J Korean Ophthalmol Soc.
2016 Sep;57(9):1465-1471. 10.3341/jkos.2016.57.9.1465.
Adult-Onset Asthma and Periocular Xanthogranuloma in a 75-Year-Old Man
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ydkimoph@skku.edu
- 2Department of Ophthalmology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 2351879
- DOI: http://doi.org/10.3341/jkos.2016.57.9.1465
Abstract
- PURPOSE
Adult xanthogranulomatous disease of the orbit including adult-onset asthma and periocular xanthogranuloma is rare. To the best of the author's knowledge, adult-onset asthma and periocular xanthogranuloma have not been previously reported in Korea.
CASE SUMMARY
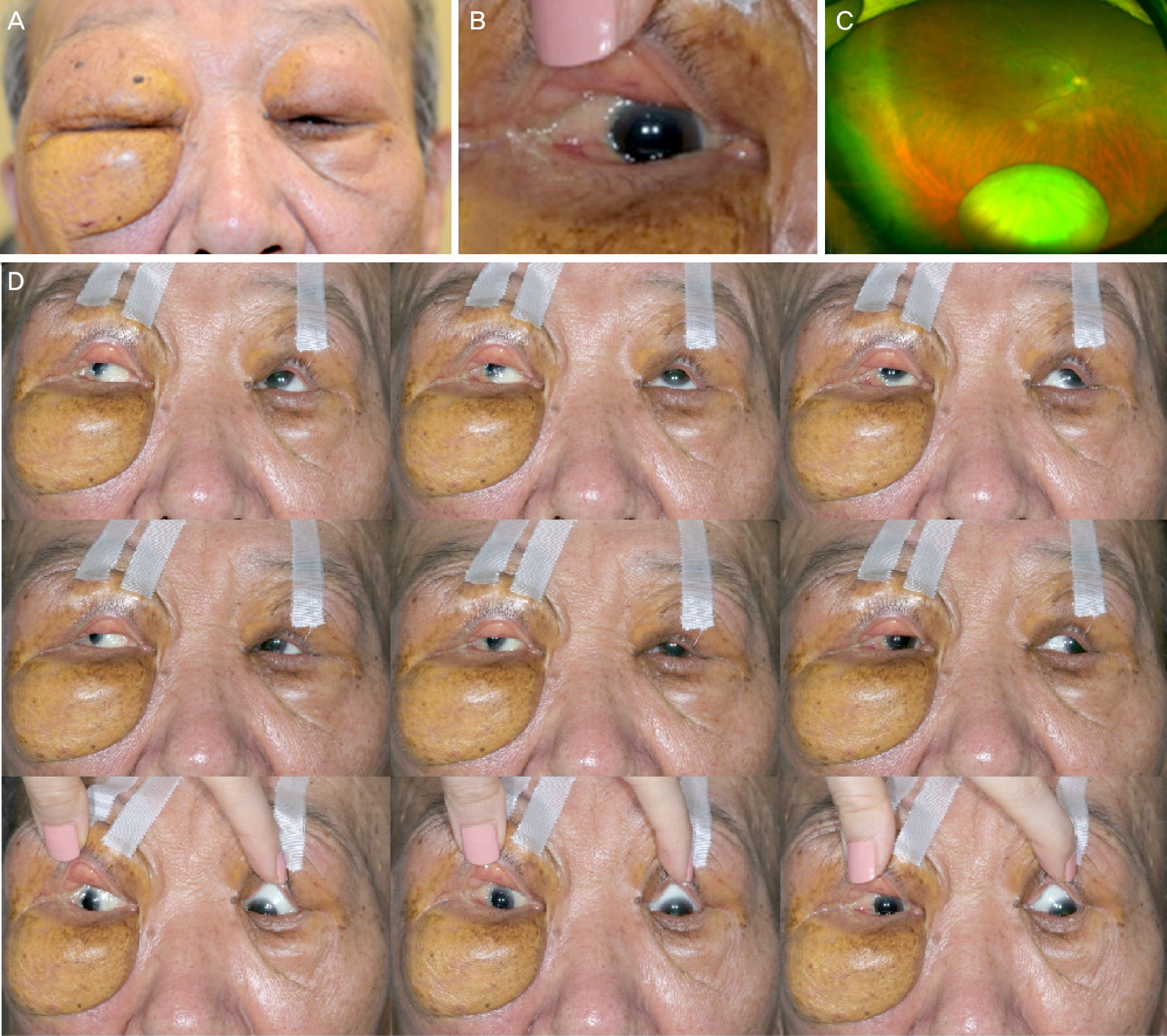
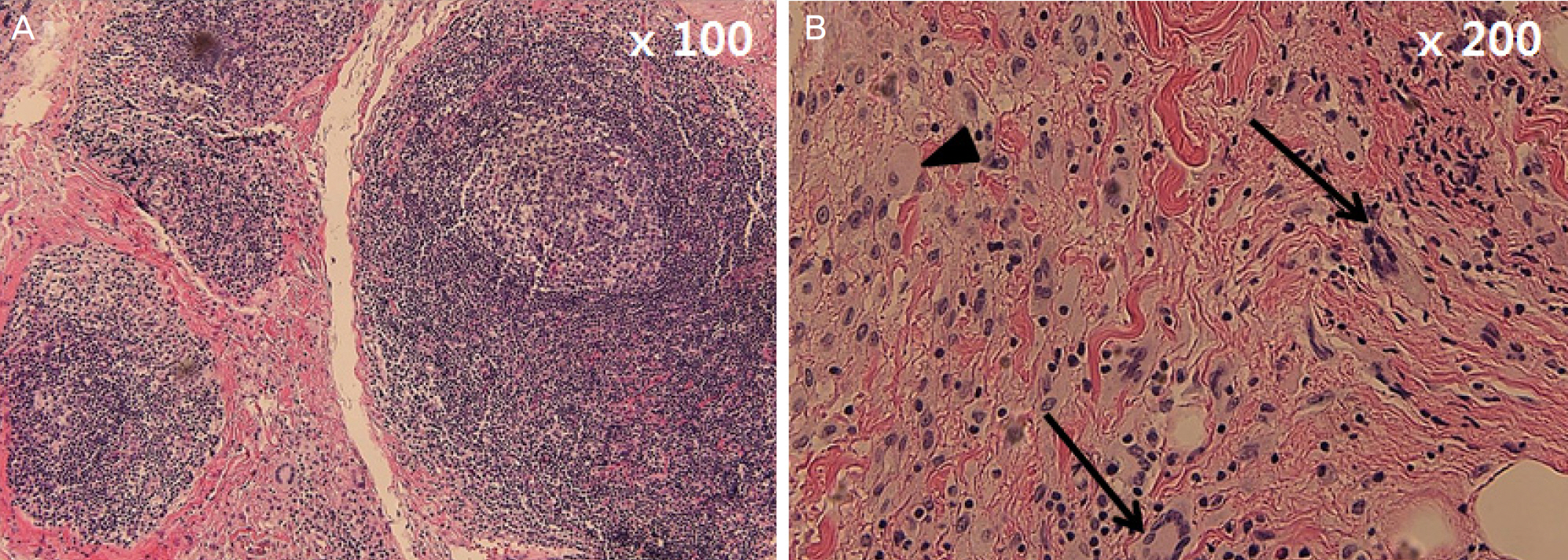
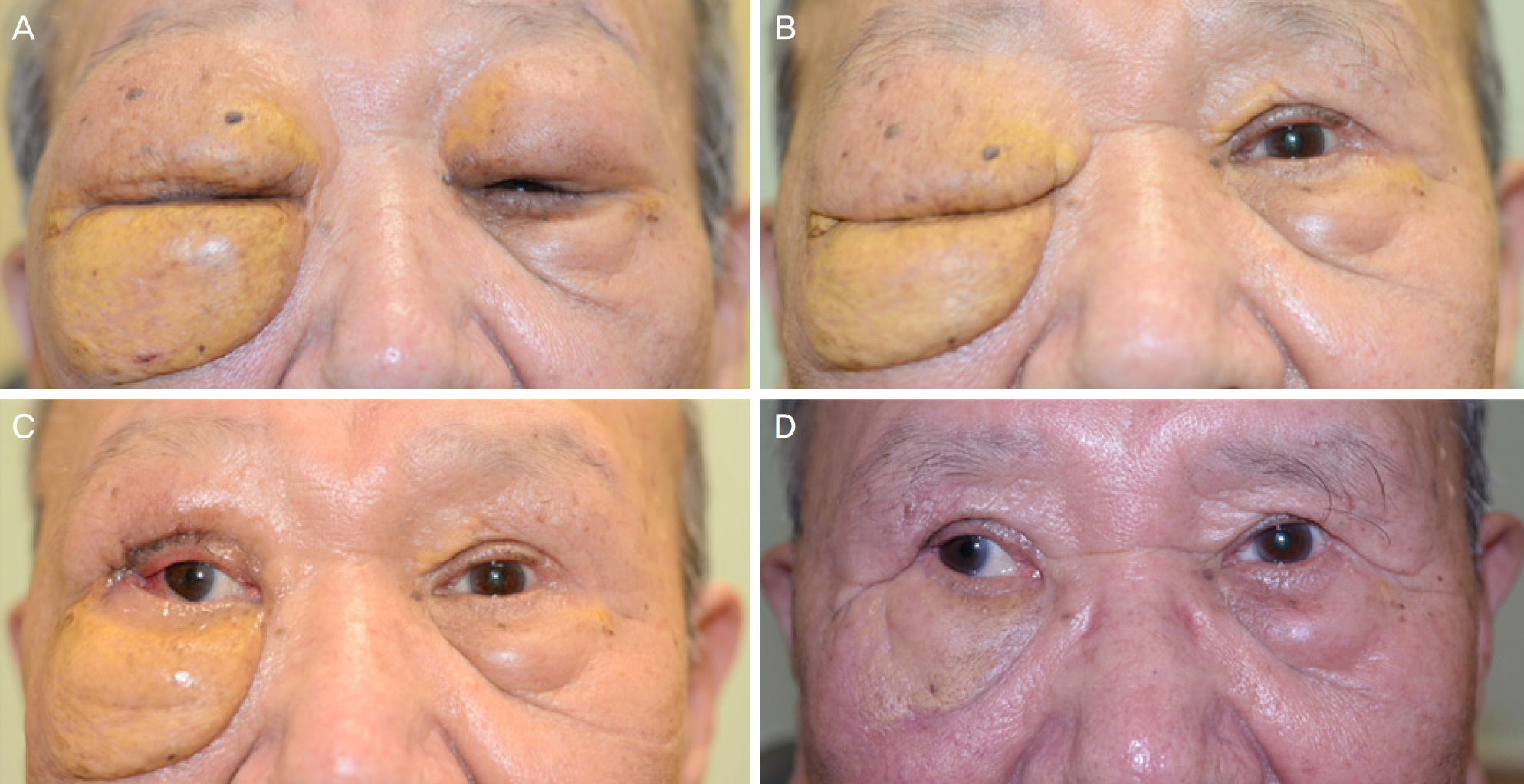
A 75-year-old man presented with a 15-year history of progressive bilateral yellowish eyelid mass. He had a history of adult-onset asthma diagnosed 13 years ago. On ocular examination, there were firm yellowish bilateral eyelid masses and ptosis markedly on the right eye. Exophthalmos was noted in the right eye. There were exotropia, hypertropia, and gaze restriction of the right eye. Orbit magnetic resonance imaging demonstrated an ill-defined bilateral infiltrative orbital mass extending to the lid, lacrimal gland, and sinuses. A right orbital mass extended to the posterior orbit. Enlargement of extraocular muscles was also noted in the right eye. Left upper eyelid mass debulking surgery was performed. A combination therapy of azathioprine and prednisolone was started. Mass debulking surgeries of the right upper and lower eyelids were performed.
CONCLUSIONS
Adult-onset asthma and periocular xanthogranuloma is known as a refractory disease. Combination therapy with azathioprine and steroid therapy with mass debulking surgery is a good treatment option for adult-onset asthma and periocular xanthogranuloma.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Bijlsma WR, van den Bosch WA, van Daele PL, Paridaens D. Azathioprine and prednisone combination treatment for adult periocular and orbital xanthogranulomatous disease. Acta Ophthalmol. 2011; 89:e278–82.
Article2. Jakobiec FA, Mills MD, Hidayat AA, et al. Periocular xanthogra-nulomas associated with severe adult-onset asthma. Trans Am Ophthalmol Soc. 1993; 91:99–125. discussion 125–9.3. Guo J, Wang J. Adult orbital xanthogranulomatous disease: review of the literature. Arch Pathol Lab Med. 2009; 133:1994–7.
Article4. Alper MG, Zimmerman LE, Piana FG. Orbital manifestations of Erdheim-Chester disease. Trans Am Ophthalmol Soc. 1983; 81:64–85.5. Robertson DM, Winkelmann RK. Ophthalmic features of necrobiotic xanthogranuloma with paraproteinemia. Am J Ophthalmol. 1984; 97:173–83.
Article6. Sivak-Callcott JA, Rootman J, Rasmussen SL, et al. Adult xanthogranulomatous disease of the orbit and ocular adnexa: new immunohistochemical findings and clinical review. Br J Ophthalmol. 2006; 90:602–8.
Article7. Hammond MD, Niemi EW, Ward TP, Eiseman AS. Adult orbital xanthogranuloma with associated adult-onset asthma. Ophthal Plast Reconstr Surg. 2004; 20:329–32.
Article8. Murray D, Marshall M, England E, et al. Erdheim-Chester disease. Clin Radiol. 2001; 56:481–4.
Article9. Elner VM, Mintz R, Demirci H, Hassan AS. Local corticosteroid treatment of eyelid and orbital xanthogranuloma. Trans Am Ophthalmol Soc. 2005; 103:69–73. discussion 73–4.
Article10. Shams PN, Rasmussen SL, Dolman PJ. Adult-onset asthma abdominal with simultaneous conjunctival, eyelid, and orbital xanthog-ranulomatosis responsive to systemic immunosuppression. Ophthal Plast Reconstr Surg. 2015; 31:e162–3.11. Papagoras C, Kitsos G, Voulgari PV, et al. Periocular xanthogranuloma: a forgotten entity? Clin Ophthalmol. 2010; 4:105–10.12. Hayden A, Wilson DJ, Rosenbaum JT. Management of orbital xanthogranuloma with methotrexate. Br J Ophthalmol. 2007; 91:434–6.
Article13. Ho VH, Chevez-Barrios P, Jorgensen JL, et al. Receptor expression in orbital inflammatory syndromes and implications for targeted therapy. Tissue Antigens. 2007; 70:105–9.
Article14. Chung SJ, Lew H. Adult orbital xanthogranulomatous disease in a 42-year-old woman. J Korean Ophthalmol Soc. 2011; 52:975–8.
Article15. Choi HJ, Kwon HJ, Kim HY. A case of posttraumatic necrobiotic xanthogranuloma of the orbit. J Korean Ophthalmol Soc. 2008; 49:677–80.
Article