Korean J Gastroenterol.
2016 Aug;68(2):109-113. 10.4166/kjg.2016.68.2.109.
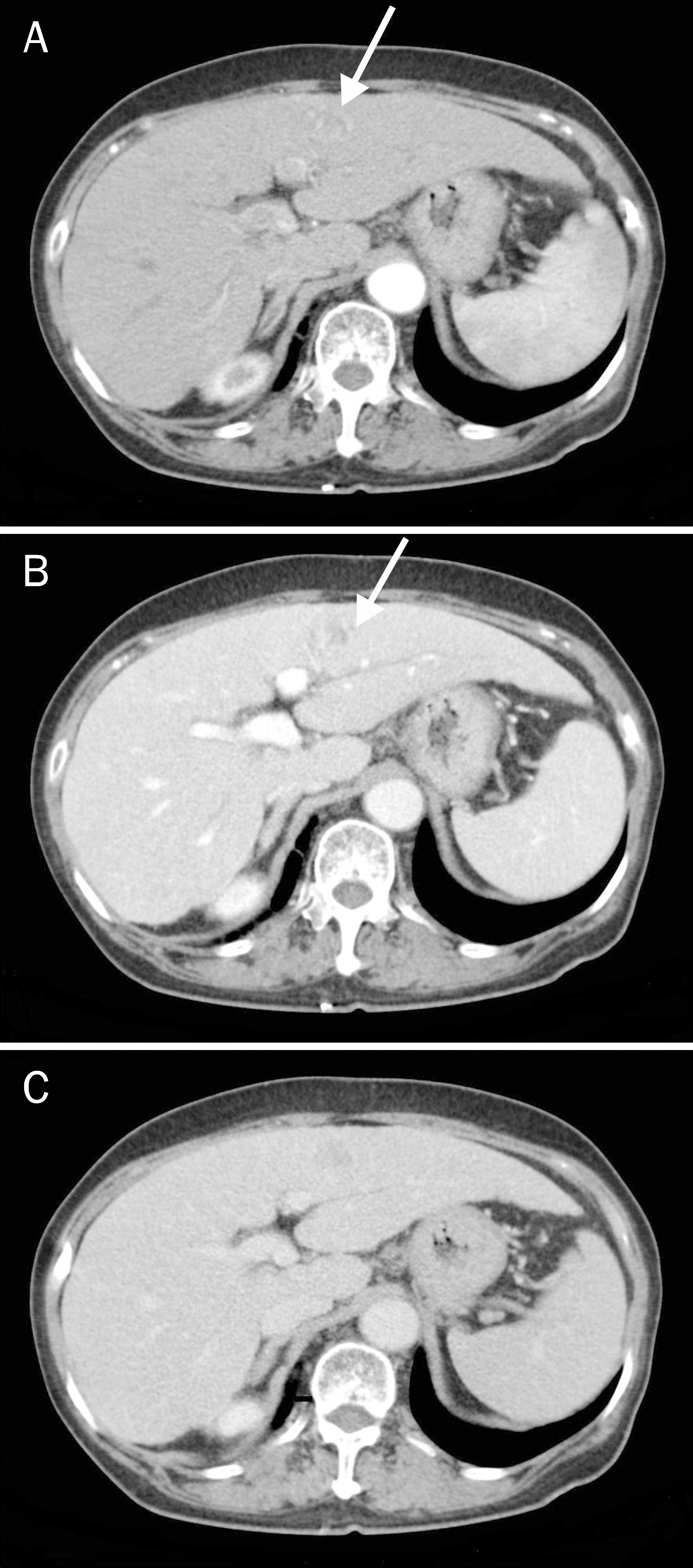
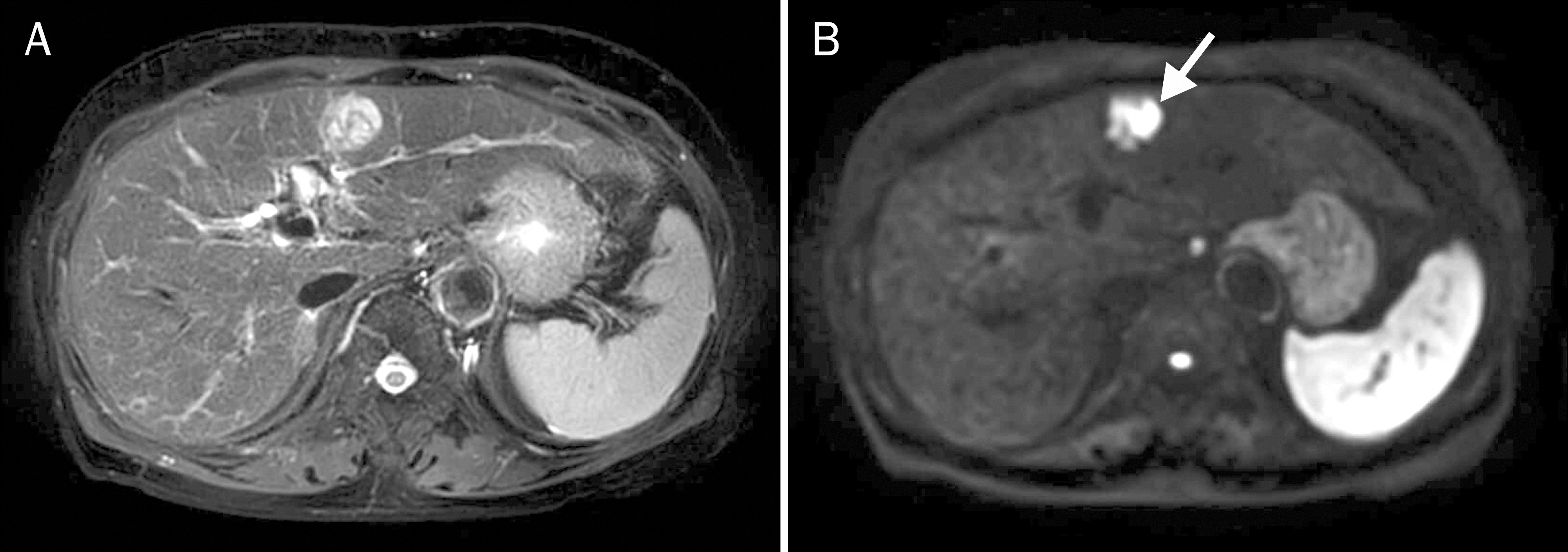
A Case of Composite Hepatocellular Carcinoma and Neuroendocrine Carcinoma in a Patient with Liver Cirrhosis Caused by Chronic Hepatitis B
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University School of Medicine, Jinju, Korea. kimthy@gnu.ac.kr
- 2Department of Pathology, Gyeongsang National University School of Medicine, Jinju, Korea.
- 3Institute of Health Sciences, Gyeongsang National University School of Medicine, Jinju, Korea.
- KMID: 2350089
- DOI: http://doi.org/10.4166/kjg.2016.68.2.109
Abstract
- Primary hepatic neuroendocrine carcinoma (PHNEC) is rare and its origin is not clearly understood. The coexistence of PHNEC and hepaotcellular carcinoma has been reported in only a few cases. We report a rare case of combined PHNEC and hepaotcellular carcinoma in a patient with liver cirrhosis caused by chronic hepatitis B that resulted in aggressive behavior and poor prognosis.
MeSH Terms
Figure
Reference
-
References
1. Barsky SH, Linnoila I, Triche TJ, Costa J. Hepatocellular carcinoma with carcinoid features. Hum Pathol. 1984; 15:892–894.
Article2. Artopoulos JG, Destuni C. Primary mixed hepatocellular carcinoma with carcinoid characteristics. A case report. Hepatogastroenterology. 1994; 41:442–444.3. Tajima Y, Nakajima T, Sugano I, Nagao K, Kondo Y, Saito J. Hepatocellular carcinoma containing endocrine cells. An autopsy report of triplecancer involving the liver, kidney and thyroid. Acta Pathol Jpn. 1992; 42:904–910.4. Wang JH, Dhillon AP, Sankey EA, Wightman AK, Lewin JF, Scheuer PJ. 'Neuroendocrine' differentiation in primary neoplasms of the liver. J Pathol. 1991; 163:61–67.
Article5. Zhao M, Laissue JA, Zimmermann A. "Neuroendocrine" differentiation in hepatocellular carcinomas (HCCs): immunohistochemical reactivity is related to distinct tumor cell types, but not to tumor grade. Histol Histopathol. 1993; 8:617–626.6. Pilichowska M, Kimura N, Ouchi A, Lin H, Mizuno Y, Nagura H. Primary hepatic carcinoid and neuroendocrine carcinoma: clinicopathological and immunohistochemical study of five cases. Pathol Int. 1999; 49:318–324.
Article7. Kaya G, Pasche C, Osterheld MC, Chaubert P, Fontolliet C. Primary neuroendocrine carcinoma of the liver: an autopsy case. Pathol Int. 2001; 51:874–878.
Article8. Ishida M, Seki K, Tatsuzawa A, et al. Primary hepatic neuroendocrine carcinoma coexisting with hepatocellular carcinoma in hepatitis C liver cirrhosis: report of a case. Surg Today. 2003; 33:214–218.
Article9. Yamaguchi R, Nakashima O, Ogata T, Hanada K, Kumabe T, Kojiro M. Hepatocellular carcinoma with an unusual neuroendocrine component. Pathol Int. 2004; 54:861–865.
Article10. Garcia MT, Bejarano PA, Yssa M, Buitrago E, Livingstone A. Tumor of the liver (hepatocellular and high grade neuroendocrine carcinoma): a case report and review of the literature. Virchows Arch. 2006; 449:376–381.
Article11. Gould VE, Banner BF, Baerwaldt M. Neuroendocrine neoplasms in unusual primary sites. Diagn Histopathol. 1981; 4:263–277.12. Hsu W, Deziel DJ, Gould VE, Warren WH, Gooch GT, Staren ED. Neuroendocrine differentiation and prognosis of extrahepatic biliary tract carcinomas. Surgery. 1991; 110:604–610. discussion 610–611.13. Cheon JH, Park JW, Park KW, et al. The clinical report of 1,078 cases of hepatocellular carcinomas: National Cancer Center experience. Korean J Hepatol. 2004; 10:288–297.14. Fenoglio LM, Severini S, Ferrigno D, et al. Primary hepatic carcinoid: a case report and literature review. World J Gastroenterol. 2009; 15:2418–2422.
Article15. Park SH, Kang MJ, Cho JH, et al. Hepatocellular carcinoma with neuroendocrine differentiation: clinical and imaging findings in five patients. J Korean Radiol Soc. 2008; 58:65–71.
Article16. Bader TR, Semelka RC, Chiu VC, Armao DM, Woosley JT. MRI of carcinoid tumors: spectrum of appearances in the gastrointestinal tract and liver. J Magn Reson Imaging. 2001; 14:261–269.
Article17. Krohn M, Grieser C, Weichert W, Pascher A, Denecke T. Well-differentiated neuroendocrine carcinoma mimicking an echino-coccus cyst of the liver in CT-MRI findings with hepatocyte specific contrast material. J Gastrointestin Liver Dis. 2011; 20:439–442.18. Shetty PK, Baliga SV, Balaiah K, Gnana PS. Primary hepatic neuroendocrine tumor: an unusual cystic presentation. Indian J Pathol Microbiol. 2010; 53:760–762.
Article19. Ramage JK, Ahmed A, Ardill J, et al. Guidelines for the management of gastroenteropancreatic neuroendocrine (including carcinoid) tumours (NETs). Gut. 2012; 61:6–32.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Who Needs Screening for the Early Detection of Hepatocellular Carcinoma ?
- A Case of Early Multiply Recurred Hepatocellular Carcinoma after Surgical Resection in Patient Who Unprecedented Chronic Liver Disease
- Hepatitis C virus antibodies in patients with hepatocellular carcinoma and liver cirrhosis
- Dynamic expressions of proto-oncogenes in chronic hepatitis, liver cirrhosis and hepatocellular carcinoma
- Management of viral hepatitis in patients with hepatocellular carcinoma