Ann Surg Treat Res.
2016 Sep;91(3):112-117. 10.4174/astr.2016.91.3.112.
A comparison between two methods for tumor localization during totally laparoscopic distal gastrectomy in patients with gastric cancer
- Affiliations
-
- 1Department of Surgery, Korea University Medical Center, Korea University College of Medicine, Seoul, Korea. ppongttai@gmail.com
- KMID: 2350537
- DOI: http://doi.org/10.4174/astr.2016.91.3.112
Abstract
- PURPOSE
The aim of this study was to compare two methods of tumor localization during totally laparoscopic distal gastrectomy (TLDG) in patients with gastric cancer.
METHODS
From March 2014 to November 2014, patients in whom TLDG had been engaged for middle third gastric cancer enrolled in this study. The patients were allocated to either the radiography or endoscopy group based on the type of tumor localization technique. Clinicopathologic outcomes were compared between the 2 groups.
RESULTS
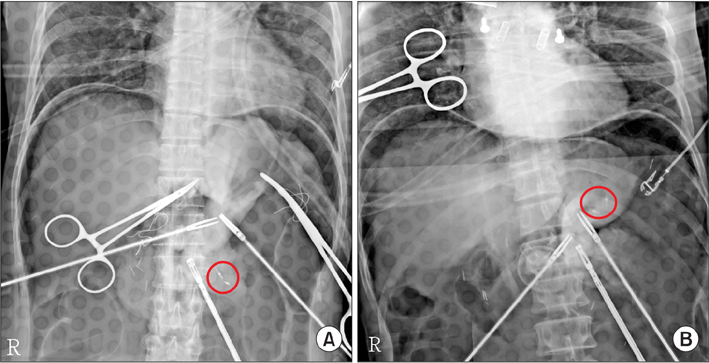
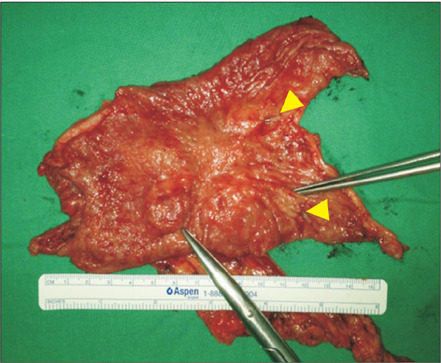
The accrual was suspended in November 2014 when 39 patients had been enrolled because a failed localization happened in the radiography group. The radiography and endoscopy groups included 17 (43.6 %) and 22 patients (56.4 %), respectively. Mean length of the proximal resection margin did not differ between the radiography and endoscopy groups (4.0 ± 2.6 and 2.8 ± 1.2 cm, respectively; P = 0.077). Mean localization time was longer in the radiography group than in the endoscopy group (22.7 ± 11.4 and 6.9 ± 1.8 minutes, respectively, P < 0.001). There were no statistically significant differences in the incidence of severe complications between the 2 groups (5.9% and 4.5%, respectively, P = 0.851).
CONCLUSION
As an intraoperative tumor localization for TLDG, radiologic method was unsafe even though other comparable parameters were not different from that of endoscopy group. Moreover, intraoperative endoscopic localization may be advantageous because it is highly accurate and contributes to reducing operation time.
Keyword
Figure
Reference
-
1. Jeong O, Park YK. Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer. 2011; 11:69–77.2. Hochwald SN, Brennan MF, Klimstra DS, Kim S, Karpeh MS. Is lymphadenectomy necessary for early gastric cancer? Ann Surg Oncol. 1999; 6:664–670.3. Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994; 4:146–148.4. Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, et al. Long-term results of laparoscopic gastrectomy for gastric cancer: a large-scale case-control and case-matched Korean multicenter study. J Clin Oncol. 2014; 32:627–633.5. Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N, Taomoto J, Masuda T, et al. Advantages of totally laparoscopic distal gastrectomy over laparoscopically assisted distal gastrectomy for gastric cancer. Surg Endosc. 2009; 23:2374–2379.6. Oki E, Sakaguchi Y, Ohgaki K, Saeki H, Chinen Y, Minami K, et al. The impact of obesity on the use of a totally laparoscopic distal gastrectomy in patients with gastric cancer. J Gastric Cancer. 2012; 12:108–112.7. Kim MG, Kawada H, Kim BS, Kim TH, Kim KC, Yook JH, et al. A totally laparoscopic distal gastrectomy with gastroduodenostomy (TLDG) for improvement of the early surgical outcomes in high BMI patients. Surg Endosc. 2011; 25:1076–1082.8. Kim MG, Kim KC, Kim BS, Kim TH, Kim HS, Yook JH, et al. A totally laparoscopic distal gastrectomy can be an effective way of performing laparoscopic gastrectomy in obese patients (body mass index≥30). World J Surg. 2011; 35:1327–1332.9. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112.10. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.11. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196.12. Ohdaira T, Nagai H. Intraoperative localization of early-stage upper gastrointestinal tumors using a magnetic marking clip-detecting system. Surg Endosc. 2007; 21:810–815.13. Kim HI, Hyung WJ, Lee CR, Lim JS, An JY, Cheong JH, et al. Intraoperative portable abdominal radiograph for tumor localization: a simple and accurate method for laparoscopic gastrectomy. Surg Endosc. 2011; 25:958–963.14. Jeong O, Cho SB, Joo YE, Ryu SY, Park YK. Novel technique for intraoperative tumor localization during totally laparoscopic distal gastrectomy: endoscopic autologous blood tattooing. Surg Endosc. 2012; 26:1778–1783.15. Xuan Y, Hur H, Byun CS, Han SU, Cho YK. Efficacy of intraoperative gastroscopy for tumor localization in totally laparoscopic distal gastrectomy for cancer in the middle third of the stomach. Surg Endosc. 2013; 27:4364–4370.16. Jeong SH, Bae K, Ha CY, Lee YJ, Lee OJ, Jung WT, et al. Effectiveness of endoscopic clipping and computed tomography gastroscopy for the preoperative localization of gastric cancer. J Korean Surg Soc. 2013; 84:80–87.17. Zubarik R, Eisen G, Mastropietro C, Lopez J, Carroll J, Benjamin S, et al. Prospective analysis of complications 30 days after outpatient upper endoscopy. Am J Gastroenterol. 1999; 94:1539–1545.18. Kavic SM, Basson MD. Complications of endoscopy. Am J Surg. 2001; 181:319–332.19. Geraci G, Pisello F, Modica G, Li Volsi F, Arnone E, Sciume C. Complications of elective esophago-gastro-duodenoscopy (EGDS). Personal experience and literature review. G Chir. 2009; 30:502–506.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Comparison of Laparoscopy-Assisted and Totally Laparoscopic Distal Gastrectomy: The Short-Term Outcome at a Low Volume Center
- Comparison of laparoscopy-assisted and totally laparoscopic Billroth-II distal gastrectomy for gastric cancer
- Totally Laparoscopic Distal Gastrectomy after Learning Curve Completion: Comparison with Laparoscopy-Assisted Distal Gastrectomy
- Corrigendum: Comparison of Short-Term Postoperative Outcomes in Totally Laparoscopic Distal Gastrectomy Versus Laparoscopy-Assisted Distal Gastrectomy