Korean J Ophthalmol.
2016 Oct;30(5):360-368. 10.3341/kjo.2016.30.5.360.
Non-human Immunodeficiency Virus-related Ocular Syphilis in a Korean Population: Clinical Manifestations and Treatment Outcomes
- Affiliations
-
- 1Department of Ophthalmology, Kyung Hee University Hospital, Kyung Hee University School of Medicine, Seoul, Korea. syyu@khu.ac.kr
- KMID: 2353829
- DOI: http://doi.org/10.3341/kjo.2016.30.5.360
Abstract
- PURPOSE
To describe the clinical manifestations and treatment outcomes of ocular syphilis in patients without human immunodeficiency virus (HIV) infection.
METHODS
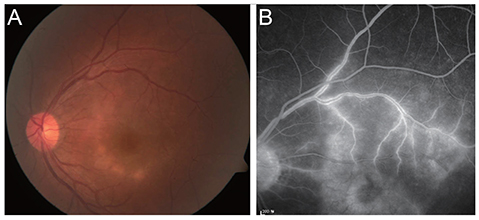
A total of 45 eyes from 39 patients with ocular syphilis confirmed by serologic tests were reviewed retrospectively. The included cases were all non-HIV-infected patients presenting with intraocular inflammation from 2002 to 2014 at Kyung Hee University Hospital. Medical records of 45 eyes were analyzed and included best-corrected visual acuity and ophthalmologic examination findings of the anterior and posterior segments to determine the focus of inflammation. Optical coherence tomography and fluorescein angiography findings as well as both medical and surgical management were also analyzed.
RESULTS
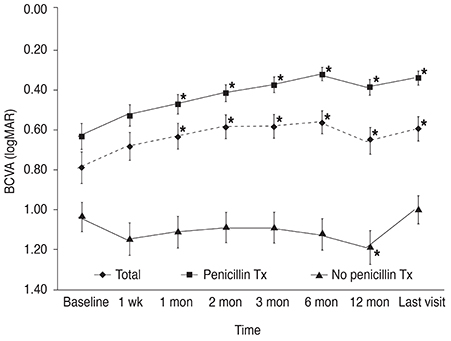
The mean patient age was 61.0 years (range, 37 to 89 years). Bilateral ocular involvement occurred in 6 patients (15.4%), and diagnoses at presentation were most frequently related to posterior uveitis (38%), followed by panuveitis (29%) and optic neuritis (11%). Isolated interstitial keratitis and intermediate uveitis were uncommon (4%, both). Twenty-eight eyes (62.2%) were treated with penicillin, and 11 eyes (24.4%) underwent surgical treatment. The mean baseline best corrected visual acuity was 0.79 ± 0.59 (mean ± standard deviation, logarithm of the minimum angle of resolution) and significantly improved to 0.60 ± 0.63 at the final follow-up after treatment (p = 0.019). Mean visual improvement was significantly greater in the penicillin-treated group (p = 0.001). Visual impairment at the final visit occurred in 11 eyes (24.4%). Among the visual impairment group, 10 eyes (90.1%) had posterior segment-involving uveitis.
CONCLUSIONS
Visual outcomes of treated, non-HIV-related ocular syphilis were favorable regardless of time to presentation. Posterior segment-involving uveitis at presentation was associated with poor visual outcome.
Keyword
MeSH Terms
Figure
Reference
-
1. Aldave AJ, King JA, Cunningham ET Jr. Ocular syphilis. Curr Opin Ophthalmol. 2001; 12:433–441.2. Kiss S, Damico FM, Young LH. Ocular manifestations and treatment of syphilis. Semin Ophthalmol. 2005; 20:161–167.3. Mathew RG, Goh BT, Westcott MC. British Ocular Syphilis Study (BOSS): 2-year national surveillance study of intraocular inflammation secondary to ocular syphilis. Invest Ophthalmol Vis Sci. 2014; 55:5394–5400.4. Centers for Disease Control and Prevention. Disease web statistics system 2014 [Internet]. Cheongju: Centers for Disease Control and Prevention;2014. cited 2014 Dec 30. Available from: http://is.cdc.go.kr/dstat/jsp/stat/stat0001.jsp?disgun=3&discode=67,68,69.5. Jones NP. The Manchester Uveitis Clinic: the first 3000 patients: epidemiology and casemix. Ocul Immunol Inflamm. 2015; 23:118–126.6. Tamesis RR, Foster CS. Ocular syphilis. Ophthalmology. 1990; 97:1281–1287.7. Jones NP. The Manchester Uveitis Clinic: the first 3000 patients, 2: uveitis manifestations, complications, medical and surgical management. Ocul Immunol Inflamm. 2015; 23:127–134.8. Cunningham ET Jr, Eandi CM, Pichi F. Syphilitic uveitis. Ocul Immunol Inflamm. 2014; 22:2–3.9. Barile GR, Flynn TE. Syphilis exposure in patients with uveitis. Ophthalmology. 1997; 104:1605–1609.10. Davis JL. Ocular syphilis. Curr Opin Ophthalmol. 2014; 25:513–518.11. Jumper JM, Machemer R, Gallemore RP, Jaffe GJ. Exudative retinal detachment and retinitis associated with acquired syphilitic uveitis. Retina. 2000; 20:190–194.12. Browning DJ. Posterior segment manifestations of active ocular syphilis, their response to a neurosyphilis regimen of penicillin therapy, and the influence of human immunodeficiency virus status on response. Ophthalmology. 2000; 107:2015–2023.13. Margo CE, Hamed LM. Ocular syphilis. Surv Ophthalmol. 1992; 37:203–220.14. Doris JP, Saha K, Jones NP, Sukthankar A. Ocular syphilis: the new epidemic. Eye (Lond). 2006; 20:703–705.15. Ghanem KG, Moore RD, Rompalo AM, et al. Neurosyphilis in a clinical cohort of HIV-1-infected patients. AIDS. 2008; 22:1145–1151.16. Eandi CM, Neri P, Adelman RA, et al. Acute syphilitic posterior placoid chorioretinitis: report of a case series and comprehensive review of the literature. Retina. 2012; 32:1915–1941.17. Tucker JD, Li JZ, Robbins GK, et al. Ocular syphilis among HIV-infected patients: a systematic analysis of the literature. Sex Transm Infect. 2011; 87:4–8.18. Amaratunge BC, Camuglia JE, Hall AJ. Syphilitic uveitis: a review of clinical manifestations and treatment outcomes of syphilitic uveitis in human immunodeficiency virus-positive and negative patients. Clin Experiment Ophthalmol. 2010; 38:68–74.19. Shalaby IA, Dunn JP, Semba RD, Jabs DA. Syphilitic uveitis in human immunodeficiency virus-infected patients. Arch Ophthalmol. 1997; 115:469–473.20. Li JZ, Tucker JD, Lobo AM, et al. Ocular syphilis among HIV-infected individuals. Clin Infect Dis. 2010; 51:468–471.21. Moradi A, Salek S, Daniel E, et al. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol. 2015; 159:334–343.e1.22. Kwak HD, Kim HW, Lee JE, et al. Clinical manifestations of syphilitic uveitis in the Korean population. J Korean Ophthalmol Soc. 2014; 55:555–562.23. Anshu A, Cheng CL, Chee SP. Syphilitic uveitis: an Asian perspective. Br J Ophthalmol. 2008; 92:594–597.24. Lautenschlager S. Diagnosis of syphilis: clinical and laboratory problems. J Dtsch Dermatol Ges. 2006; 4:1058–1075.25. Hong MC, Sheu SJ, Wu TT, Chuang CT. Ocular uveitis as the initial presentation of syphilis. J Chin Med Assoc. 2007; 70:274–280.26. Puech C, Gennai S, Pavese P, et al. Ocular manifestations of syphilis: recent cases over a 2.5-year period. Graefes Arch Clin Exp Ophthalmol. 2010; 248:1623–1629.27. Reddy S, Cubillan LD, Hovakimyan A, Cunningham ET Jr. Inflammatory ocular hypertension syndrome (IOHS) in patients with syphilitic uveitis. Br J Ophthalmol. 2007; 91:1610–1612.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Unusual Manifestations of Secondary Syphilis Accompanied by Human Immunodeficiency Virus Infection
- A Case of Neurosyphilis with Acute Optic Neuritis and Trochlear Nerve Palsy in Human Immunodeficiency Virus Infected Male
- A Case of Ankylosing Spondylitis in a Patient with Human Immunodeficiency Virus
- Two Cases of Secondary Syphilis Accompanied by Acquired Immunodeficiency Syndrome
- Ocular Inflammation Associated with Systemic Infection