Spine. 2007; 7:124–130.4. Yue WM, Brodner W, Highland TR. Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year follow-up study. Eur Spine J. 2005; 14:677–682.5. McAfee PC, Cappuccino A, Cunningham BW, Devine JG, Phillips FM, Regan JJ, Albert TJ, Ahrens JE. Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Tech. 2010; 23:1–8.6. Kang SH, Kim DK, Seo KM, Kim KT, Kim YB. Multi-level spinal fusion and postoperative prevertebral thickness increase the risk of dysphagia after anterior cervical spine surgery. J Clin Neurosci. 2011; 18:1369–1373.7. Riley LH 3rd, Vaccaro AR, Dettori JR, Hashimoto R. Postoperative dysphagia in anterior cervical spine surgery. Spine. 2010; 35:S76–85.8. Siska PA, Ponnappan RK, Hohl JB, Lee JY, Kang JD, Donaldson WF 3rd. Dysphagia after anterior cervical spine surgery: a prospective study using the swallowing-quality of life questionnaire and analysis of patient comorbidities. Spine. 2011; 36:1387–1391.9. Logemann JA. Manual for the Videofluorographic Study of Swallowing. 2nd ed. Austin, TX: Pro-Ed;1993.10. Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. J Speech Lang Hear Res. 2000; 43:1264–1274.11. Min Y, Kim WS, Kang SS, Choi JM, Yeom JS, Paik NJ. Incidence of dysphagia and serial videofluoroscopic swallow study findings after anterior cervical discectomy and fusion: a prospective study. Clin Spine Surg. 2016; 29:E177–81.12. Leonard R, Belafsky P. Dysphagia following cervical spine surgery with anterior instrumentation: evidence from fluoroscopic swallow studies. Spine. 2011; 36:2217–2223.13. Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine. 2002; 27:2453–2458.14. Rihn JA, Kane J, Joshi A, Albert TJ, Vaccaro AR, Harrop J, Anderson DG, Hilibrand AS. Gastroesophageal reflux after anterior cervical surgery: a controlled, prospective analysis. Spine. 2011; 36:2039–2044.15. Cho SK, Lu Y, Lee DH. Dysphagia following anterior cervical spinal surgery: a systematic review. Bone Joint J. 2013; 95-B:868–873.16. Zeng JH, Zhong ZM, Chen JT. Early dysphagia complicating anterior cervical spine surgery: incidence and risk factors. Arch Orthop Trauma Surg. 2013; 133:1067–1071.17. Rihn JA, Kane J, Albert TJ, Vaccaro AR, Hilibrand AS. What is the incidence and severity of dysphagia after anterior cervical surgery? Clin Orthop Relat Res. 2011; 469:658–665.