Korean J Radiol.
2013 Jun;14(3):532-539. 10.3348/kjr.2013.14.3.532.
Dual-Energy CT in the Assessment of Mediastinal Lymph Nodes: Comparative Study of Virtual Non-Contrast and True Non-Contrast Images
- Affiliations
-
- 1Department of Radiology, School of Medicine, Ewha Womans University, Seoul 158-710, Korea.
- 2Department of Radiology, School of Medicine, Ewha Womans University, Mokdong Hospital, Seoul 158-710, Korea. yookkim@ewha.ac.kr
- 3Department of Radiology, Kepco Medical Center, Seoul 132-703, Korea.
- KMID: 1705471
- DOI: http://doi.org/10.3348/kjr.2013.14.3.532
Abstract
OBJECTIVE
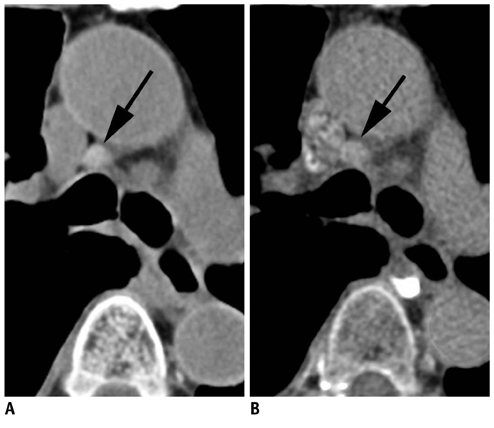
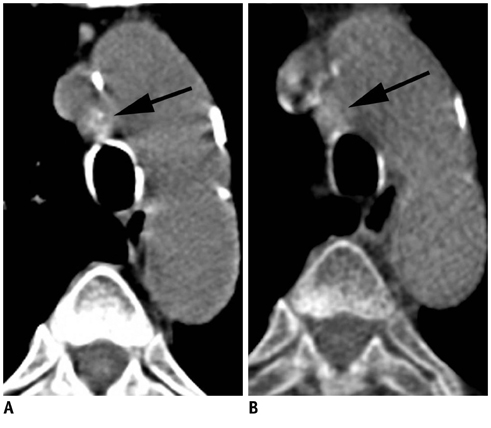
To evaluate the reliability of virtual non-contrast (VNC) images reconstructed from contrast-enhanced, dual-energy scans compared with true non-contrast (TNC) images in the assessment of high CT attenuation or calcification of mediastinal lymph nodes.
MATERIALS AND METHODS
A total of 112 mediastinal nodes from 45 patients who underwent non-contrast and dual-energy contrast-enhanced scans were analyzed. Node attenuation in TNC and VNC images was compared both objectively, using computed tomography (CT) attenuation, and subjectively, via visual scoring (0, attenuation < or = the aorta; 1, > the aorta; 2, calcification). The relationship among attenuation difference between TNC and VNC images, CT attenuation in TNC images, and net contrast enhancement (NCE) was analyzed.
RESULTS
CT attenuation in TNC and VNC images showed moderate agreement (intraclass correlation coefficient, 0.612). The mean absolute difference was 7.8 +/- 7.6 Hounsfield unit (HU) (range, 0-36 HU), and the absolute difference was equal to or less than 10 HU in 65.2% of cases (73/112). Visual scores in TNC and VNC images showed fair agreement (kappa value, 0.335). Five of 16 nodes (31.3%) which showed score 1 (n = 15) or 2 (n = 1) in TNC images demonstrated score 1 in VNC images. The TNC-VNC attenuation difference showed a moderate positive correlation with CT attenuation in TNC images (partial correlation coefficient [PCC] adjusted by NCE: 0.455) and a weak negative correlation with NCE (PCC adjusted by CT attenuation in TNC: -0.245).
CONCLUSION
VNC images may be useful in the evaluation of mediastinal lymph nodes by providing additional information of high CT attenuation of nodes, although it is underestimated compared with TNC images.
MeSH Terms
Figure
Reference
-
1. Kim YK, Lee KS, Kim BT, Choi JY, Kim H, Kwon OJ, et al. Mediastinal nodal staging of nonsmall cell lung cancer using integrated 18F-FDG PET/CT in a tuberculosis-endemic country: diagnostic efficacy in 674 patients. Cancer. 2007. 109:1068–1077.2. Li M, Wu N, Liu Y, Zheng R, Liang Y, Zhang W, et al. Regional nodal staging with 18F-FDG PET-CT in non-small cell lung cancer: additional diagnostic value of CT attenuation and dual-time-point imaging. Eur J Radiol. 2012. 81:1886–1890.3. Liao CY, Chen JH, Liang JA, Yeh JJ, Kao CH. Meta-analysis study of lymph node staging by 18 F-FDG PET/CT scan in non-small cell lung cancer: comparison of TB and non-TB endemic regions. Eur J Radiol. 2012. 81:3518–3523.4. Toba H, Kondo K, Otsuka H, Takizawa H, Kenzaki K, Sakiyama S, et al. Diagnosis of the presence of lymph node metastasis and decision of operative indication using fluorodeoxyglucose-positron emission tomography and computed tomography in patients with primary lung cancer. J Med Invest. 2010. 57:305–313.5. Iskender I, Kadioglu SZ, Cosgun T, Kapicibasi HO, Sagiroglu G, Kosar A, et al. False-positivity of mediastinal lymph nodes has negative effect on survival in potentially resectable non-small cell lung cancer. Eur J Cardiothorac Surg. 2012. 41:874–879.6. Shim SS, Lee KS, Kim BT, Chung MJ, Lee EJ, Han J, et al. Non-small cell lung cancer: prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology. 2005. 236:1011–1019.7. Chae EJ, Song JW, Seo JB, Krauss B, Jang YM, Song KS. Clinical utility of dual-energy CT in the evaluation of solitary pulmonary nodules: initial experience. Radiology. 2008. 249:671–681.8. Coursey CA, Nelson RC, Boll DT, Paulson EK, Ho LM, Neville AM, et al. Dual-energy multidetector CT: how does it work, what can it tell us, and when can we use it in abdominopelvic imaging? Radiographics. 2010. 30:1037–1055.9. Kang MJ, Park CM, Lee CH, Goo JM, Lee HJ. Dual-energy CT: clinical applications in various pulmonary diseases. Radiographics. 2010. 30:685–698.10. Huda W, Scalzetti EM, Levin G. Technique factors and image quality as functions of patient weight at abdominal CT. Radiology. 2000. 217:430–435.11. Darling GE, Maziak DE, Inculet RI, Gulenchyn KY, Driedger AA, Ung YC, et al. Positron emission tomography-computed tomography compared with invasive mediastinal staging in non-small cell lung cancer: results of mediastinal staging in the early lung positron emission tomography trial. J Thorac Oncol. 2011. 6:1367–1372.12. De Cecco CN, Buffa V, Fedeli S, Luzietti M, Vallone A, Ruopoli R, et al. Dual energy CT (DECT) of the liver: conventional versus virtual unenhanced images. Eur Radiol. 2010. 20:2870–2875.13. Chandarana H, Godoy MC, Vlahos I, Graser A, Babb J, Leidecker C, et al. Abdominal aorta: evaluation with dual-source dual-energy multidetector CT after endovascular repair of aneurysms--initial observations. Radiology. 2008. 249:692–700.14. Graser A, Johnson TR, Hecht EM, Becker CR, Leidecker C, Staehler M, et al. Dual-energy CT in patients suspected of having renal masses: can virtual nonenhanced images replace true nonenhanced images? Radiology. 2009. 252:433–440.15. Stolzmann P, Frauenfelder T, Pfammatter T, Peter N, Scheffel H, Lachat M, et al. Endoleaks after endovascular abdominal aortic aneurysm repair: detection with dual-energy dual-source CT. Radiology. 2008. 249:682–691.16. Toepker M, Moritz T, Krauss B, Weber M, Euller G, Mang T, et al. Virtual non-contrast in second-generation, dual-energy computed tomography: reliability of attenuation values. Eur J Radiol. 2012. 81:e398–e405.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Virtual Monochromatic Image Quality from Dual-Layer Dual-Energy Computed Tomography for Detecting Brain Tumors
- Comparison of True and Virtual Non-Contrast Images of Liver Obtained with Single-Source Twin Beam and Dual-Source Dual-Energy CT
- Supraclavicular Lymph Node Metastasis from Various Malignancies: Assessment with 18F-Fluorodeoxyglucose Positron Emission Tomography/CT, Contrast-Enhanced CT and Ultrasound
- Dual-Energy CT: New Horizon in Medical Imaging
- Virtual Non-Contrast CT Using Dual-Energy Spectral CT: Feasibility of Coronary Artery Calcium Scoring