J Korean Soc Radiol.
2010 Oct;63(4):359-364.
Evaluation of the Optimal Site for Retrograde Common Femoral Arterial Puncture
- Affiliations
-
- 1Department of Radiology, Gachon University Gil Hospital, Korea. ho7ok7@gilhospital.com
Abstract
- PURPOSE
To determine the optimal skin site for retrograde common femoral arterial puncture based on the inguinal skin crease.
MATERIALS AND METHODS
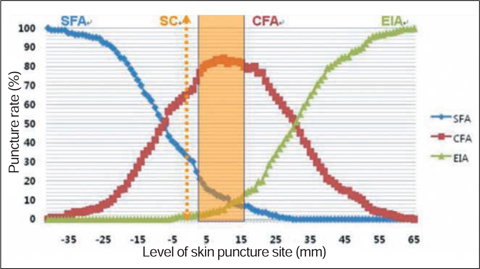
We retrospectively evaluated CT arteriographic images of right groins in 200 patients. We measured the relative distances of the common femoral artery bifurcation and inguinal ligament from the inguinal skin crease, respectively. We calculated the rates of common femoral artery puncture at 1 mm intervals, above or below the inguinal skin crease.
RESULTS
The range in skin site where the rates of common femoral artery puncture were greater than 60%, 70%, and 80% were situated between 3 mm below to 27 mm above, 1 mm to 23 mm above, and 5 mm to 15 mm above the inguinal skin crease, respectively. The skin site of the highest puncture rate was 10 mm above inguinal skin crease (85.2%).
CONCLUSION
The optimal skin site for retrograde common femoral artery puncture was above the inguinal skin crease, most optimally at 10 mm above the inguinal skin crease.
MeSH Terms
Figure
Reference
-
1. Millward SF, Burbridge BE, Luna G. Puncturing the pulseless femoral artery: a simple technique that uses palpation of anatomic landmarks. J Vasc Interv Radiol. 1993; 4:415–417.2. Grier D, Hartnell G. Percutaneous femoral artery puncture: practice and anatomy. Br J Radiol. 1990; 63:602–604.3. Dotter CT, Rosch J, Robinson M. Fluoroscopic guidance in femoral artery puncture. Radiology. 1978; 127:266–267.4. Garrett PD, Eckart RE, Bauch TD, Thompson CM, Stajduhar KC. Fluoroscopic localization of the femoral head as a landmark for common femoral artery cannulation. Catheter Cardiovasc Interv. 2005; 65:205–207.5. Lechner G, Jantsch H, Waneck R, Kretschmer G. The relationship between the common femoral artery, the inguinal crease, and the inguinal ligament: a guide to accurate angiographic puncture. Cardiovasc Intervent Radiol. 1988; 11:165–169.6. Schnyder G, Sawhney N, Whisenant B, Tsimikas S, Turi ZG. Common femoral artery anatomy is influenced by demographics and comorbidity: implications for cardiac and peripheral invasive studies. Catheter Cardiovasc Interv. 2001; 53:289–295.7. Grossman M. How to miss the profunda femoris. Radiology. 1974; 111:482.8. Yeow KM, Toh CH, Wu CH, Lee RY, Hsieh HC, Liau CT, et al. Sonographically guided antegrade common femoral artery access. J Ultrasound Med. 2002; 21:1413–1416.9. Hessel SJ, Adams DF, Abrams HL. Complications of angiography. Radiology. 1981; 138:273–281.10. Rapoport S, Sniderman KW, Morse SS, Proto MH, Ross GR. Pseudoaneurysm: a complication of faulty technique in femoral arterial puncture. Radiology. 1985; 154:529–530.11. Illescas FF, Baker ME, McCann R, Cohan RH, Silverman PM, Dunnick NR. CT evaluation of retroperitoneal hemorrhage associated with femoral arteriography. AJR Am J Roentgenol. 1986; 146:1289–1292.12. Rupp SB, Vogelzang RL, Nemcek AA Jr, Yungbluth MM. Relationship of the inguinal ligament to pelvic radiographic landmarks: anatomic correlation and its role in femoral arteriography. J Vasc Interv Radiol. 1993; 4:409–441.13. Spector KS, Lawson WE. Optimizing safe femoral access during cardiac catheterization. Catheter Cardiovasc Interv. 2001; 53:209–212.14. Chung HH, Ha JS, Cha SH, Kim BH, Lee KY, Kim TK, Lee SH, Kim JH, Seol HY. Femoral Arterial Puncture: Comparison of Using the Inguinal Crease and Bony Landmarks. J Korean Radiol Soc. 2006; 54:251–257.15. Jeon MH, Han GS, Kim SJ, Park KS, Cha SH, Bae IH, Lee SY. Anatomic Landmarks of Fluoroscopy Guided Puncture of the Pulseless Femoral Artery. J Korean Radiol Soc. 2006; 55:53–57.16. Spijkerboer AM, Scholten FG, Mali WP, van Schaik JP. Antegrade puncture of the femoral artery: morphologic study. Radiology. 1990; 176:57–60.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Femoral Arterial Puncture: Comparison of Using the Inguinal Crease and Bony Landmarks
- Ultrasonographic evaluation of complications related to transfemoral arterial procedures
- Pseudoaneurysm Leading to Necrotizing Fasciitis at the Femoral Arterial Puncture Site
- Assessment of the Optimal Site of Femoral Artery Puncture and Angiographic Anatomical Study of the Common Femoral Artery
- Safety and Effectiveness of a Circumferential Clip-Based Vascular Closure Device for Hemostasis in Off-Label Applications: Comparison with Standard Applications