J Korean Soc Radiol.
2016 Aug;75(2):157-161. 10.3348/jksr.2016.75.2.157.
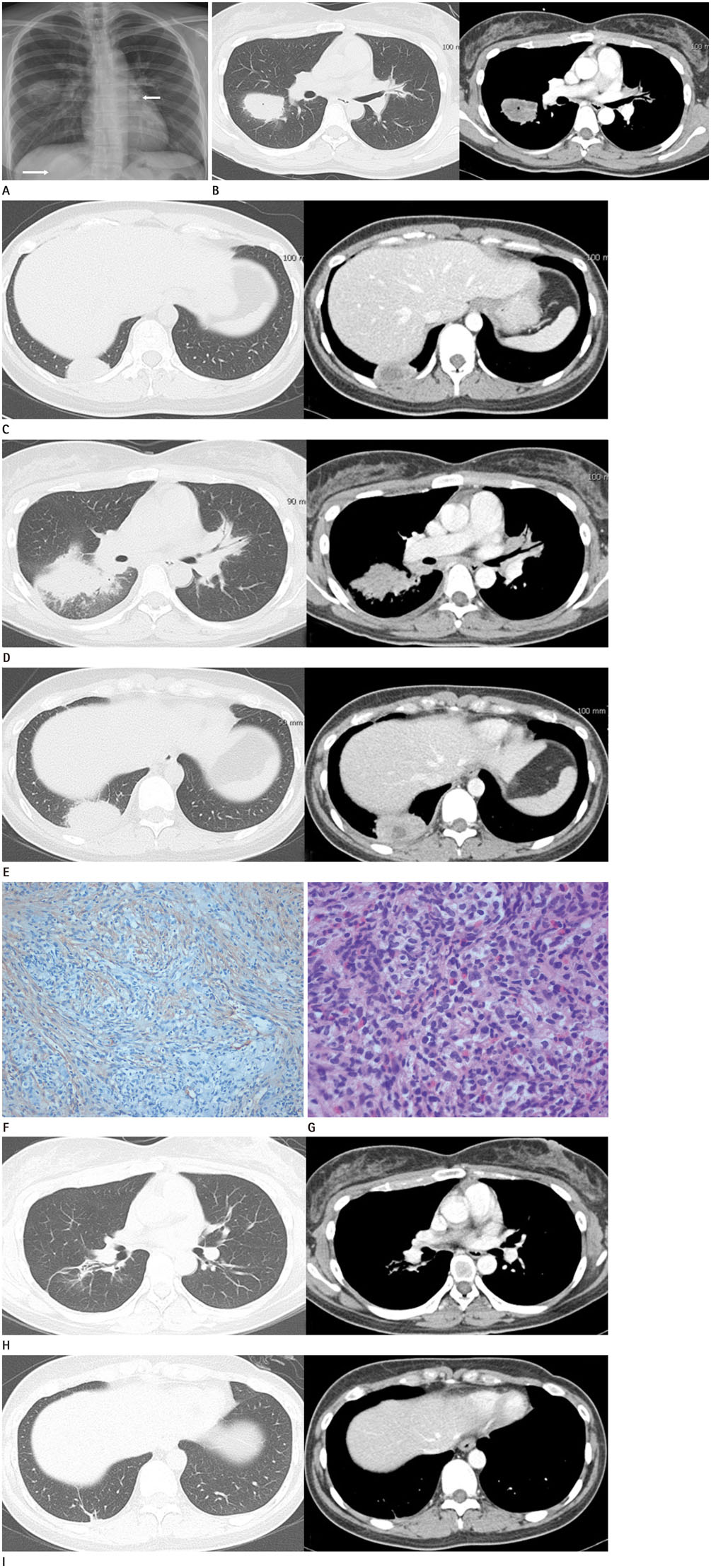
Aggressive and Multifocal Pulmonary Inflammatory Myofibroblastic Tumor in Young Woman
- Affiliations
-
- 1Department of Radiology, Bucheon St. Mary's Hospital, The Catholic University of Korea, Bucheon, Korea. mhchung@catholic.ac.kr
- 2Division of Allergy and Pulmonary, Department of Internal Medicine, Bucheon St. Mary's Hospital, The Catholic University of Korea, Bucheon, Korea.
- 3Department of Hospital Pathology, Bucheon St. Mary's Hospital, The Catholic University of Korea, Bucheon, Korea.
- KMID: 2344808
- DOI: http://doi.org/10.3348/jksr.2016.75.2.157
Abstract
- We report a case of pulmonary inflammatory myofibroblastic tumor (IMT) showing aggressive and unusually rapid progression. A 27-year-old woman was admitted to the emergency room due to dry cough, fever and blood-tinged sputum that lasted one week. Initial chest radiograph and computed tomography scan revealed multifocal pulmonary nodules, which subsequently progressed into large necrotic masses within two months. She underwent a fine needle biopsy of the largest mass in the right middle lung zone which revealed inflammatory myofibroblastic cells consistent with IMT. The masses showed complete regression after six months of corticosteroid therapy. This unusual clinical manifestation could help explain the reactive inflammatory nature associated with IMTs.
MeSH Terms
Figure
Reference
-
1. Coffin CM, Watterson J, Priest JR, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol. 1995; 19:859–872.2. Agrons GA, Rosado-de-Christenson ML, Kirejczyk WM, Conran RM, Stocker JT. Pulmonary inflammatory pseudotumor: radiologic features. Radiology. 1998; 206:511–518.3. Iczkowski KA, Shanks JH, Gadaleanu V, Cheng L, Jones EC, Neumann R, et al. Inflammatory pseudotumor and sarcoma of urinary bladder: differential diagnosis and outcome in thirty-eight spindle cell neoplasms. Mod Pathol. 2001; 14:1043–1051.4. Patnana M, Sevrukov AB, Elsayes KM, Viswanathan C, Lubner M, Menias CO. Inflammatory pseudotumor: the great mimicker. AJR Am J Roentgenol. 2012; 198:W217–W227.5. Patankar T, Prasad S, Shenoy A, Rathod K. Pulmonary inflammatory pseudotumour in children. Australas Radiol. 2000; 44:318–320.6. Hedlund GL, Navoy JF, Galliani CA, Johnson WH Jr. Aggressive manifestations of inflammatory pulmonary pseudotumor in children. Pediatr Radiol. 1999; 29:112–116.7. Kato S, Kondo K, Teramoto T, Harada T, Ikeda H, Hara K, et al. A case report of inflammatory pseudotumor of the lung: rapid recurrence appearing as multiple lung nodules. Ann Thorac Cardiovasc Surg. 2002; 8:224–227.8. Coffin CM, Hornick JL, Fletcher CD. Inflammatory myofibroblastic tumor: comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive cases. Am J Surg Pathol. 2007; 31:509–520.9. Matsubara O, Tan-Liu NS, Kenney RM, Mark EJ. Inflammatory pseudotumors of the lung: progression from organizing pneumonia to fibrous histiocytoma or to plasma cell granuloma in 32 cases. Hum Pathol. 1988; 19:807–814.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inflammatory Myofibroblastic Tumor (InflammatoryFibrosarcoma) of the Lung: A Case Report
- Inflammatory Myofibroblastic Tumor of Nasal Septum after Septoplasty: A Case Report
- Inflammatory Myofibroblastic Tumor of Kidney
- Aggressive Pulmonary Inflammatory Myofibroblastic Tumor with Chest Wall Invasion: A Case Report
- Pulmonary Inflammatory Myofibroblastic Tumor with Bronchus Invasion: One case report