J Korean Soc Radiol.
2016 Oct;75(4):276-284. 10.3348/jksr.2016.75.4.276.
Effectiveness of Virtual Non-Enhanced Images Acquired by Dual-Energy Computed Tomography in Evaluation of Patients with Suspected Acute Appendicitis
- Affiliations
-
- 1Department of Radiology, Wonkwang University Hospital, Iksan, Korea. yjyh@wonkwang.ac.kr
- KMID: 2353678
- DOI: http://doi.org/10.3348/jksr.2016.75.4.276
Abstract
- PURPOSE
To determine whether virtual non-enhanced (VNE) images derived from dual-energy computed tomography (DECT) can replace true non-enhanced (TNE) images in patients with suspected acute appendicitis.
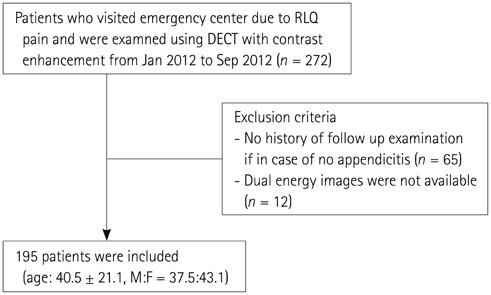
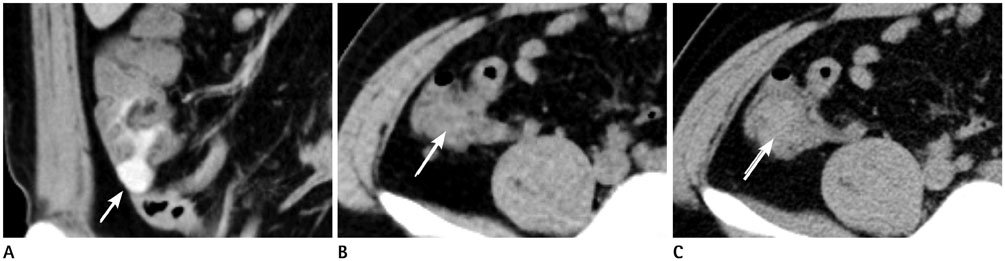
MATERIALS AND METHODS
A total of 195 patients were scanned using DECT. Two radiologists reviewed the VNE set (VNE and portal-phase images) and the TNE set (TNE and portal-phase images), 4 weeks later. Sensitivities and specificities for the diagnosis of acute appendicitis and radiation doses for each set were calculated. Image quality and artifacts in the VNE set were rated on a four point scale (1 = poor-4 = excellent). Size and attenuation of intraperitoneal calcifications were compared in each image.
RESULTS
A total of 114 patients were diagnosed with acute appendicitis by operation. In the VNE set, sensitivity and specificity were 99.1% and 89.9% for reader 1, and 96.6% and 94.8% for reader 2, respectively. In the TNE set, the corresponding values were 96.6% and 94.9% for reader 1, and 94.8% and 92.4% for reader 2, respectively. Among the 87 calcifications detected in the TNE set, 74 calcifications were noted in the VNE set. Mean image quality and artifact were 3.61 and 3.83, respectively. Radiation dose reduction was 48% after excluding the TNE set.
CONCLUSION
Image quality and diagnostic performance of the VNE set were not inferior to those of the TNE set. Replacing TNE images by VNE images can reduce the radiation dose in evaluation of patients with acute appendicitis.
MeSH Terms
Figure
Reference
-
1. Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993-2008. J Surg Res. 2012; 175:185–190.2. Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med. 2011; 154:789–796. W-2913. Pooler BD, Lawrence EM, Pickhardt PJ. Alternative diagnoses to suspected appendicitis at CT. Radiology. 2012; 265:733–742.4. Raman SS, Lu DS, Kadell BM, Vodopich DJ, Sayre J, Cryer H. Accuracy of nonfocused helical CT for the diagnosis of acute appendicitis: a 5-year review. AJR Am J Roentgenol. 2002; 178:1319–1325.5. Krajewski S, Brown J, Phang PT, Raval M, Brown CJ. Impact of computed tomography of the abdomen on clinical outcomes in patients with acute right lower quadrant pain: a meta-analysis. Can J Surg. 2011; 54:43–53.6. Raja AS, Wright C, Sodickson AD, Zane RD, Schiff GD, Hanson R, et al. Negative appendectomy rate in the era of CT: an 18-year perspective. Radiology. 2010; 256:460–465.7. Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007; 357:2277–2284.8. Berrington de González A, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009; 169:2071–2077.9. Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990; 132:910–925.10. Kim SH, Yoon JH, Lee JH, Lim YJ, Kim OH, Ryu JH, et al. Low-dose CT for patients with clinically suspected acute appendicitis: optimal strength of sinogram affirmed iterative reconstruction for image quality and diagnostic performance. Acta Radiol. 2015; 56:899–907.11. Chiu YH, Chen JD, Wang SH, Tiu CM, How CK, Lai JI, et al. Whether intravenous contrast is necessary for CT diagnosis of acute appendicitis in adult ED patients? Acad Radiol. 2013; 20:73–78.12. Kim SY, Lee KH, Kim K, Kim TY, Lee HS, Hwang SS, et al. Acute appendicitis in young adults: low- versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology. 2011; 260:437–445.13. Seo H, Lee KH, Kim HJ, Kim K, Kang SB, Kim SY, et al. Diagnosis of acute appendicitis with sliding slab ray-sum interpretation of low-dose unenhanced CT and standard-dose i.v. contrast-enhanced CT scans. AJR Am J Roentgenol. 2009; 193:96–105.14. Kitagawa M, Kotani T, Miyamoto Y, Kuriu Y, Tsurudome H, Nishi H, et al. Noncontrast and contrast enhanced computed tomography for diagnosing acute appendicitis: a retrospective study for the usefulness. J Radiol Case Rep. 2009; 3:26–33.15. Keyzer C, Cullus P, Tack D, De Maertelaer V, Bohy P, Gevenois PA. MDCT for suspected acute appendicitis in adults: impact of oral and IV contrast media at standard-dose and simulated low-dose techniques. AJR Am J Roentgenol. 2009; 193:1272–1281.16. Fefferman NR, Bomsztyk E, Yim AM, Rivera R, Amodio JB, Pinkney LP, et al. Appendicitis in children: low-dose CT with a phantom-based simulation technique--initial observations. Radiology. 2005; 237:641–646.17. Fefferman NR, Roche KJ, Pinkney LP, Ambrosino MM, Genieser NB. Suspected appendicitis in children: focused CT technique for evaluation. Radiology. 2001; 220:691–695.18. Rao PM, Rhea JT, Novelline RA, McCabe CJ, Lawrason JN, Berger DL, et al. Helical CT technique for the diagnosis of appendicitis: prospective evaluation of a focused appendix CT examination. Radiology. 1997; 202:139–144.19. Malone AJ Jr, Wolf CR, Malmed AS, Melliere BF. Diagnosis of acute appendicitis: value of unenhanced CT. AJR Am J Roentgenol. 1993; 160:763–766.20. Khan N, Anwar Z, Zafar AM, Ahmed F, Ather MH. A comparison of non-contrast CT and intravenous urography in the diagnosis of urolithiasis and obstruction. Afr J Urol. 2012; 18:108–111.21. Anderson SW, Lucey BC, Varghese JC, Soto JA. Accuracy of MDCT in the diagnosis of choledocholithiasis. AJR Am J Roentgenol. 2006; 187:174–180.22. Ishiyama M, Yanase F, Taketa T, Makidono A, Suzuki K, Omata F, et al. Significance of size and location of appendicoliths as exacerbating factor of acute appendicitis. Emerg Radiol. 2013; 20:125–130.23. Tanaka Y, Uchida H, Kawashima H, Fujiogi M, Takazawa S, Deie K, et al. Long-term outcomes of operative versus nonoperative treatment for uncomplicated appendicitis. J Pediatr Surg. 2015; 50:1893–1897.24. Fletcher JG, Takahashi N, Hartman R, Guimaraes L, Huprich JE, Hough DM, et al. Dual-energy and dual-source CT: is there a role in the abdomen and pelvis? Radiol Clin North Am. 2009; 47:41–57.25. Graser A, Johnson TR, Chandarana H, Macari M. Dual energy CT: preliminary observations and potential clinical applications in the abdomen. Eur Radiol. 2009; 19:13–23.26. Song KD, Kim CK, Park BK, Kim B. Utility of iodine overlay technique and virtual unenhanced images for the characterization of renal masses by dual-energy CT. AJR Am J Roentgenol. 2011; 197:W1076–W1082.27. Paulson EK, Coursey CA. CT protocols for acute appendicitis: time for change. AJR Am J Roentgenol. 2009; 193:1268–1271.28. Kamel IR, Goldberg SN, Keogan MT, Rosen MP, Raptopoulos V. Right lower quadrant pain and suspected appendicitis: nonfocused appendiceal CT--review of 100 cases. Radiology. 2000; 217:159–163.29. Singh AK, Hahn PF, Gervais D, Vijayraghavan G, Mueller PR. Dropped appendicolith: CT findings and implications for management. AJR Am J Roentgenol. 2008; 190:707–711.30. Paajanen H, Tainio H, Laato M. A chance of misdiagnosis between acute appendicitis and renal colic. Scand J Urol Nephrol. 1996; 30:363–366.31. Johnson TR, Krauss B, Sedlmair M, Grasruck M, Bruder H, Morhard D, et al. Material differentiation by dual energy CT: initial experience. Eur Radiol. 2007; 17:1510–1517.32. Ascenti G, Siragusa C, Racchiusa S, Ielo I, Privitera G, Midili F, et al. Stone-targeted dual-energy CT: a new diagnostic approach to urinary calculosis. AJR Am J Roentgenol. 2010; 195:953–958.33. Im AL, Lee YH, Bang DH, Yoon KH, Park SH. Dual energy CT in patients with acute abdomen; is it possible for virtual non-enhanced images to replace true non-enhanced images? Emerg Radiol. 2013; 20:475–483.34. Ho LM, Yoshizumi TT, Hurwitz LM, Nelson RC, Marin D, Toncheva G, et al. Dual energy versus single energy MDCT: measurement of radiation dose using adult abdominal imaging protocols. Acad Radiol. 2009; 16:1400–1407.35. Weld KJ, Montiglio C, Morris MS, Bush AC, Cespedes RD. Shock wave lithotripsy success for renal stones based on patient and stone computed tomography characteristics. Urology. 2007; 70:1043–1046.36. Mangold S, Thomas C, Fenchel M, Vuust M, Krauss B, Ketelsen D, et al. Virtual nonenhanced dual-energy CT urography with tin-filter technology: determinants of detection of urinary calculi in the renal collecting system. Radiology. 2012; 264:119–125.37. Phan CM, Yoo AJ, Hirsch JA, Nogueira RG, Gupta R. Differentiation of hemorrhage from iodinated contrast in different intracranial compartments using dual-energy head CT. AJNR Am J Neuroradiol. 2012; 33:1088–1094.38. Ferda J, Novák M, Mírka H, Baxa J, Ferdová E, Bednárová A, et al. The assessment of intracranial bleeding with virtual unenhanced imaging by means of dual-energy CT angiography. Eur Radiol. 2009; 19:2518–2522.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Computed Tomography in the Diagnosis of Acute Appendicitis
- Dual-Energy CT in the Assessment of Mediastinal Lymph Nodes: Comparative Study of Virtual Non-Contrast and True Non-Contrast Images
- Virtual Non-Contrast CT Using Dual-Energy Spectral CT: Feasibility of Coronary Artery Calcium Scoring
- Virtual Monochromatic Image Quality from Dual-Layer Dual-Energy Computed Tomography for Detecting Brain Tumors
- Dual-Energy CT: New Horizon in Medical Imaging