Korean Circ J.
2016 Mar;46(2):147-153. 10.4070/kcj.2016.46.2.147.
Rosuvastatin Reduces Blood Viscosity in Patients with Acute Coronary Syndrome
- Affiliations
-
- 1Division of Cardiology, Chonbuk National University Hospital and Chonbuk National University Medical School, Jeonju, Korea. medorche@jbnu.ac.kr
- 2Division of Mechanical Design Engineering, Chonbuk National University, Jeonju, Korea.
- 3Department of Laboratory Medicine, Chonbuk National University Hospital and Chonbuk National University Medical School, Jeonju, Korea.
- KMID: 2344465
- DOI: http://doi.org/10.4070/kcj.2016.46.2.147
Abstract
- BACKGROUND AND OBJECTIVES
Wall shear stress contributes to atherosclerosis progression and plaque rupture. There are limited studies for statin as a major contributing factor on whole blood viscosity (WBV) in patients with acute coronary syndrome (ACS). This study investigates the effect of statin on WBV in ACS patients.
SUBJECTS AND METHODS
We prospectively enrolled 189 consecutive patients (mean age, 61.3±10.9 years; 132 males; ST-segment elevation myocardial infarction, n=52; non-ST-segment elevation myocardial infarction, n=84; unstable angina n=53). Patients were divided into two groups (group I: previous use of statins for at least 3 months, n=51; group II: statin-naïve patients, n=138). Blood viscosities at shear rates of 1 s-1 (diastolic blood viscosity; DBV) and 300 s-1 (systolic blood viscosity; SBV) were measured at baseline and one month after statin treatment. Rosuvastatin was administered to patients after enrollment (mean daily dose, 16.2±4.9 mg).
RESULTS
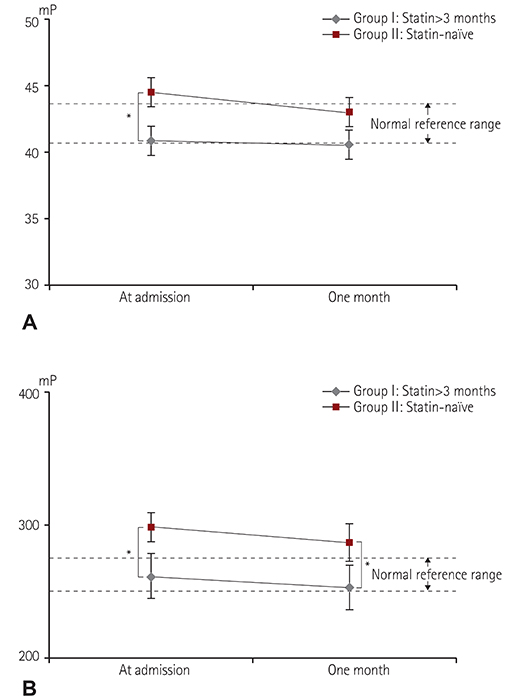
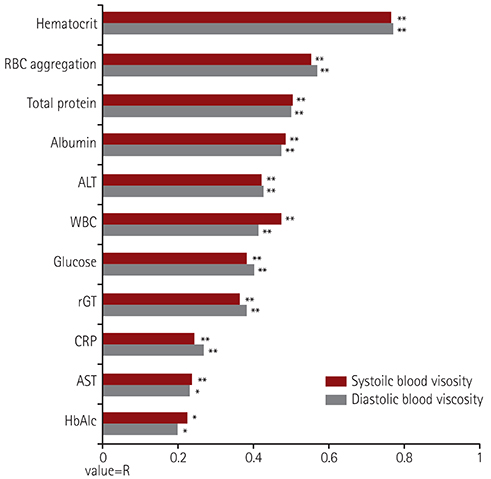
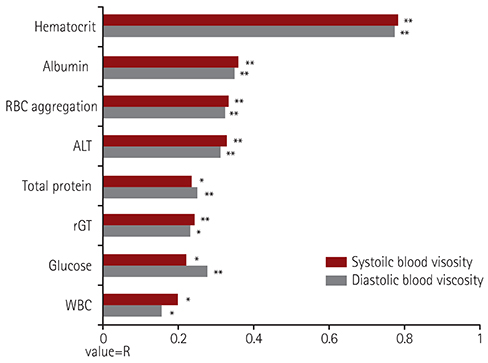
Baseline WBV was significantly higher in group II ([SBV: group I vs group II, 40.8±5.9 mP vs. 44.2±7.4 mP, p=0.003], [DBV: 262.2±67.8 mP vs. 296.9±76.0 mP, p=0.002]). WBV in group II was significantly lower one month after statin treatment ([SBV: 42.0±4.7 mP, p=0.012, DBV: 281.4±52.6 mP, p=0.044]). However, low-density lipoprotein cholesterol level was not associated with WBV in both baseline (SBV: R2=0.074, p=0.326; DBV: R2=0.073, p=0.337) and after one month follow up (SBV: R2=0.104, p=0.265; DBV: R2=0.112, p=0.232).
CONCLUSION
Previous statin medication is an important determinant in lowering WBV in patients with ACS. However, one month of rosuvastatin decreased WBV in statin-naïve ACS patients.
MeSH Terms
Figure
Cited by 2 articles
-
Prior antithrombotic use is significantly associated with decreased blood viscosity within 24 hours of symptom onset in patients with acute ischemic stroke
Joong Hyun Park, Jeong Yeon Kim, Jong Sam Baik, Jae Hyeon Park, Hyo Suk Nam, Sang Won Han
J Neurocrit Care. 2019;12(2):85-91. doi: 10.18700/jnc.190092.The good genotype for clopidogrel metabolism is associated with decreased blood viscosity in clopidogrel-treated ischemic stroke patients
Joong Hyun Park, Sang Won Han, Hyun-Jeung Yu
J Neurocrit Care. 2020;13(2):93-100. doi: 10.18700/jnc.200023.
Reference
-
1. Arbab-Zadeh A, Nakano M, Virmani R, Fuster V. Acute coronary events. Circulation. 2012; 125:1147–1156.2. Kensey KR. The mechanistic relationships between hemorheological characteristics and cardiovascular disease. Curr Med Res Opin. 2003; 19:587–596.3. Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006; 47:8 Suppl. C13–C18.4. Finn AV, Nakano M, Narula J, Kolodgie FD, Virmani R. Concept of vulnerable/unstable plaque. Arterioscler Thromb Vasc Biol. 2010; 30:1282–1292.5. Marton Z, Horvath B, Alexy T, et al. Follow-up of hemorheological parameters and platelet aggregation in patients with acute coronary syndromes. Clin Hemorheol Microcirc. 2003; 29:81–94.6. Cho YI, Kensey KR. Effects of the non-Newtonian viscosity of blood on flows in a diseased arterial vessel. Part 1: steady flows. Biorheology. 1991; 28:241–262.7. Fuchs J, Pinhas A, Davidson E, Rotenberg Z, Agmon J, Weinberger I. Plasma viscosity, fibrinogen and haematocrit in the course of unstable angina. Eur Heart J. 1990; 11:1029–1032.8. Cho YI, Cho DJ. Hemorheology and microvascular disorders. Korean Circ J. 2011; 41:287–295.9. Lipowsky HH. Microvascular rheology and hemodynamics. Microcirculation. 2005; 12:5–15.10. Lee AJ, Mowbray PI, Lowe GD, Rumley A, Fowkes FG, Allan PL. Blood viscosity and elevated carotid intima-media thickness in men and women: the Edinburgh Artery Study. Circulation. 1998; 97:1467–1473.11. Lee SR, Jung JM, Jung LY, et al. Elevated coronary whole blood viscosity in acute coronary syndrome patients. Clin Hemorheol Microcirc. 2013; 55:85–94.12. Sezer M, Oflaz H, Gören T, et al. Intracoronary streptokinase after primary percutaneous coronary intervention. N Engl J Med. 2007; 356:1823–1834.13. Moriarty PM, Gibson CA, Kensey KR, Hogenauer W. Effect of lowdensity lipoprotein cholesterol apheresis on blood viscosity. Am J Cardiol. 2004; 93:1044–1046.14. Rosenson RS, Tangney CC. Antiatherothrombotic properties of statins: implications for cardiovascular event reduction. JAMA. 1998; 279:1643–1650.15. Vaughan CJ, Murphy MB, Buckley BM. Statins do more than just lower cholesterol. Lancet. 1996; 348:1079–1082.16. Beigel Y, Fuchs J, Snir M, Green P, Lurie Y, Djaldetti M. Lovastatin therapy in hypercholesterolemia: effect on fibrinogen, hemorrheologic parameters, platelet activity, and red blood cell morphology. J Clin Pharmacol. 1991; 31:512–517.17. Jay RH, Rampling MW, Betteridge DJ. Abnormalities of blood rheology in familial hypercholesterolaemia: effects of treatment. Atherosclerosis. 1990; 85:249–256.18. Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischemic heart disease, and stroke: systemic review and meta-analysis. BMJ. 2003; 326:1423.19. Kim H, Cho YI, Lee DH, et al. Analytical performance evaluation of the scanning capillary tube viscometer for measurement of whole blood viscosity. Clin Biochem. 2013; 46:139–142.20. Shin S, Hou JX, Suh JS, Singh M. Validation and application of a microfluidic ektacytometer (RheoScan-D) in measuring erythrocyte deformability. Clin Hemorheol Microcirc. 2007; 37:319–328.21. Holsworth RE Jr, Cho YI, Weidman JJ, Sloop GD, St Cyr JA. Cardiovascular benefits of phlebotomy: relationship to changes in hemorheological variables. Perfusion. 2014; 29:102–116.22. Rosenson RS, Wolff D, Green D, Boss AH, Kensey KR. Aspirin . Aspirin dose not alter native blood viscosity. J Thromb Haemost. 2004; 2:340–341.23. Froom P. Blood viscosity and the risk of death from coronary heart disease. Eur Heart J. 2000; 21:513–514.24. Jung JM, Lee DH, Kim KT, et al. Reference intervals for whole blood viscosity using the analytical performance-evaluated scanning capillary tube viscometer. Clin Biochem. 2014; 47:489–493.25. Banyai S, Banyai M, Falger J, et al. Atorvastatin improves blood rheology in patients with familial hypercholesterolemia (FH) on long-term LDL apheresis treatment. Atherosclerosis. 2001; 159:513–519.26. Bo M, Bonino F, Neirotti M, et al. Hemorheologic and coagulative pattern in hypercholesterolemic subjects treated with lipid-lowering drugs. Angiology. 1991; 42:106–113.27. Ditzel J, Kampmann J. Whole-blood viscosity, hematocrit and plasma protein in normal subjects at different ages. Acta Physiol Scand. 1971; 81:264–268.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antithrombotic Therapy for Elderly Patients with Acute Coronary Syndrome
- Effect of High Dose Rosuvastatin Loading before Primary Percutaneous Coronary Intervention on Infarct Size in Patients with ST-Segment Elevation Myocardial Infarction
- Rosuvastatin-induced Generalized Drug Eruption
- Effect of Physical Vibration on Blood Viscosity
- Spontaneous Coronary Artery Dissection in a female patient with fragile X syndrome