J Korean Med Sci.
2015 Nov;30(11):1631-1637. 10.3346/jkms.2015.30.11.1631.
Is Radical Perineal Prostatectomy a Viable Therapeutic Option for Intermediate- and High-risk Prostate Cancer?
- Affiliations
-
- 1Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. hanchoi@skku.edu
- 2Research Institute for Future Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2351114
- DOI: http://doi.org/10.3346/jkms.2015.30.11.1631
Abstract
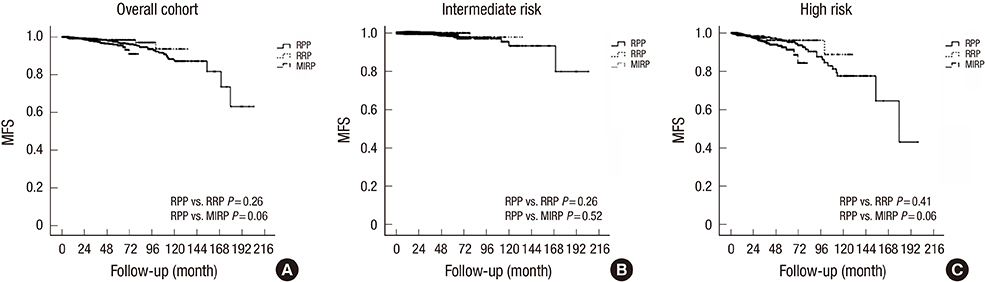
- The aim of this study was to investigate a single-institution experience with radical perineal prostatectomy (RPP), radical retropubic prostatectomy (RRP) and minimally invasive radical prostatectomy (MIRP) with respect to onco-surgical outcomes in patients with intermediate-risk (IR; PSA 10-20 ng/mL, biopsy Gleason score bGS 7 or cT2b-2c) and high-risk (HR; PSA >20 ng/mL, bGS > or =8, or > or =cT3) prostate cancer (PCa). We retrospectively reviewed data from 2,581 men who underwent radical prostatectomy for IR and HR PCa (RPP, n = 689; RRP, n = 402; MIRP, n = 1,490 [laparoscopic, n = 206; robot-assisted laparoscopic, n = 1,284]). The proportion of HR PCa was 40.3%, 46.8%, and 49.5% in RPP, RRP, and MIRP (P < 0.001), respectively. The positive surgical margin rate was 23.8%, 26.1%, and 18.7% (P = 0.002) overall, 17.5%, 17.8%, and 8.8% (P < 0.001) for pT2 disease and 41.9%, 44.4%, and 40.0% (P = 0.55) for pT3 disease in men undergoing RPP, RRP, and MIRP, respectively. Biochemical recurrence-free survival rates among RPP, RRP, and MIRP were 73.0%, 70.1%, and 76.8%, respectively, at 5 yr (RPP vs. RPP, P = 0.02; RPP vs. MIRP, P = 0.23). Furthermore, comparable 5-yr metastases-free survival rates were demonstrated for specific surgical approaches (RPP vs. RPP, P = 0.26; RPP vs. MIRP, P = 0.06). RPP achieved acceptable oncological control for IR and HR PCa.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Disease-Free Survival
Humans
Laparoscopy/*utilization
Male
Middle Aged
Minimally Invasive Surgical Procedures/*utilization
Perineum/*surgery
Prevalence
Prostatectomy/*utilization
Prostatic Neoplasms/diagnosis/*epidemiology/*surgery
Republic of Korea/epidemiology
Retrospective Studies
Risk Factors
Treatment Outcome
Figure
Reference
-
1. Rodrigues G, Warde P, Pickles T, Crook J, Brundage M, Souhami L, Lukka H. Genitourinary Radiation Oncologists of Canada. Pre-treatment risk stratification of prostate cancer patients: a critical review. Can Urol Assoc J. 2012; 6:121–127.2. Cooperberg MR, Lubeck DP, Mehta SS, Carroll PR. CaPSURE. Time trends in clinical risk stratification for prostate cancer: implications for outcomes (data from CaPSURE). J Urol. 2003; 170:S21–S25.3. Ischia J, Gleave M. Radical prostatectomy in high-risk prostate cancer. Int J Urol. 2013; 20:290–300.4. Eggener SE, Scardino PT, Walsh PC, Han M, Partin AW, Trock BJ, Feng Z, Wood DP, Eastham JA, Yossepowitch O, et al. Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J Urol. 2011; 185:869–875.5. Young HH. The early diagnosis and radical cure of carcinoma of the prostate: being a study of 40 cases and presentation of a radical operation which was carried out in 4 cases. Bull Johns Hopkins Hosp. 1905; 16:315–321.6. Nargund VH, Zaman F. Radical prostatectomy: too soon to abandon the perineal approach? Nat Rev Urol. 2011; 8:179–180.7. Comploj E, Palermo S, Trenti E, Martini T, Lodde M, Mian C, Mazzoleni G, Pycha A. Radical perineal prostatectomy: an outdated procedure? Int J Surg. 2011; 9:400–403.8. Gianino MM, Galzerano M, Martin B, Chiadò Piat S, Gontero P. Costs in surgical techniques for radical prostatectomy: a review of the current state. Urol Int. 2012; 88:1–5.9. Mirza M, Art K, Wineland L, Tawfik O, Thrasher JB. A comparison of radical perineal, radical retropubic, and robot-assisted laparoscopic prostatectomies in a single surgeon series. Prostate Cancer. 2011; 2011:878323.10. Eliya F, Kernen K, Gonzalez J, Peters K, Ibrahim I, Petzel K. Radical perineal prostatectomy: a learning curve? Int Urol Nephrol. 2011; 43:139–142.11. Briganti A, Larcher A, Abdollah F, Capitanio U, Gallina A, Suardi N, Bianchi M, Sun M, Freschi M, Salonia A, et al. Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol. 2012; 61:480–487.12. Kawakami J, Meng MV, Sadetsky N, Latini DM, Duchane J, Carroll PR. CaPSURE Investigators. Changing patterns of pelvic lymphadenectomy for prostate cancer: results from CaPSURE. J Urol. 2006; 176:1382–1386.13. Feifer AH, Elkin EB, Lowrance WT, Denton B, Jacks L, Yee DS, Coleman JA, Laudone VP, Scardino PT, Eastham JA. Temporal trends and predictors of pelvic lymph node dissection in open or minimally invasive radical prostatectomy. Cancer. 2011; 117:3933–3942.14. Catalona WJ, Smith DS. Cancer recurrence and survival rates after anatomic radical retropubic prostatectomy for prostate cancer: intermediate-term results. J Urol. 1998; 160:2428–2434.15. Abdollah F, Schmitges J, Sun M, Tian Z, Briganti A, Shariat SF, Perrotte P, Montorsi F, Karakiewicz PI. A critical assessment of the value of lymph node dissection at radical prostatectomy: A population-based study. Prostate. 2011; 71:1587–1594.16. Mohler J, Bahnson RR, Boston B, Busby JE, D'Amico A, Eastham JA, Enke CA, George D, Horwitz EM, Huben RP, et al. NCCN clinical practice guidelines in oncology: prostate cancer. J Natl Compr Canc Netw. 2010; 8:162–200.17. Lezin MS, Cherrie R, Cattolica EV. Comparison of laparoscopic and minilaparotomy pelvic lymphadenectomy for prostate cancer staging in a community practice. Urology. 1997; 49:60–63.18. Parra RO, Boullier JA, Rauscher JA, Cummings JM. The value of laparoscopic lymphadenectomy in conjunction with radical perineal or retropubic prostatectomy. J Urol. 1994; 151:1599–1602.19. Pierorazio PM, Guzzo TJ, Han M, Bivalacqua TJ, Epstein JI, Schaeffer EM, Schoenberg M, Walsh PC, Partin AW. Long-term survival after radical prostatectomy for men with high Gleason sum in pathologic specimen. Urology. 2010; 76:715–721.20. Herrmann TR, Rabenalt R, Stolzenburg JU, Liatsikos EN, Imkamp F, Tezval H, Gross AJ, Jonas U, Burchardt M. Oncological and functional results of open, robot-assisted and laparoscopic radical prostatectomy: does surgical approach and surgical experience matter? World J Urol. 2007; 25:149–160.21. Boccon-Gibod L. Radical prostatectomy: open? Laparoscopic? Robotic? Eur Urol. 2006; 49:598–599.22. Salomon L, Levrel O, de la Taille A, Anastasiadis AG, Saint F, Zaki S, Vordos D, Cicco A, Olsson LE, Hoznek A, et al. Radical prostatectomy by the retropubic, perineal and laparoscopic approach: 12 years of experience in one center. Eur Urol. 2002; 42:104–110.23. Ahlering TE, Woo D, Eichel L, Lee DI, Edwards R, Skarecky DW. Robot-assisted versus open radical prostatectomy: a comparison of one surgeon's outcomes. Urology. 2004; 63:819–822.24. Busch J, Magheli A, Leva N, Hinz S, Ferrari M, Friedersdorff F, Fuller TF, Miller K, Gonzalgo ML. Matched comparison of outcomes following open and minimally invasive radical prostatectomy for high-risk patients. World J Urol. 2014; 32:1411–1416.25. Furubayashi N, Nakamura M, Hishikawa K, Fukuda A, Matsumoto T, Nishiyama K, Yamanaka T, Hasegawa Y. Radical prostatectomy as radical cure of prostate cancer in a high-risk group: A single-institution experience. Mol Clin Oncol. 2013; 1:337–342.26. Smith JA Jr, Chan RC, Chang SS, Herrell SD, Clark PE, Baumgartner R, Cookson MS. A comparison of the incidence and location of positive surgical margins in robotic assisted laparoscopic radical prostatectomy and open retropubic radical prostatectomy. J Urol. 2007; 178:2385–2389.27. Rozet F, Jaffe J, Braud G, Harmon J, Cathelineau X, Barret E, Vallancien G. A direct comparison of robotic assisted versus pure laparoscopic radical prostatectomy: a single institution experience. J Urol. 2007; 178:478–482.28. Joniau S, Tosco L, Briganti A, Vanden Broeck T, Gontero P, Karnes RJ, Spahn M, Van Poppel H. European Multicenter Prostate Cancer Clinical and Translational research group. Results of surgery for high-risk prostate cancer. Curr Opin Urol. 2013; 23:342–348.29. Tewari AK, Patel ND, Leung RA, Yadav R, Vaughan ED, El-Douaihy Y, Tu JJ, Amin MB, Akhtar M, Burns M, et al. Visual cues as a surrogate for tactile feedback during robotic-assisted laparoscopic prostatectomy: posterolateral margin rates in 1340 consecutive patients. BJU Int. 2010; 106:528–536.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radical Prostatectomy
- A Case of No Residual Cancer in Radical Prostatectomy Specimens Despite Biopsy-proven Prostate Cancer
- Predictors of Biochemical Failure after Radical Perineal Prostatectomy for Localized Prostate Cancer
- Review the Treatment Outcome in the Adenocarcinoma of the Prostate
- Comparison of biochemical recurrence in prostate cancer patients treated with radical prostatectomy or radiotherapy