Clin Exp Otorhinolaryngol.
2016 Sep;9(3):226-232. 10.21053/ceo.2015.01375.
Assessment of Change in Palatal Sensation in Obstructive Sleep Apnea Patients by Using Two-Point Palatal Discrimination
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Konkuk University School of Medicine, Seoul, Korea. entalk@kuh.ac.kr
- 2Department of Biomedical Engineering, Konkuk University School of Medicine, Seoul, Korea.
- KMID: 2353620
- DOI: http://doi.org/10.21053/ceo.2015.01375
Abstract
OBJECTIVES
Patients with obstructive sleep apnea syndrome (OSAS) have impaired responses to inspiratory resistive loading during sleep. This may be due, in part, to a change in the upper airway sensation. Therefore, we hypothesized that patients with OSAS have diminished upper airway sensation due to snoring.
METHODS
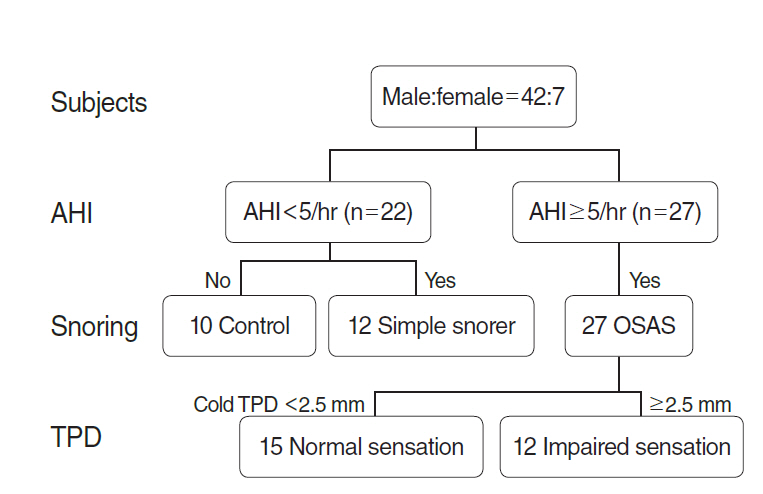
A total of 53 participants were selected based on clinical evaluation and polysomnography. Two-point discrimination was measured with modified calipers in the tongue and soft palate.
RESULTS
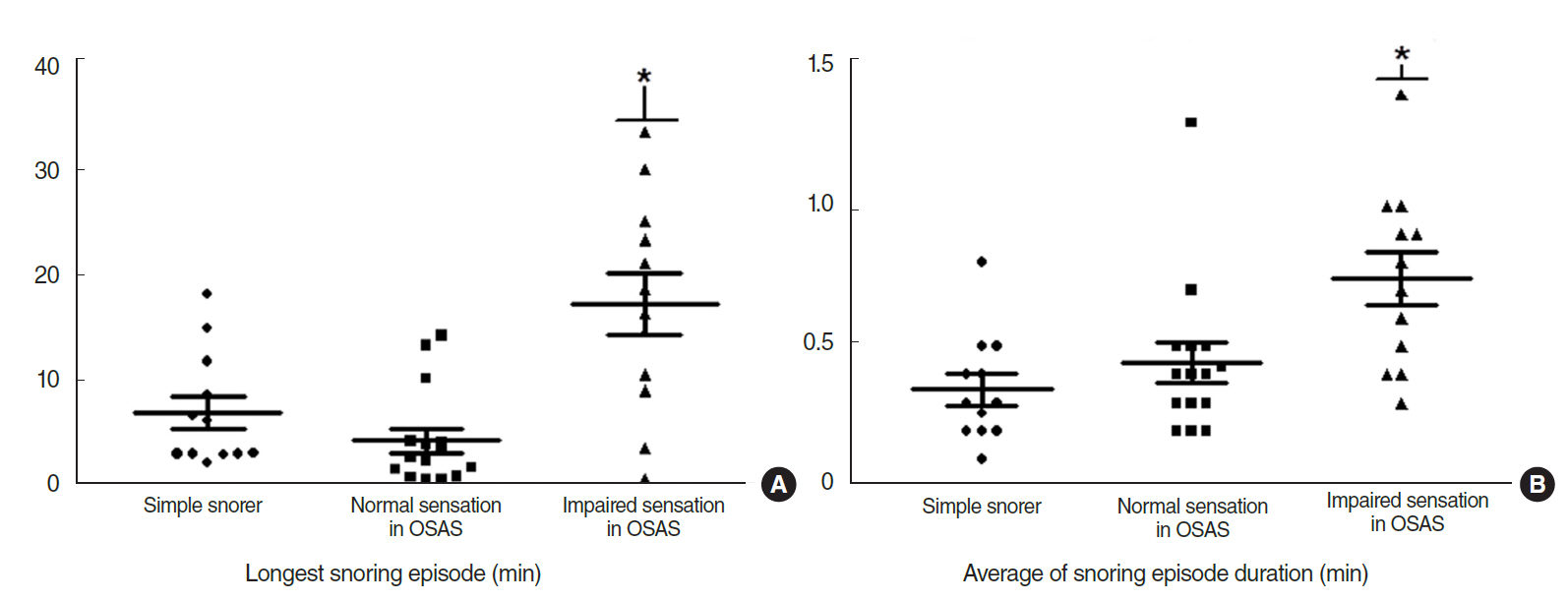
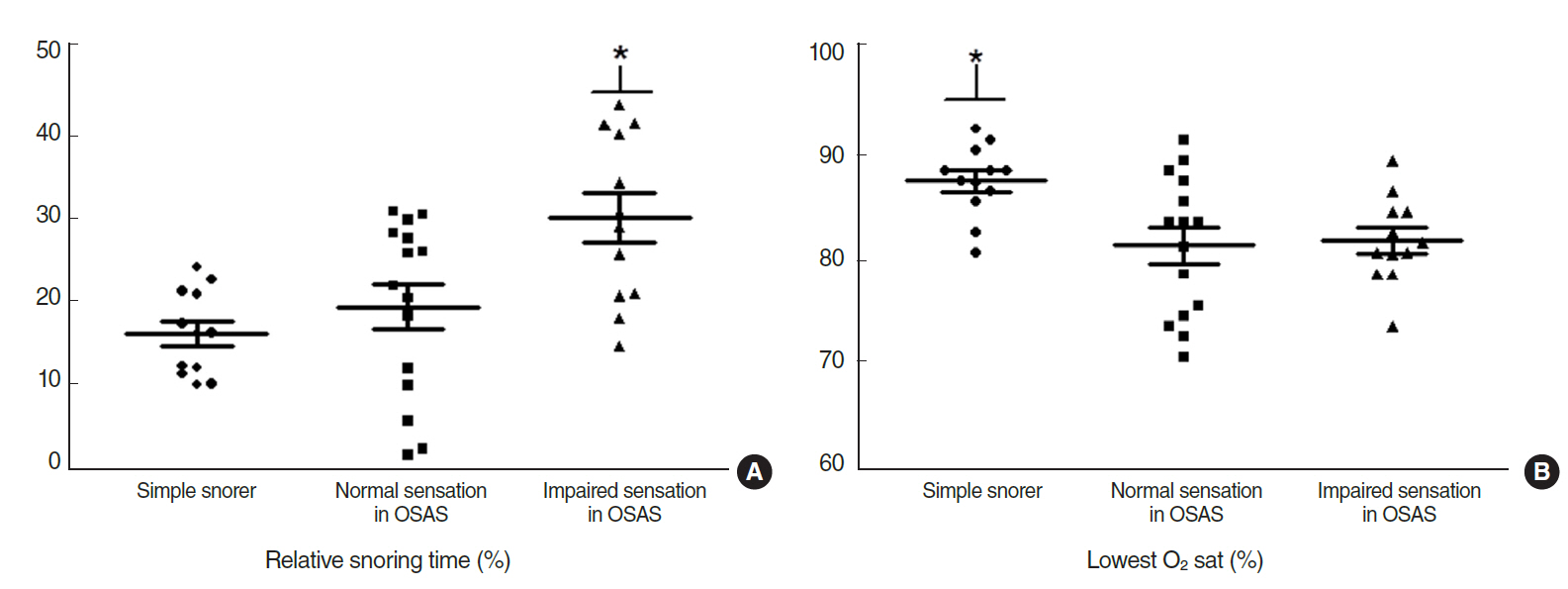
A total of 10 participants were included in the control group, 12 participants in the simple snoring group, and 27 participants in the OSAS group. There were 12 patients in the impaired sensation group of the OSAS group. On comparing polysomnography, patients with impairment of their palatal sensory input in two-point discrimination (TPD) had a more protracted duration of the longest snoring episode than those with simple snoring and normal sensation. Patients with decreased sensory input in TPD had longer average duration of snoring episodes and relative snoring time than those with simple snoring and normal sensory input in cold uvular TPD. Comparison of the cold uvular TPD for normal sensation and impaired sensation in patients with OSAS after treatment showed a different trend.
CONCLUSION
Impaired sensation of the soft palate was correlated with the longest snoring episode duration, average snoring episode duration, and relative snoring time. It is helpful in detecting the early stage of neural degradation in OSAS patients by assessing snoring components of polysomnography and TPD in the soft palate.
MeSH Terms
Figure
Reference
-
1. Silva GE, An MW, Goodwin JL, Shahar E, Redline S, Resnick H, et al. Longitudinal evaluation of sleep-disordered breathing and sleep symptoms with change in quality of life: the Sleep Heart Health Study (SHHS). Sleep. 2009; Aug. 32(8):1049–57.
Article2. Berger G, Berger R, Oksenberg A. Progression of snoring and obstructive sleep apnoea: the role of increasing weight and time. Eur Respir J. 2009; Feb. 33(2):338–45.
Article3. Svanborg E. Impact of obstructive apnea syndrome on upper airway respiratory muscles. Respir Physiol Neurobiol. 2005; Jul. 147(2-3):263–72.
Article4. Friberg D, Ansved T, Borg K, Carlsson-Nordlander B, Larsson H, Svanborg E. Histological indications of a progressive snorers disease in an upper airway muscle. Am J Respir Crit Care Med. 1998; Feb. 157(2):586–93.
Article5. Hagander L, Harlid R, Svanborg E. Quantitative sensory testing in the oropharynx: a means of showing nervous lesions in patients with obstructive sleep apnea and snoring. Chest. 2009; Aug. 136(2):481–9.6. Kimoff RJ, Sforza E, Champagne V, Ofiara L, Gendron D. Upper airway sensation in snoring and obstructive sleep apnea. Am J Respir Crit Care Med. 2001; Jul. 164(2):250–5.
Article7. Guilleminault C, Li K, Chen NH, Poyares D. Two-point palatal discrimination in patients with upper airway resistance syndrome, obstructive sleep apnea syndrome, and normal control subjects. Chest. 2002; Sep. 122(3):866–70.
Article8. Nguyen AT, Jobin V, Payne R, Beauregard J, Naor N, Kimoff RJ. Laryngeal and velopharyngeal sensory impairment in obstructive sleep apnea. Sleep. 2005; May. 28(5):585–93.
Article9. Choi JH, Jun YJ, Kim TH, Lee HM, Lee SH, Kwon SY, Choi H, et al. Effect of isolated uvulopalatopharyngoplasty on subjective obstructive sleep apnea symptoms. Clin Exp Otorhinolaryngol. 2013; Sep. 6(3):161–5.
Article10. Guilleminault C, Poyares D, Palombini L, Koester U, Pelin Z, Black J. Variability of respiratory effort in relation to sleep stages in normal controls and upper airway resistance syndrome patients. Sleep Med. 2001; Sep. 2(5):397–405.
Article11. Shy ME, Frohman EM, So YT, Arezzo JC, Cornblath DR, Giuliani MJ, et al. Quantitative sensory testing: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2003; Mar. 60(6):898–904.
Article12. Tapia IE, Bandla P, Traylor J, Karamessinis L, Huang J, Marcus CL. Upper airway sensory function in children with obstructive sleep apnea syndrome. Sleep. 2010; Jul. 33(7):968–72.
Article13. Akobeng AK. Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr. 2007; May. 96(5):644–7.
Article14. Mackenzie RA, Skuse NF, Lethlean AK. A micro-electrode study of peripheral neuropathy in man. Part 1. Responses to single graded stimuli. J Neurol Sci. 1977; Nov. 34(2):157–74.15. Friberg D, Gazelius B, Hokfelt T, Nordlander B. Abnormal afferent nerve endings in the soft palatal mucosa of sleep apnoics and habitual snorers. Regul Pept. 1997; Jul. 71(1):29–36.
Article16. Friberg D, Gazelius B, Lindblad LE, Nordlander B. Habitual snorers and sleep apnoics have abnormal vascular reactions of the soft palatal mucosa on afferent nerve stimulation. Laryngoscope. 1998; Mar. 108(3):431–6.
Article17. Sunnergren O, Brostrom A, Svanborg E. Soft palate sensory neuropathy in the pathogenesis of obstructive sleep apnea. Laryngoscope. 2011; Feb. 121(2):451–6.
Article18. Takeuchi T, Futatsuka M, Imanishi H, Yamada S. Pathological changes observed in the finger biopsy of patients with vibration-induced white finger. Scand J Work Environ Health. 1986; Aug. 12(4 Spec No):280–3.
Article19. Stromberg T, Dahlin LB, Lundborg G. Hand problems in 100 vibration-exposed symptomatic male workers. J Hand Surg Br. 1996; Jun. 21(3):315–9.20. Virokannas H. Dose-response relation between exposure to two types of hand-arm vibration and sensorineural perception of vibration. Occup Environ Med. 1995; May. 52(5):332–6.
Article21. Lugaresi E, Coccagna G, Cirignotta F, Farneti P, Gallassi R, Di Donato G, et al. Breathing during sleep in man in normal and pathological conditions. Adv Exp Med Biol. 1978; May. 99:35–45.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Palatal Implants on Snoring and Obstructive Sleep Apnea Syndrome
- Evaluation of the Obstructive Site in Patients with Obstructive Sleep Apnea Using Sleep Endoscopy
- The relationship between the predictors of obstructive sleep apnea and difficult intubation
- Palatal Implants for Persistent Snoring and Mild Obstructive Sleep Apnea After Laser-Assisted Uvulopalatoplasty
- Clinical Safety of PMR(Palatal Muscle Resection) In Which Performed OSAS Patients